Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8284
Peer-review started: September 22, 2023
First decision: October 9, 2023
Revised: October 12, 2023
Accepted: December 4, 2023
Article in press: December 4, 2023
Published online: December 16, 2023
Processing time: 83 Days and 2.3 Hours
Bronchiolitis is a common lower respiratory tract infection in infants and young children. Severe cases may be accompanied by obvious dyspnea and oxygen saturation decline.
To summarize the clinical features, standard diagnosis, and treatment of bronchiolitis.
This is a retrospective analysis of 114 pediatric patients (74 males, 40 females) who were first diagnosed as having bronchioles at the Department of Pediatrics of Tongling Maternal and Child Health Hospital from January 2019 to December 2019. The clinical features, imaging features, treatment, and other clinical data were recorded and analyzed.
The age of onset of the disease was mainly from 1 mo to 6 mo (75.4%), and the time to hospital visit was mostly from the 2nd day to the 4th day of the course of the disease (75.4%). Lung imaging examination showed increase in lung texture, fuzzy (93.8%). The main treatment was atomization therapy: Budesonide combined with terbutaline (45.6%) and budesonide combined with salbutamol (38.5%). The average hospitalization time was 7.1 ± 2.4 d, and the overall cure rate was 94.7%. In patients without bacterial infection, the use of antibiotics significantly prolonged the length of hospital stay (7.8 ± 2.5 d vs 5.7 ± 1.8 d) and improved the cure rate (98.3% vs 87.9%, P < 0.05).
Infants with bronchiolitis are mainly male and tend to have a good prognosis. However, the unneeded use of antibiotics may prolong the length of hospital stay significantly, which imposes the burden both on the patients and hospital system.
Core Tip: A retrospective analysis of the data of infants and young children with bronchiolitis showed that the disease had a male gender preference, the age of onset was relatively young, and the prognosis was good. Through comparative analysis of the use of antibiotics in infants and young children with bronchiolitis without bacterial infection, it was found that there was controversy over the abuse of antibiotics in the treatment of the disease. Increasing the use of antibiotics can improve the cure rate of patients, but it will prolong the length of hospital stay, and there is controversy over unreasonable use of medical resources.
- Citation: Shi C, Wu MH, Zuo A, Yang MM, Jiang RR. Clinical analysis of 114 cases of bronchiolitis in infants. World J Clin Cases 2023; 11(35): 8284-8290
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8284.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8284
In infants, bronchiolitis is one of the more common lower respiratory tract infection, its clinical manifestations mainly include cough, shortness of breath, and difficulty breathing, and lung auscultation may reveal wheezing sound and wet rales. Patients with severe bronchiolitis may have obvious dyspnea and oxygen saturation decline[1]. The peak age of its onset is 2-6 mo, and it is the main cause of hospitalization in children under 24 mo old[2]. At present, it is known that bronchiolitis is mainly caused by viral infection, the most common of which is respiratory syncytial virus[3], followed by adenovirus and influenza virus[4]. The main treatment measures were symptomatic and supportive treatment such as relieving cough and asthma and resolving phlegm[5]. The prognosis of children with this disease is mostly good, and a small number of children will develop into childhood asthma. Therefore, bronchiolitis should be actively prevented and treated to reduce the occurrence of asthma.
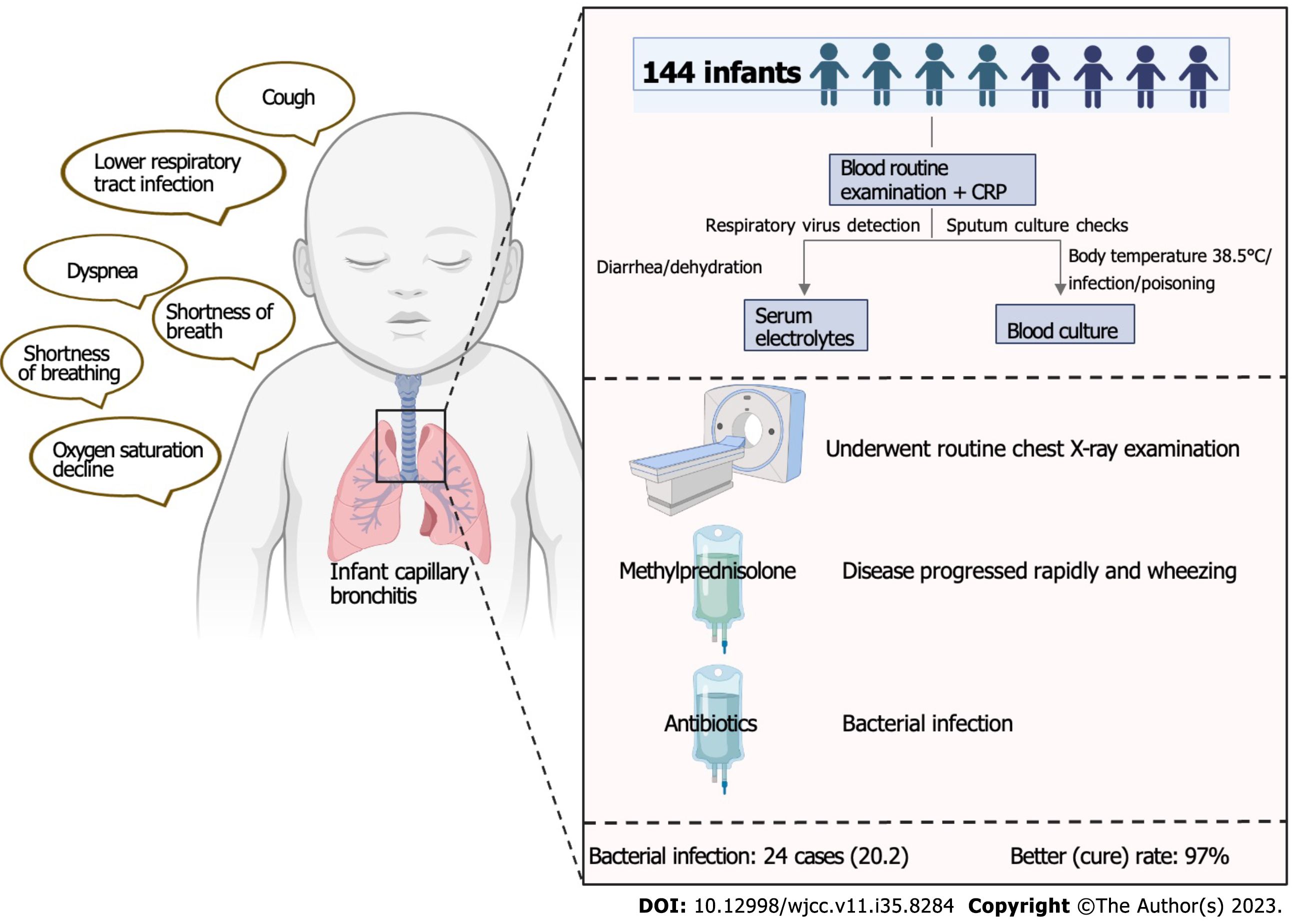
A total of 114 hospitalized children diagnosed with bronchiolitis at the Department of Pediatrics of Tongling Maternal and Child Health Care Hospital in the past year were retrospectively analyzed, and according to the treatment experience, the hospital's diagnosis and treatment standards for the disease were formulated to save medical costs. The main flowchart of the study is shown in Figure 1. This study was approved by the Medical Ethics Committee of Tongling Maternal and Child Health Hospital, and informed consent was obtained from the children's guardians.
The clinical data of 114 children hospitalized at Tongling Maternal and Child Health Hospital from January to December 2019 with the first diagnosis of bronchiolitis were collected. All the children met the diagnostic criteria for bronchiolitis. The diagnostic criteria were based on the 8th edition of "Zhufang Practical Pediatrics". Cases with missing data or incomplete primary data were excluded, and as a result, 18 patients were excluded from the study. The criteria for discharge included patients who were either cured or showed significant improvement, had stable vital signs, and exhibited clinical symptoms and signs that had returned to normal for more than 24 hours. Additionally, a review conducted before leaving the hospital confirmed that all infection indicators were normal.
All children underwent routine blood tests, examinations for hypersensitive C-reactive protein (CRP) and liver and kidney function, respiratory virus detection, and sputum culture checks. Children with the following conditions required further examination: (1) Serum electrolytes were measured when there were signs of diarrhea or dehydration; and (2) Blood culture was done when the body temperature was > 38.5 ℃ or there were symptoms of infection and poisoning. All children underwent pulmonary X-ray examination during their illness.
The following treatments were administered: (1) All hospitalized children were randomly treated with nebulized bronchodilator and/or β2 receptor agonist according to their condition; (2) Glucocorticoid atomization treatment was routinely used, and for severe cases, intravenous corticosteroids or intravenous immunoglobulin can be used; (3) Antibiotic treatment was given or not according to the results of the first blood routine test and CRP within 24 h before and after admission; and (4) Antiviral drugs were not used routinely.
SPSS19.0 software package was applied for statistical anlyses. Measurement data with a normal distribution are expressed as the mean ± SD, and the two independent samples t test was used for comparison. Count data are expressed as percentages (%) or rates, and the chi-square test was used for comparison. P < 0.05 was considered statistically significant.
As shown in Table 1, among the 114 children, 74 were male and 40 were femalewith a male to female ratio of about 1:0.54; 71 (62.3%) were born via natural delivery and 43 (37.7%) via cesarean section. The age of onset was mainly from 1 mo to 6 mo (93.9%), the time to visit the hospital was mostly 2-4 d (79.8%), the average length of hospital stay was (7.1 ± 2.4) d, and 23 cases (20.2%) were confirmed to have bacterial infection. In the study group, there were no deaths or serious complications. Six people were transferred, and the cure rate was 94.7%
| Basic information | |
| Gender, n (%) | |
| Male | 74 (64.9) |
| Female | 40 (35.1) |
| Onset age, n (%) | |
| 1-6 mo | 107 (93.9) |
| 6-12 mo | 7 (6.1) |
| Delivery, n (%) | |
| Natural labour | 71 (62.3) |
| Cesarean section | 43 (37.7) |
| Time to hospital visit (d), n (%) | |
| 2-4 | 91 (79.8) |
| 5-10 | 23 (20.2) |
| Length of stay (d) | 7.1 ± 2.4 |
| Co-infection with bacteria, n (%) | 23 (20.2) |
| Cure rate, n (%) | 108 (94.7) |
All children underwent routine chest X-ray examination. As shown in Table 2, of 107 cases (93.8%) showed thickened and blurred lung texture, and 7 (6.1%) were combined with patchy shadows. Wheezing was found in 47 cases (41.2%), pulmonary rales in 40 (35.1%), wet rales in 22 (19.3%), fever in 12 (10.5%), and perioral cyanosis in 3 (2.6%).
| Bronchiolitis | |
| Wheezing | 47 (41.2) |
| Fever | 12 (10.5) |
| Rhonchi | 40 (35.1) |
| Crackles | 22 (19.3) |
| Cyanosis | 3 (2.6) |
| Increased lung texture | 107 (93.8) |
| Patchy shadow | 7 (6.1) |
In terms of treatment measures, as shown in Table 3, of 81 children (41.2%) were treated with methylprednisolone when the disease progressed rapidly and wheezing was obvious. Fifty-two cases (45.6%) were treated with budesonide combined with terbutaline, 44 (38.5%) with budesonide combined with salbutamol, 81 (71.1%) with antibiotics, and 81 (71.1%) with interferon.
| Treatment | |
| Antibiotic treatment | 81 (71.1) |
| Hormone treatment | 47 (41.2) |
| Antiviral treatment | 81 (71.1) |
| Atomized medication | |
| Budesonide + terbutaline | 52 (45.6) |
| Budesonide + salbutamol | 44 (38.5) |
According to the results of the first routine blood test combined with CRP within 24 h before and after admission, the children were divided into children with clear bacterial infection (n = 23) and those with unknown infection status (n = 91). As shown in Table 4, of 23 children with clear bacterial infection were treated with antibiotics, while 58 children with unknown bacterial infection status were treated with antibiotics (63.7%); there was a significant difference between them (P < 0.05). Between the two groups, there were no significant differences in other drug treatments, length of hospital stay, or lung imaging examination results (P > 0.05).
| Bacterial infection (n = 23) | Unknown bacterial infection (n = 91) | t/χ2 | P value | |
| Antibiotic treatment, n (%) | 23 (100) | 58 (63.7) | 11.636 | 0.0001 |
| Hormone treatment, n (%) | 10 (43.5) | 35 (38.5) | 0.193 | 0.660 |
| Antiviral treatment, n (%) | 17 (73.9) | 64 (70.3) | 0.115 | 0.735 |
| Atomized medication, n (%) | 1.424 | 0.491 | ||
| Budesonide + terbutaline | 8 (34.8) | 44 (48.4) | ||
| Budesonide + salbutamol | 11 (47.8) | 33 (36.3) | ||
| Length of stay (d) | 7.3 ± 2.9 | 6.8 ± 2.3 | 0.959 | 0.735 |
| Increased lung texture, n (%) | 21 (91.3) | 86 (94.5) | 0.326 | 0.568 |
| Wheezing, n (%) | 11 (47.8) | 36 (39.6) | 0.518 | 0.472 |
According to whether antibiotics were used or not, the children with bronchiolitis without bacterial infection were divided into a antibiotic treatment group (n = 58) and a non-antibiotic treatment group (n = 33). As shown in Table 5, the average length of hospital stay in the antibiotic treatment group was 7.8 ± 2.5 d, which was significantly longer than that of the non-antibiotic treatment group (5.7 ± 1.8 d; P < 0.05). The cure rate was 98.3% in the antibiotic treatment group and 87.9% in the non-antibiotic treatment group (P < 0.05).
Acute bronchiolitis is a common cause of infant emergency department attendance and hospitalization[6]. In developed countries, infants under 1 year old with bronchiolitis account for 18% of all pediatric inpatients[7]. In this study, bronchiolitis infants under 1 year old accounted for about 13.5% (132/976) of all pediatric inpatients, which is slightly lower than previous reports. Bronchiolitis is a viral infectious disease, and the virus detection rate in severe bronchiolitis is 100%. Respiratory syncytial virus is the most important pathogenic factor for bronchiolitis[3,4]. More convincingly, routine respiratory virus examinations were not conducted for all children, an aspect that requires improvement. Furthermore, the study observed a higher incidence in male children compared to female, with a male-to-female incidence ratio of approximately 1:0.54. The age of onset was primarily between January and 6 months of age. These findings are not entirely consistent with related reports, which may be attributed to the short duration of the statistical period and the small sample size. Further verification is needed.
Most children hospitalized for acute bronchiolitis have a stable course[8]; however, approximately 2%-6% require admission to a pediatric intensive care unit[9]. The diagnosis of the disease mainly depends on the patient's clinical manifestations, signs, and imaging examination. Clinical manifestations mainly include common symtoms of viral infections, such as sneezing, runny nose, and fever, the gradual development of paroxysmal cough, asthma, etc. The chest manifestations were nonspecific, and most of them were accompanied by wheezing and wet rales in the lungs. In this study, in addition to cough, the children mainly presented with wheezing, increased and blurred lung texture on pulmonary imaging, and dry rales and wet rales on clinical auscultation, with a small number of children having fever and perioral cyanosis.
At present, the treatment of this disease is controversial, and there is no clear recommendation to use any drug for the treatment of bronchiolitis[10]. Common medications such as bronchodilators, corticosteroids, and hypertonic saline only provide symptom relief[11]. There is still insufficient evidence for other treatments, such as aerosol inhalation of hypertonic saline, and their role should be further clarified in the future. In this study, 71.7% of the patients were treated with antibiotics, about 41.2% were treated with hormone drugs, and 71.1% were treated with antiviral therapy. The commonly used nebulised drugs were budesonide plus terbutaline (45.6%) and budesonide plus salbutamol (38.5%).
Children with bronchiolitis mostly have a good prognosis. However, some children have persistent problems (e.g., wheezing and cough) after acute infection (> 14 d), increasing the risk of later persistent lung disease and costs to health systems. Active anti-infection treatment could improve the status of more children. In a small randomized trial, azithromycin treatment appeared to reduce the risk of subsequent long-term respiratory disease in 40 hospitalized children with respiratory syncytial virus bronchiolitis during an acute exacerbation[12], which is similar to the findings in this study. In this study, we found that the probability of bacterial infection in patients with capillary bronchitis was low, yet the use of antibiotics was common. Further research revealed that in patients without a clear bacterial infection, antibiotic use significantly improved the cure rate (P < 0.05). However, it also prolonged the duration of hospitalization (P < 0.05), highlighting the need for standardized antibiotic use. Moreover, bronchiolitis may lead to lung injury, which can result in recurring wheezing episodes and the development of asthma[13]. It is suggested that severe bronchiolitis during the first episode could be a critical factor or event, and should be considered in designing secondary prevention strategies for asthma. Post-discharge follow-up for up to one year revealed that two cases still experienced symptoms like cough, wheezing, shortness of breath, and other respiratory issues, which were particularly pronounced during respiratory infections or mild exercise.
Bronchiolitis is a common acute respiratory infectious disease in infants and young children. It mainly affects male children and the age onset is between 1 to 6 mo. The standard use of antibiotics should be emphasized in view of the prolonged average length of hospital stay between the antibiotic treatment group and the non-antibiotic treatment group. When the course of disease is more than 7 d or the treatment effect is poor, active anti-infective treatment is needed to improve the long-term prognosis. Very few children have recurrent cough and wheezing symptoms within 1 year, which may be related to the risk of later asthma attack.
Bronchiolitis is one of the common lower respiratory tract infections in infants and young children. Severe cases are accompanied by dyspnea and decreased oxygen saturation.
To investigate the clinical characteristics, standardized diagnosis, and treatment of bronchiolitis.
Comparative analysis of the use of antibiotics in bronchiolitis infants with and without bacterial infection has revealed that the use of antibiotics in the treatment of bronchiolitis is controversial. Increasing the use of antibiotics can improve the cure rate of patients, but it will prolong the length of hospital stay. It is necessary to optimize the treatment methods to reduce the length of hospital stay and financial burden of patients.
The clinical data of 114 children with newly diagnosed bronchiolitis at the Department of Pediatrics, Tongling Maternal and Child Health Hospital from January 2019 to December 2019 were retrospectively analyzed. The clinical features, imaging features, treatment, and other data were recorded and analyzed.
The age of onset was mostly from 1 mo to 6 mo, and the time to hospital visit was mostly from the second day to the fourth day of the course of the disease. Lung imaging studies showed increased and blurred lung texture. The main treatment was aerosol inhalation. The average hospitalization time was 7.1 ± 2.4 d, and the total cure rate was 94.7%. In patients without bacterial infection, the use of antibiotics significantly prolonged the length of hospital stay (7.8 ± 2.5 d vs 5.7 ± 1.8 d) and improved the cure rate (98.3% vs 87.9%, P < 0.05).
Most of the affected infants are male and have a good prognosis. Unnecessary use of antibiotics may significantly prolong the length of hospital stay, thereby putting pressure on both patients and the hospital system.
Measures should be taken to optimize the treatment methods, and shorten the treatment time and the length of hospital stay, so as to reduce the economic pressure on both patients and on the hospital system.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alsamhi SH, Ireland S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Dalziel SR, Haskell L, O'Brien S, Borland ML, Plint AC, Babl FE, Oakley E. Bronchiolitis. Lancet. 2022;400:392-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 93] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 2. | Meissner HC. Viral Bronchiolitis in Children. N Engl J Med. 2016;374:62-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 491] [Article Influence: 54.6] [Reference Citation Analysis (1)] |
| 3. | Manti S, Staiano A, Orfeo L, Midulla F, Marseglia GL, Ghizzi C, Zampogna S, Carnielli VP, Favilli S, Ruggieri M, Perri D, Di Mauro G, Gattinara GC, D'Avino A, Becherucci P, Prete A, Zampino G, Lanari M, Biban P, Manzoni P, Esposito S, Corsello G, Baraldi E. UPDATE - 2022 Italian guidelines on the management of bronchiolitis in infants. Ital J Pediatr. 2023;49:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 4. | Wainwright C. Acute viral bronchiolitis in children- a very common condition with few therapeutic options. Paediatr Respir Rev. 2010;11:39-45; quiz 45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 5. | Milési C, Baudin F, Durand P, Emeriaud G, Essouri S, Pouyau R, Baleine J, Beldjilali S, Bordessoule A, Breinig S, Demaret P, Desprez P, Gaillard-Leroux B, Guichoux J, Guilbert AS, Guillot C, Jean S, Levy M, Noizet-Yverneau O, Rambaud J, Recher M, Reynaud S, Valla F, Radoui K, Faure MA, Ferraro G, Mortamet G; French Speaking Group for Pediatric Intensive and Emergency Care. Clinical practice guidelines: management of severe bronchiolitis in infants under 12 months old admitted to a pediatric critical care unit. Intensive Care Med. 2023;49:5-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | Ghazaly M, Nadel S. Characteristics of children admitted to intensive care with acute bronchiolitis. Eur J Pediatr. 2018;177:913-920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 7. | Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Trends in bronchiolitis hospitalizations in the United States, 2000-2009. Pediatrics. 2013;132:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 385] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 8. | Birkhaug IM, Inchley CS, Aamodt G, Ånestad G, Nystad W, Nakstad B. Infectious burden of respiratory syncytial virus in relation to time of birth modifies the risk of lower respiratory tract infection in infancy: the Norwegian Mother and Child Cohort. Pediatr Infect Dis J. 2013;32:e235-e241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Ghazaly MMH, Abu Faddan NH, Raafat DM, Mohammed NA, Nadel S. Acute viral bronchiolitis as a cause of pediatric acute respiratory distress syndrome. Eur J Pediatr. 2021;180:1229-1234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, Johnson DW, Light MJ, Maraqa NF, Mendonca EA, Phelan KJ, Zorc JJ, Stanko-Lopp D, Brown MA, Nathanson I, Rosenblum E, Sayles S 3rd, Hernandez-Cancio S; American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134:e1474-e1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 1139] [Article Influence: 103.5] [Reference Citation Analysis (0)] |
| 11. | Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet. 2017;389:211-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 296] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 12. | Stokholm J, Chawes BL, Vissing NH, Bjarnadóttir E, Pedersen TM, Vinding RK, Schoos AM, Wolsk HM, Thorsteinsdóttir S, Hallas HW, Arianto L, Schjørring S, Krogfelt KA, Fischer TK, Pipper CB, Bønnelykke K, Bisgaard H. Azithromycin for episodes with asthma-like symptoms in young children aged 1-3 years: a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2016;4:19-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 138] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 13. | Jartti T, Smits HH, Bønnelykke K, Bircan O, Elenius V, Konradsen JR, Maggina P, Makrinioti H, Stokholm J, Hedlin G, Papadopoulos N, Ruszczynski M, Ryczaj K, Schaub B, Schwarze J, Skevaki C, Stenberg-Hammar K, Feleszko W; EAACI Task Force on Clinical Practice Recommendations on Preschool Wheeze. Bronchiolitis needs a revisit: Distinguishing between virus entities and their treatments. Allergy. 2019;74:40-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |