Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8276
Peer-review started: September 27, 2023
First decision: October 24, 2023
Revised: November 18, 2023
Accepted: November 30, 2023
Article in press: November 30, 2023
Published online: December 16, 2023
Processing time: 77 Days and 17.2 Hours
Acute pancreatitis (AP) is a common inflammatory disease of the pancreas with high mortality rates. It is of great significance to take scientific intervention measures for patients with AP in time.
To explore the effect of standardized nursing combined with mindfulness stress reduction training on the curative effect, negative emotion, and quality of life in patients with acute pancreatitis.
A total of 80 patients with acute pancreatitis admitted to The First People's Hospital of Jiangxia District Hospital from May 2021 to May 2023 were randomly divided into control group and observation group (n = 40). Patients in control group were given the standardized nursing intervention, and the observation group were given standardized nursing plus mindfulness stress reduction training intervention. The time of clinical symptom disappeared or improved, complication occurrence rate, emotional state, and quality of life score of the two groups were observed and compared.
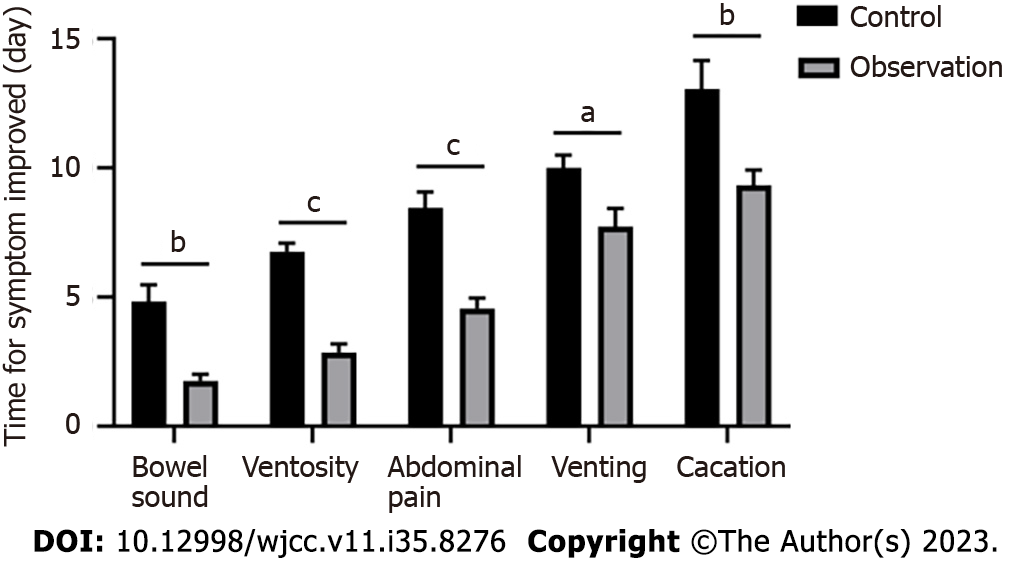
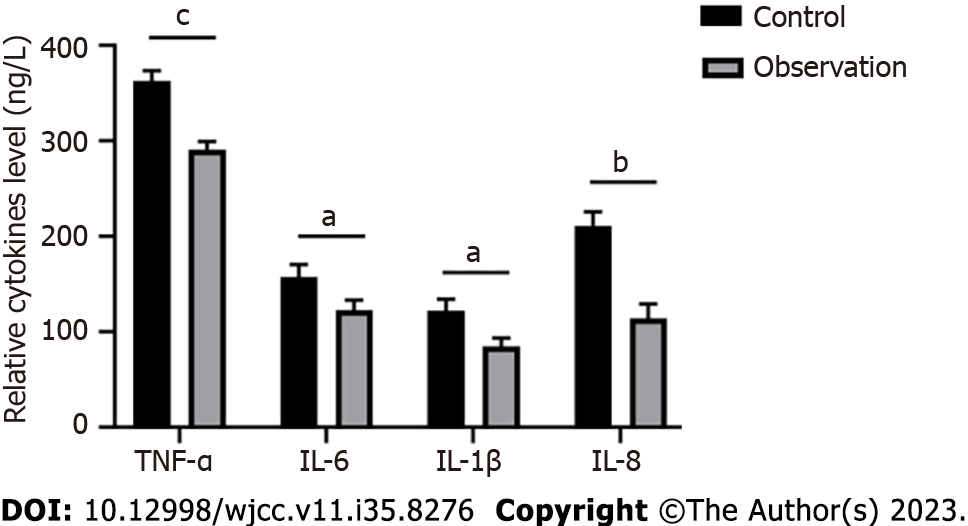
In comparison with the control group, the bowel sound recovery time, ventosity and abdominal pain improvement time, and venting and cacation time in observation group were shorter, and the total incidence rate of complications was reduced, showing statistically significant difference (P < 0.05). The scores of anxiety and depression in observation group were lower than those in control group (P < 0.05). Serum levels of tumour necrosis factor alpha, interleukin (IL)-6, IL-1β and IL-8 in observation group were lower than those in control group (P < 0.05). The scores of life quality in physiology, psychology, environment and social relations in observation group were higher than those in control group, and the differences were statistically significant (P < 0.05).
The application of standardized nursing intervention combined with mindfulness stress reduction training in patients with acute pancreatitis has a definite effect, which can help to ameliorate the clinical symptoms, anxiety and depression of patients, reduce the incidence rate of complications, and improve the prognosis of patients.
Core Tip: Acute pancreatitis is a destructive inflammatory condition of the pancreas in gastroenterology. In this study, after intervention of standardized nursing combined with mindfulness stress reduction training, the total incidence rate of complications, the scores of anxiety and depression, and levels of serum inflammatory cytokines were decreased, and the scores of life quality was elevated, suggesting that the combined intervention of standardized nursing and mindfulness stress reduction training is beneficial to reduce complications and negative emotions, as well as improve quality of life.
- Citation: Li S, Yin D, Guo XC. Influence of standardized nursing intervention combined with mindfulness stress reduction training on the curative effect in patients with acute pancreatitis. World J Clin Cases 2023; 11(35): 8276-8283
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8276.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8276
Acute pancreatitis is a common acute severe disease in the department of gastroenterology[1]. It is mainly caused by a variety of pathogeny, such as biliary tract diseases, alcohol consumption, hyperlipidemia, infectious factors, autoimmune diseases, etc., and produces local inflammatory response after being applied to pancreatic tissue[2-4]. The disease has a sudden onset and rapid progression, and is easily accompanied by complications such as peritonitis, secondary infection and shock, which may even endanger the life safety of patients if not treated in time[4,5]. The clinical treatment process can produce a variety of serious complications, and patients are prone to anxiety, depression and other emotions[6], so the treatment should be included scientific and reasonable nursing mode intervention.
With the continuous development of the bio-psycho-social medical model, the application of the psychological intervention technology of mindfulness stress reduction training has attracted extensive attention of scholars[7]. Mindfulness is a method of self-regulation by being aware of your thoughts, actions, and behaviors without judgment[8]. Mindfulness stress reduction training is a training method formed on the basis of mindfulness theory, through intensive meditation practice to help trainers cope with stress and manage emotions, and ultimately achieve the purpose of improving physical and mental problems[9,10]. At present, there are few studies on mindfulness stress reduction training in the treatment of acute pancreatitis. Therefore, it is of great significance to explore the effect of standardized nursing intervention combined with mindfulness stress reduction training in the treatment of patients with acute pancreatitis.
This study selected 80 patients with acute pancreatitis admitted to the gastroenterology department of our hospital from May 2021 to May 2023, aiming to explore the effects of standardized nursing intervention combined with mind
A total of 80 patients with acute pancreatitis admitted to the gastroenterology department of our hospital were selected and randomly divided into control group and observation group. The control group contains 40 patients, including 23 male patients and 17 female patients, the average age was (33.52 ± 6.35) years old, and the mean course of disease was (39.25 ± 5.40) h. The observation group consisted of 40 patients, including 24 male patients and 16 female patients, the average age was (32.95 ± 6.20) years old, and the mean course of disease was (39.45 ± 5.34) h. There was no significant difference in gender, age and other general data between the two groups (P > 0.05), indicating comparability. This study has been approved by the Ethics Committee of XX Hospital.
Inclusion criteria: (1) All the patients met the relevant diagnostic criteria in the Chinese Guidelines for Diagnosis and Treatment of Acute Pancreatitis (Shanghai, 2013); (2) All the patients have normal cognitive and communication functions; (3) All the patients have signed the informed consent and can return to the hospital for review regularly; and (4) all the patients have complete clinical data. Exclusion criteria: (1) Patients with severe organ diseases; (2) Patients with mental disorders or diseases; (3) Patients with malignant tumors or systemic immune diseases; and (4) Patients cannot cooperate with the experimental researcher.
The two groups of diagnosed patients were treated with routine symptomatic treatment, including fluid rehydration, nutritional support, spasmodic, pain relief, gastrointestinal decompression, jejunal nutrition tube, etc.
Control group: Patients in control group received standard nursing intervention, and the intervention services included timely observation of the condition at admission, psychological nursing, and diet nursing. Patients with abdominal distension and abdominal pain were given guidance on abdominal muscle relaxation, analgesic drugs, and ventilation and defecation status of patients were closely monitored. Closely observed the gastrointestinal decompression tube of the patient to ensure that the drainage tube was smooth and ensure the continuity of gastrointestinal decom
Observation group: Patients in observation group were given mindfulness stress reduction training on the basis of control group. The contents of mindfulness stress reduction training group included as follows: Week 1: A professional psychologist explained the theory to the patients, informed the purpose, process, significance, etc. At the same time, distributed relevant materials related to chemical training, narrated the contents including mindful breathing and methods, and discussed how to use mindful introspection to relieve stress in life and work. Week 2: Review and analyze the problems in mindfulness training, explain the purpose, method and significance of walking meditation, teach patients how to apply walking meditation to life, and guide them to complete walking meditation training after class. Week 3: Review and analyze the problems of walking meditation after class, and then guide patients to do mental and physical scanning training to feel various parts of the body. Week 4: Apply the mindfulness meditation training of the previous 3 wk to the classic yoga movements to further experience the mindfulness training. Week 5: Instruct the patient to do zazen training and apply mindfulness meditation to further experience this stress reduction training. Week 6: Review and analyze the learning content of the previous 5 wk with zazen training, share their shortcomings and advantages and solve them one by one. It is required to do training at least once a week, each time about 3 h, the first half hour is a review and analysis, and the self-training after class is not less than 5 d (about 30 min each). The intervention lasted for 6 wk.
Observation indicators: (1) The recovery time of abdominal pain and abdominal distension in the two groups; (2) The occurrence of complications during treatment in the two groups; (3) The anxiety and depression status were evaluated according to the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS). The higher score of SAS and SDS indicate severer anxiety and depression; (4) The life quality of patients in the two groups was assessed according to the Chinese version of WHO QOL-100. The score relates to 4 areas: Psychological field, physiological field, environmental field and social relations, and the higher score suggest the higher life quality; and (5) Comparison of inflammatory indicators between the two groups: 5 mL of venous blood was collected from the fasting patients of the two groups, centrifuged at 3000 rpm for 10 min to separate serum, and the levels of TNF-α, IL-6, IL-1β and IL-8 in serum were detected by enzyme-linked immunosorbent assay.
Statistical Methods The data in this study were analyzed using SPSS18.0 statistical software. Measurement data were represented by mean ± SD, and t-test was performed between groups. The counting data were represented as n/% and analyzed by χ2 test. P < 0.05 was considered statistically significant.
As shown in Table 1, there was no statistically significant difference between the control group and the observation group in gender, age, body mass index, disease course, the proportion of mild pancreatitis and severe pancreatitis, marital status, educational level, and other general data (P > 0.05), indicating that the data of the two groups were comparable.
| General data | Control group (n = 40) | Observation group (n = 40) | χ2/t | P value |
| Sex, male | 23 (57.5) | 24 (60.0) | 0.043 | 0.905 |
| Female | 17 (42.5) | 16 (40.0) | ||
| Age (yr, mean ± SD) | 33.52 ± 6.35 | 32.95 ± 6.20 | 0.073 | 0.830 |
| Course of disease (h, mean ± SD) | 39.25 ± 5.40 | 39.45 ± 5.34 | 0.613 | 0.503 |
| BMI (kg/m2, mean ± SD) | 22.64 ± 2.16 | 22.71 ± 2.11 | 0.235 | 0.416 |
| Mild acute pancreatitis | 32 (80.0) | 34 (85.0) | 0.423 | 0.104 |
| Serve acute pancreatitis | 8 (20.0) | 6 (15.0) | ||
| Marital status | 0.240 | 0.632 | ||
| Married | 31 (77.5) | 33 (82.5) | ||
| Spinsterhood, divorced, widowed | 9 (22.5) | 7 (17.5) | ||
| Education level | 1.231 | 0.522 | ||
| Above high school | 33 (82.5) | 32 (80.0) | ||
| High school and below | 7 (17.5) | 8 (20.0) |
Compared with the control group, the recovery time of bowel sound, the disappearance time of abdominal pain and ventosity, and the time of venting and cacation were all shortened in the observation group, with statistical significance
In the control group, 5 cases of sedimentary pneumonia (12.50%) and 4 cases of pressure sore (10.00%) occurred, and the total complication rate was 22.50%. In the observation group, there was 1 case of sedimentary pneumonia (2.50%) and 1 case of pressure sore (2.50%), and the total complication rate was 5.00%. The total complication occurrence rate in the observation group was lower than that in the control group (P < 0.05, Table 2).
According to the evaluation of SAS and SDS, the anxiety scores of the observation group were lower than those of the control group, and there was a statistical difference between the two groups (P < 0.05). The depression scores of the observation group were lower than those of the control group, with statistical difference between the two groups (P < 0.05, Table 3).
Compared with the control group, the serum levels of tumour necrosis factor alpha (TNF alpha), interleukin (IL)-6, IL-1β and IL-8 in the observation group were all decreased, with statistical differences between the two groups (P < 0.05, Figure 2).
The life quality scores of the two groups were measured during follow-up, and the scores of the observation group in the psychological field, physiological field, environmental field and social relations were higher than those of the control group, with statistical significance (P < 0.05, Table 4).
With the continuous development of modern society and economy, people's irregular diet is increasing, resulting in the prevalence of acute pancreatitis rising year by year[11,12]. In patients with pancreatitis, the trypsin in the pancreas is activated, leading to edema and bleeding in the tissues around the pancreas, and even produce necrotic inflammatory reactions, which seriously reduces the life quality of patients[13,14]. In addition to clinical treatment, scientific nursing intervention is equally important, while the nursing intervention alone cannot achieve an ideal effect[15,16]. Therefore, on the basis of standardized nursing, more comprehensive and high-quality intervention measures should be taken. In this study, standardized nursing combined with mindfulness stress reduction training was used to intervene patients with acute pancreatitis. Compared with the standardized nursing alone, the recovery time of clinical symptoms in the combined treatment group was shorter, the total incidence of complications was reduced, the levels of serum inflammatory factors were decreased, the scores of anxiety and depression were declined, and the scores of patients' life quality in physiological, psychological, environmental and social fields were increased. These results suggest that combined therapy has a good effect on improving the clinical symptoms, psychological state and life quality of patients with acute pancreatitis.
Mindfulness stress reduction training combines meditation, yoga and other activities, and applies psychological intervention and guidance to achieve the purpose of improving the emotional state of patients[7,17,18]. The training node is calculated by week, guiding patients to do mindfulness training step by step every week, and ensuring that the content of the previous week is reviewed and analyzed before each training, which can effectively divert their attention[19,20]. Here, we found that compared with the control group, the recovery time of bowel sound, ventosity and abdominal pain improvement time, venting time and cacation time of patients in the observation group were shorter, and the total incidence of complications was reduced. The anxiety and depression scores of the observation group were lower than those of the control group. These results indicate that mindfulness stress reduction training combined with standardized nursing intervention can effectively alleviate clinical symptoms and negative emotions in patients with acute pancreatitis. The reason may be that, under the intervention of mindfulness stress reduction, through professional communication methods, patients' cognition of the disease is changed, so as to eliminate bad emotions and divert attention, thereby achieving the effect of soothing the body and mind. Similarly, Sanilevici et al[21] reported that mindfulness stress reduction training can improve negative emotions and increase mental health regulation in coronavirus disease 2019 patients.
Additionally, we also found that the levels of serum inflammatory factors TNF-α, IL-6, IL-1β and IL-8 in the observation group were lower than those in the control group, and the life quality score of patients in the observation group was significantly higher than that in the control group, involving physiological fields, psychological fields, environmental fields and social relations. These results indicate that the combination therapy can improve the anti-inflammatory response and social ability of patients. Due to the impact of the disease, the patient's physiology and psychology are greatly destroyed[22,23]. The combination therapy can specifically intervene the patient's situation, and improve the quality of life and psychological state to a certain extent. The combined treatment enables patients to get positive stimulation in both physical and mental aspects, ensuring adequate nutrition can improve various functions of the body, reduce inflammation and enhance immunity, which may be related to mindfulness stress reduction training to eliminate patients' negative emotions and promote patients' self-confidence. A recent study showed that mindfulness stress reduction training can reduce stress and inflammatory cytokine levels in patients with autoimmune hepatitis[24]. Another study reported that mindfulness stress reduction training improved psychological and inflammatory responses in breast cancer patients[25]. These results are basically consistent with the present researches.
In summary, mindfulness stress reduction training combined with standardized nursing can effectively improve clinical symptoms of patients with acute pancreatitis, reduce the incidence of complications, decrease inflammation, improve patients' negative emotions, and improve their quality of life. This kind of combination therapy is effective and beneficial to improve the prognosis of patients, and it is worth promoting. However, there are some limitations in this study. The sample size is a bit small, and the observational indicators such as nursing satisfaction rate and physical rehabilitation indicators are absent. Further studies were needed to overcome these limitations to make the data more convincing.
Acute pancreatitis is one of the common acute abdomen in gastroenterology, which has the characteristics of acute onset, severe disease, and rapid change, and is easy to endanger life if not actively treated.
Psychological intervention care can alleviate negativity in patients with acute pancreatitis.It effectively improves the treatment effect of patients.
To explore the effect of standardized nursing combined with mindfulness-based stress reduction training on the rehabilitation of patients with acute pancreatitis.
A total of 80 patients in our hospital were retrospectively analyzed, and the recovery of the patients was studied.
The results showed significant improvement in all indicators.
This study firstly found that the standardized nursing combined with mindfulness stress reduction training had defined curative effect on patients with acute pancreatitis (AP), which ameliorated clinical symptoms, negative emotion, and quality of life. Our study provide an effective nursing intervention method for AP.
AP is one of the most common inflammatory diseases and requires scientific and reasonable intervention measures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Iqbal Z, United States S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Li XY, He C, Zhu Y, Lu NH. Role of gut microbiota on intestinal barrier function in acute pancreatitis. World J Gastroenterol. 2020;26:2187-2193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 69] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (3)] |
| 2. | Bálint ER, Fűr G, Kiss L, Németh DI, Soós A, Hegyi P, Szakács Z, Tinusz B, Varjú P, Vincze Á, Erőss B, Czimmer J, Szepes Z, Varga G, Rakonczay Z Jr. Assessment of the course of acute pancreatitis in the light of aetiology: a systematic review and meta-analysis. Sci Rep. 2020;10:17936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 3. | Gupta M, Liti B, Barrett C, Thompson PD, Fernandez AB. Prevention and Management of Hypertriglyceridemia-Induced Acute Pancreatitis During Pregnancy: A Systematic Review. Am J Med. 2022;135:709-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Ge P, Luo Y, Okoye CS, Chen H, Liu J, Zhang G, Xu C. Intestinal barrier damage, systemic inflammatory response syndrome, and acute lung injury: A troublesome trio for acute pancreatitis. Biomed Pharmacother. 2020;132:110770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 123] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 5. | Ding L, Yang Y, Li H, Wang H, Gao P. Circulating Lymphocyte Subsets Induce Secondary Infection in Acute Pancreatitis. Front Cell Infect Microbiol. 2020;10:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | McGuire SP, Montero AM, McGreevy KA, Zyromski NJ. Pancreatitis associated anxiety, depression, and stress: Hypothesis, definition, and intervention. Surg Open Sci. 2022;10:50-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Lenze EJ, Voegtle M, Miller JP, Ances BM, Balota DA, Barch D, Depp CA, Diniz BS, Eyler LT, Foster ER, Gettinger TR, Head D, Hershey T, Klein S, Nichols JF, Nicol GE, Nishino T, Patterson BW, Rodebaugh TL, Schweiger J, Shimony JS, Sinacore DR, Snyder AZ, Tate S, Twamley EW, Wing D, Wu GF, Yang L, Yingling MD, Wetherell JL. Effects of Mindfulness Training and Exercise on Cognitive Function in Older Adults: A Randomized Clinical Trial. JAMA. 2022;328:2218-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 64] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 8. | Green AA, Kinchen EV. The Effects of Mindfulness Meditation on Stress and Burnout in Nurses. J Holist Nurs. 2021;39:356-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 9. | Tobias Mortlock J, Carter A, Querstret D. Extending the Transformative Potential of Mindfulness Through Team Mindfulness Training, Integrating Individual With Collective Mindfulness, in a High-Stress Military Setting. Front Psychol. 2022;13:867110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Crane RS, Callen-Davies R, Francis A, Francis D, Gibbs P, Mulligan B, O'Neill B, Pierce Williams NK, Waupoose M, Vallejo Z. Mindfulness-Based Stress Reduction for Our Time: A Curriculum that is up to the Task. Glob Adv Integr Med Health. 2023;12:27536130231162604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 11. | Yang AL, McNabb-Baltar J. Hypertriglyceridemia and acute pancreatitis. Pancreatology. 2020;20:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 12. | Khoja K, Sadiq O, Chisholm PR, Dua KS, Madhavan S, Smith ZL. The incidence of new mental health disorders after acute pancreatitis: A large, propensity-matched, observational study. Pancreatology. 2023;23:163-170. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Cañamares-Orbís P, García-Rayado G, Alfaro-Almajano E. Nutritional Support in Pancreatic Diseases. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 14. | Zhang Q, Li S, Yu Y, Zhu Y, Tong R. A Mini-Review of Diagnostic and Therapeutic Nano-Tools for Pancreatitis. Int J Nanomedicine. 2022;17:4367-4381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 15. | He F, He RX. Systematic nursing interventions in gastric cancer: A randomized controlled study. World J Clin Cases. 2022;10:1843-1851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (2)] |
| 16. | Tu X, Liu Q, Chen L, Li J, Yu X, Jiao X, Wang N, Hu L, Yuan Y, Gong W, Ding Y, Shi X, Xiao W, Lu G. Number of recurrences is significantly associated with the post-acute pancreatitis diabetes mellitus in a population with hypertriglyceridemic acute pancreatitis. Lipids Health Dis. 2023;22:82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Foley T, Lanzillotta-Rangeley J. Stress Reduction Through Mindfulness Meditation in Student Registered Nurse Anesthetists. AANA J. 2021;89:284-289. [PubMed] |
| 18. | Sun Y, Li Y, Wang J, Chen Q, Bazzano AN, Cao F. Effectiveness of Smartphone-Based Mindfulness Training on Maternal Perinatal Depression: Randomized Controlled Trial. J Med Internet Res. 2021;23:e23410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 84] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 19. | Sarazine J, Heitschmidt M, Vondracek H, Sarris S, Marcinkowski N, Kleinpell R. Mindfulness Workshops Effects on Nurses' Burnout, Stress, and Mindfulness Skills. Holist Nurs Pract. 2021;35:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Kaisti I, Kulmala P, Hintsanen M, Hurtig T, Repo S, Paunio T, Miettunen J, Halt AH, Jääskeläinen E. The effects of mindfulness-based interventions in medical students: a systematic review. Adv Health Sci Educ Theory Pract. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Sanilevici M, Reuveni O, Lev-Ari S, Golland Y, Levit-Binnun N. Mindfulness-Based Stress Reduction Increases Mental Wellbeing and Emotion Regulation During the First Wave of the COVID-19 Pandemic: A Synchronous Online Intervention Study. Front Psychol. 2021;12:720965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Dunbar E, Greer PJ, Melhem N, Alkaade S, Amann ST, Brand R, Coté GA, Forsmark CE, Gardner TB, Gelrud A, Guda NM, LaRusch J, Lewis MD, Machicado JD, Muniraj T, Papachristou GI, Romagnuolo J, Sandhu BS, Sherman S, Wilcox CM, Singh VK, Yadav D, Whitcomb DC; NAPS2 study group. Constant-severe pain in chronic pancreatitis is associated with genetic loci for major depression in the NAPS2 cohort. J Gastroenterol. 2020;55:1000-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Fonseca Sepúlveda EV, Guerrero-Lozano R. Acute pancreatitis and recurrent acute pancreatitis: an exploration of clinical and etiologic factors and outcomes. J Pediatr (Rio J). 2019;95:713-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Alrabadi LS, Dutton A, Rabiee A, Roberts SJ, Deng Y, Cusack L, Silveira MG, Ciarleglio M, Bucala R, Sinha R, Boyer JL, Assis DN. Mindfulness-based stress reduction may decrease stress, disease activity, and inflammatory cytokine levels in patients with autoimmune hepatitis. JHEP Rep. 2022;4:100450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 25. | Mirmahmoodi M, Mangalian P, Ahmadi A, Dehghan M. The Effect of Mindfulness-Based Stress Reduction Group Counseling on Psychological and Inflammatory Responses of the Women With Breast Cancer. Integr Cancer Ther. 2020;19:1534735420946819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |