Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8235
Peer-review started: October 17, 2023
First decision: November 1, 2023
Revised: November 15, 2023
Accepted: November 28, 2023
Article in press: November 28, 2023
Published online: December 6, 2023
Processing time: 44 Days and 22.8 Hours
One challenging scenario in the treatment of biliary stricture is that post-liver transplantation (LT) biliary strictures cannot be accessed using endoscopic retrograde cholangiopancreatography (ERCP). Here, we report such a case that was successfully treated using a novel endoscopic technique.
A 60-year-old man presented with obstructive jaundice caused by a post-LT biliary stricture. He underwent LT for compensated alcoholic liver cirrhosis and hepatocellular carcinoma. Laboratory investigations unveiled a cholestatic pattern of abnormalities in liver function and a total bilirubin level of 16 mg/dL. Magnetic resonance cholangiopancreatography revealed a stricture extending from the right intrahepatic bile duct into the common hepatic duct. Severe postoperative deformities made accessing the ampulla of Vater with a side-viewing duodenoscope impossible. Percutaneous transhepatic biliary drainage (PTBD) was performed to treat biliary obstruction. Moreover, to resolve the stricture completely, a fully covered self-expandable metal stent (FC-SEMS) with a novel proximal retrievable string was deployed into the post-LT biliary stricture through the PTBD tract. Before inserting the stent through the PTBD tract, the stent with the distal string was manually inverted to ensure that the distal part with the string became the proximal part for later endoscopic removal. After 6 mo, the FC-SEMS was successfully removed without complications, as the string was pulled out using a forward-viewing gastroscope.
Deployment and endoscopic removal of an FC-SEMS with a novel proximal string through the PTBD tract may be a viable option for treating post-LT biliary strictures that are inaccessible by ERCP.
Core Tip: Post-liver transplantation biliary stricture is complex and involves many variables. There is no established method for its evaluation and treatment, and various approaches are needed depending on patient factors. While a fully covered self-expandable metal stent shows good effectiveness, it is premised on endoscopic access. This case report presents a new solution through percutaneous stent insertion and endoscopic removal in cases where endoscopic retrograde cholangiopancreatography is not possible.
- Citation: Lee Y, Park CH, Cho E, Kim KH. Management of post-liver transplantation biliary stricture inaccessible by endoscopic retrograde cholangiopancreatography: A case report. World J Clin Cases 2023; 11(34): 8235-8241
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8235.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8235
Endoscopic retrograde cholangiopancreatography (ERCP) has become the standard treatment for benign biliary strictures (BBSs) associated with liver transplantation (LT) owing to the safety and efficacy of the technique[1,2]. However, a percutaneous transhepatic cholangioscopy (PTCS)-guided approach is sometimes required, particularly when ERCP is not feasible. The European Society of Gastrointestinal Endoscopy considers fully covered self-expandable metal stents (FC-SEMS) as the mainstay of BBS treatment[2]. Herein, we report a case of PTCS-guided insertion of an FC-SEMS with a proximal retrieval string in the treatment of a post-LT biliary stricture inaccessible by ERCP. This was followed by the successful endoscopic removal of the FC-SEMS.
A 60-year-old man presented with jaundice.
The patient denied the presence of any symptoms such as fever or abdominal pain.
In 2017, the patient underwent LT for compensated alcoholic liver cirrhosis with hepatocellular carcinoma.
There was no other special personal or family history.
There were no unusual findings on physical examination.
Laboratory investigations revealed a cholestatic pattern of abnormalities in the liver function with a total bilirubin level of 16 mg/dL.
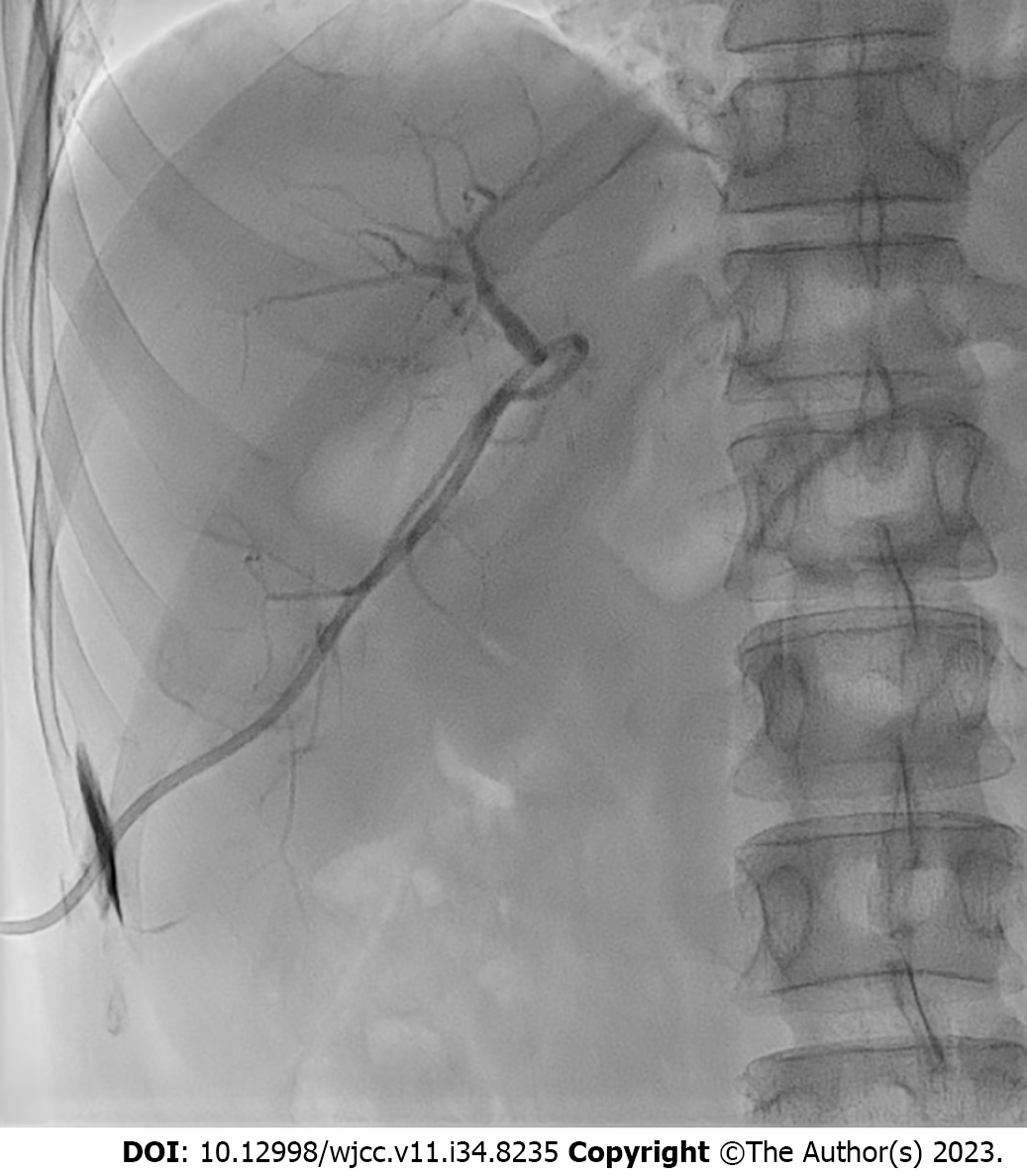
Magnetic resonance cholangiopancreatography revealed a stricture extending from the right intrahepatic bile duct (IHBD) to the common hepatic duct (Figure 1). Therefore, ERCP was planned for the management of the post-LT biliary stricture. Although a forward-viewing gastroscope could reach the ampulla of Vater, a side-viewing duodenoscope was unable to reach the same extent due to severe postoperative deformities, including those at the gastric antrum and duodenal bulb. Percutaneous transhepatic biliary drainage (PTBD) was performed to achieve biliary decompression (Figure 2). During PTBD, it was impossible for the guidewires to pass through the post-LT biliary stricture.
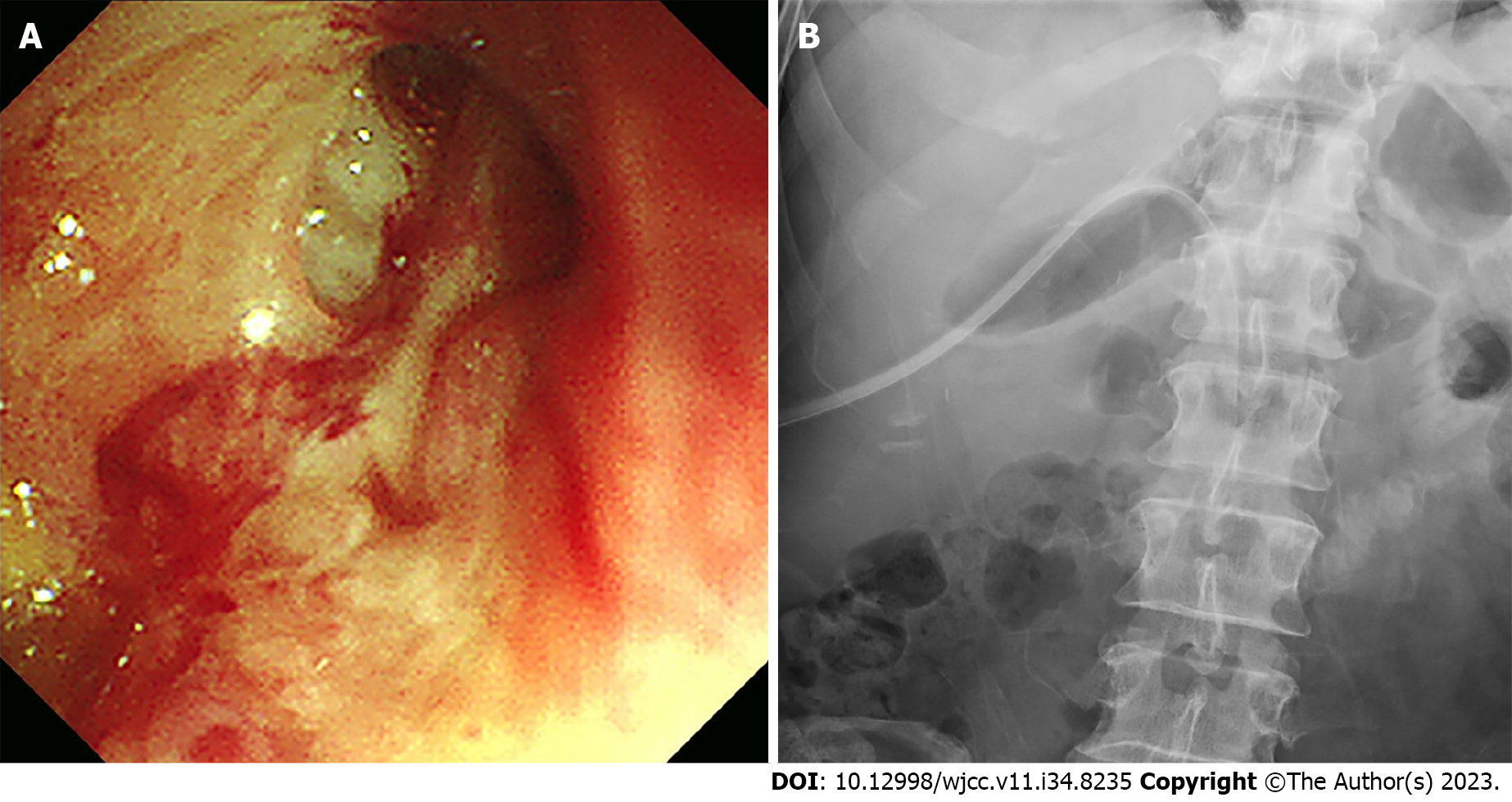
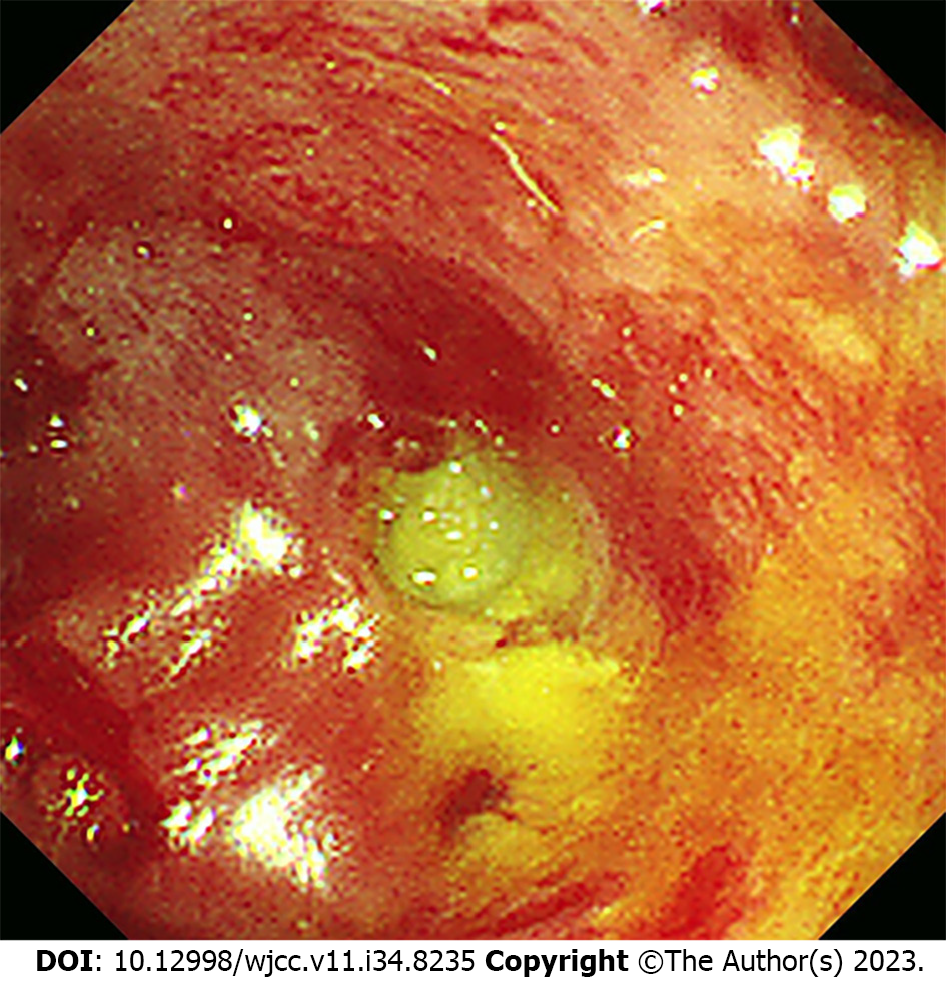
PTCS is imperative for the accurate diagnosis of strictures and their resolution. After 1 wk, the PTBD tract was sequentially dilated using a Mustang balloon dilatation catheter (Boston Scientific, Marlborough, MA, United States), 8 mm in diameter. An 18 Fr PTCS catheter (Akita Sumitomo Bakelite Co. Ltd., Japan) was maintained in situ for 2 wk to facilitate tract maturation. A slit-like stricture opening was detected using PTCS (Figure 3A), and a guidewire was inserted through the opening into the common bile duct and duodenum. Additionally, an 18 Fr PTCS catheter was inserted after stricture dilation to resolve the stricture. Maintenance of the catheter in place for 3 mo was planned (Figure 3B). However, the catheter abruptly migrated into the right IHBD approximately 2 mo after insertion. Cholangioscopy revealed a near-complete obstruction of the previously dilated biliary stricture (Figure 4).
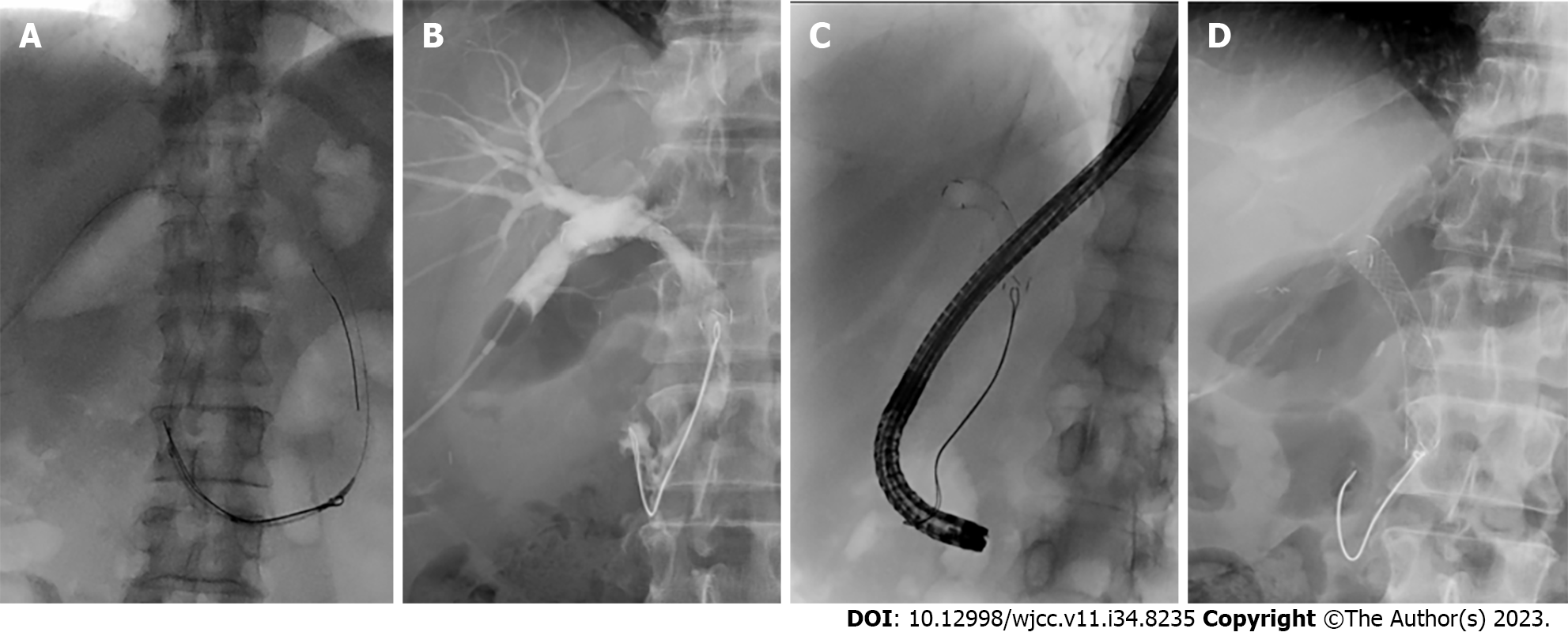
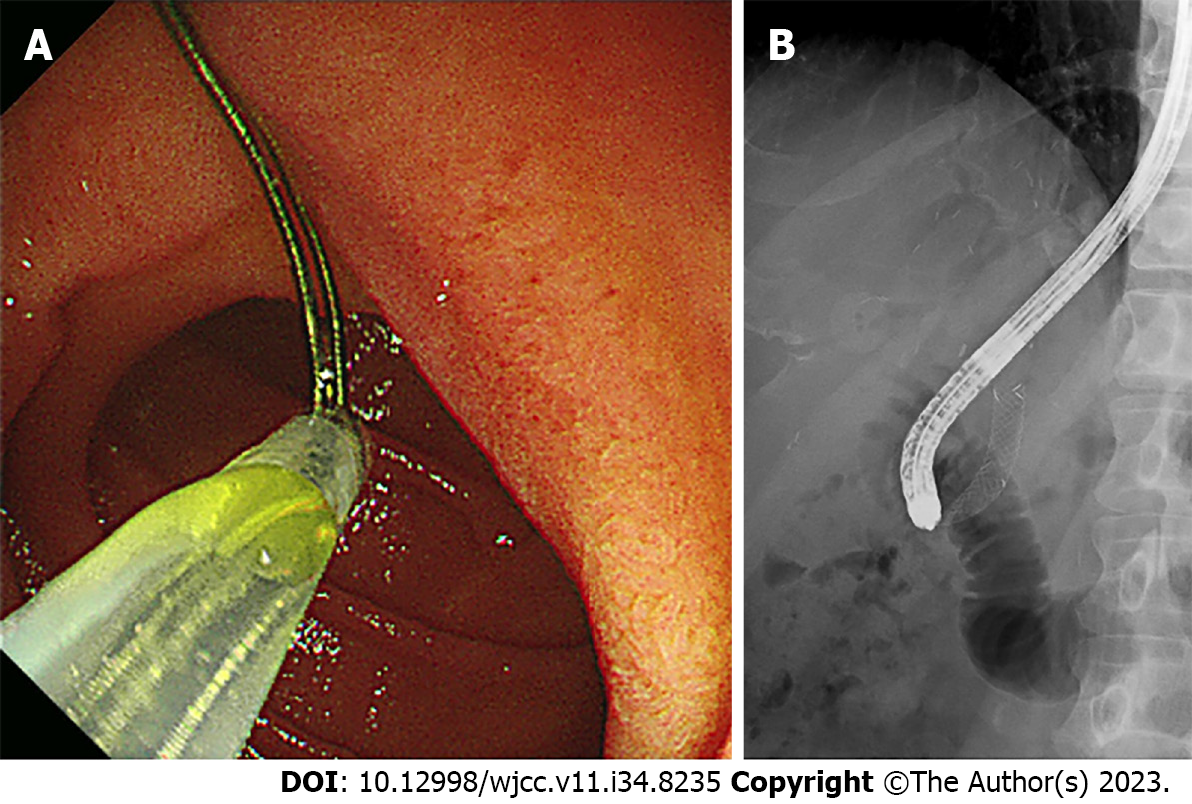
The insertion of a removable FC-SEMS through the PTBD tract was considered a definitive solution for post-LT biliary strictures with a low risk of recurrent PTCS catheter migration. The Kaffes stent (Taewoong Medical, South Korea) is a removable FC-SEMS with a radiopaque retrievable string as the distal attachment. For the endoscopic removal of the Kaffes stent inserted through the PTBD tract, the stent was manually inverted so that the distal part with a retrievable string became the proximal part before stent insertion. The stent was slowly deployed over the stricture under fluoroscopic guidance. Furthermore, the stent was initially inserted up to the third portion of the duodenum and slowly pulled back to the post-LT biliary stricture for the string to spontaneously change direction and be positioned correctly within the duodenal lumen (Figure 5A, Video 1). After the string was confirmed to be well-stretched in the duodenal lumen, the stent was positioned approximately over the stricture site and then deployed (Video 2). Subsequent cholangiography revealed that the stent had blocked the branches of the right proximal IHBD (Figure 5B). The proximal end of the stent was adjusted to be distal to the right IHBD bifurcation to prevent obstruction of the branches of the right IHBD. Simultaneously, the string was carefully pulled using a forward-viewing gastroscope with a snare (Figure 5C and D).
After 6 mo, the Kaffes stent was removed without complications, as the string was pulled out following the same technique using a forward-viewing gastroscope (Figure 6).
Despite advances in endoscopic techniques, post-LT biliary strictures have recently been regarded as among the most difficult complications to address[3]. Post-LT biliary strictures are often complex, associated with recurrences, and inaccessible by ERCP. Numerous studies have demonstrated that the treatment of complex post-LT biliary strictures requires multiple modalities, including interventional radiologic and endoscopic techniques[4]. A recent meta-analysis displayed that multiple plastic stents and removable FC-SEMSs are equally effective and safe procedures for managing refractory biliary strictures or as primary treatment[5]. However, removable FC-SEMSs are favored over the aforementioned options[5].
When post-LT biliary strictures are inaccessible by ERCP, the resolution of the biliary strictures can be challenging. In this context, PTBD plays an important role as a salvage procedure in the treatment of acute cholangitis. However, long-term maintenance of PTBD is associated with significant patient distress and risk of various complications, including catheter dislodgement, bleeding, infection, and bile leakage[6]. A non-removable FC-SEMS may be inserted through the PTBD tract to prevent complications associated with the long-term maintenance of PTBD. However, long-term placement of a non-removable FC-SEMS could also lead to various serious complications such as stent occlusion, stone formation, secondary biliary cirrhosis, and death[7,8].
In the present case, an FC-SEMS with a novel proximal retrieval string was successfully deployed into a post-LT biliary stricture through the PTBD tract. After 6 mo, the FC-SEMS was removed without complications, by pulling out the string using a forward-viewing gastroscope with a snare. To the authors’ knowledge, in the English literature, this was the first endoscopic removal of an FC-SEMS with a novel proximal string inserted through the PTBD tract for the treatment of post-LT biliary stricture[3-5]. An alternative approach to treating BBS involves the insertion of a removable FC-SEMS through a PTBD tract. In this method, the stent with a distal string is inserted in the conventional direction, and the string is fixed to the skin[9]. This carries a risk of peripheral stent migration along the string, infection through the string tract, and additional PTCS for stent removal[9].
The cause of BBS varies in patients, from post-LT biliary stricture to chronic inflammation[1]. Despite these various causes, a removable FC-SEMS is the preferred treatment for providing stricture resolution with sustained patency and reducing the number of endoscopic sessions[1]. In the present case, where a stricture was inaccessible by ERCP, either multiple plastic stents or an FC-SEMS would be considered to prolong patency. Regarding the number of PTBD sessions, a manually rearranged FC-SEMS attached to a proximal string was selected and deployed through the PTBD tract to facilitate stricture resolution in one session. This case demonstrates that the deployment of an FC-SEMS with a proximal string is a viable option for biliary strictures that are inaccessible by ERCP. Endoscopic ultrasonography (EUS)-guided biliary drainage is also a salvage technique for strictures that are inaccessible by ERCP[1]. In this setting, FC-SEMS with a proximal string can help in EUS-guided antegrade biliary drainage for BBSs.
Traditionally, removable FC-SEMSs with distal strings have been inserted using ERCP. If an FC-SEMS inserted through the PTBD tract can be removed by pulling the string using endoscopy, the stent should be inverted so that the distal string becomes the proximal string before insertion through the tract. As this type of removable FC-SEMS was not available, rearrangement of the FC-SEMS was manually performed immediately before the procedure in the present case. No difficulties were encountered in rearranging the inverted FC-SEMS. Another technical point for consideration is the change in the string direction. During FC-SEMS insertion, the string was directed toward the liver. However, the direction of the string should be changed so that it faces the duodenum with the distal end positioned adjacent to the duodenum for endoscopic removal. To change direction, the FC-SEMS was initially inserted into the third portion of the duodenum and slowly pulled back into the post-LT biliary stricture. As the FC-SEMS was being pulled back, the string spontaneously changed direction.
In summary, a post-LT biliary stricture complicated by obstructive jaundice was treated by the placement of a removable FC-SEMS through a PTBD tract. Initially, PTBD played a central role as a salvage procedure for treating biliary obstruction in post-LT biliary strictures that were inaccessible by ERCP. A removable FC-SEMS inserted through the PTBD tract successfully resolved the stricture in one session. The endoscopic removal of an FC-SEMS with a novel proximal string through the PTBD tract may be a feasible option for the treatment of post-LT biliary strictures that are inaccessible by ERCP.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dragonieri S, Italy S-Editor: Qu XL L-Editor: Wang TQ P-Editor: Yu HG
| 1. | Sato T, Nakai Y, Fujishiro M. Current endoscopic approaches to biliary strictures. Curr Opin Gastroenterol. 2022;38:450-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 2. | Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50:910-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 483] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 3. | Koksal AS, Eminler AT, Parlak E, Gurakar A. Management of biliary anastomotic strictures after liver transplantation. Transplant Rev (Orlando). 2017;31:207-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Fasullo M, Shah T, Zhou H, Siddiqui MS. Post-Transplant Biliary Strictures: An Updated Review. Semin Liver Dis. 2022;42:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Tringali A, Tarantino I, Barresi L, Traina M, Bonato G, Cintolo M, Hassan C, Mutignani M, Adler DG. Multiple plastic versus fully covered metal stents for managing post-liver transplantation anastomotic biliary strictures: a meta-analysis of randomized controlled trials. Ann Gastroenterol. 2019;32:407-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Villa NA, Harrison ME. Management of Biliary Strictures After Liver Transplantation. Gastroenterol Hepatol (N Y). 2015;11:316-328. [PubMed] |
| 7. | Culp WC, McCowan TC, Lieberman RP, Goertzen TC, LeVeen RF, Heffron TG. Biliary strictures in liver transplant recipients: treatment with metal stents. Radiology. 1996;199:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Yoon HK, Sung KB, Song HY, Kang SG, Kim MH, Lee SG, Lee SK, Auh YH. Benign biliary strictures associated with recurrent pyogenic cholangitis: treatment with expandable metallic stents. AJR Am J Roentgenol. 1997;169:1523-1527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Tomishima K, Ishii S, Fujisawa T, Ikemura M, Ushio M, Takahashi S, Yamagata W, Takasaki Y, Suzuki A, Ito K, Haga K, Ochiai K, Nomura O, Saito H, Shibuya T, Nagahara A, Isayama H. Evaluation of the Feasibility and Effectiveness of Placement of Fully Covered Self-Expandable Metallic Stents via Various Insertion Routes for Benign Biliary Strictures. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |