Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8219
Peer-review started: October 6, 2023
First decision: October 17, 2023
Revised: October 27, 2023
Accepted: November 29, 2023
Article in press: November 29, 2023
Published online: December 6, 2023
Processing time: 61 Days and 2.4 Hours
Frostbite is becoming increasingly common in urban environments, and severe cases can lead to tissue loss. The treatment goal is to preserve tissue and function; the sooner appropriate treatment is administered, the more tissue can be saved. However, not every patient with deep frostbite seeks medical care promptly.
We report the case of a 73-year-old male patient who was lost in the wilderness for 2 d due to trauma and confusion. He experienced deep frostbite on multiple fingers. Treatment should not be discontinued for patients with deep frostbite who present after the optimum treatment timing. Bullae that no longer form (bloody) blisters within 24 h of aspiration should be removed. Mucopolysaccharide polysulfate cream has clinical value in frostbite treatment. The patient was transferred to Chinese Academy of Medical Sciences and Peking Union Medical College Hospital 12 h after being rescued. The patient had contraindications for thrombolysis, the most effective treatment, due to intracranial hemorrhage and presenting past the optimum treatment timing. We devised a comprehensive treatment plan, which involved delayed use vasodilators and high-pressure oxygen therapy at day 49 post-injury. We experimented with mucopolysaccharide polysulfate cream to treat the frostbite. The aim of the treatment was to safeguard as much tissue as possible. In the end, the fingers that suffered from frostbite were able to be partially preserved.
The case indicated that patients with severe frostbite who missed the optimal treatment time and had contraindications for thrombolysis could still partially preserve the affected limbs through comprehensive treatment.
Core Tip: Frostbite, increasingly common in urban areas, requires swift treatment for tissue preservation. Not all deep frostbite cases receive prompt medical attention. A 73-year-old male, lost in the wilderness for 2 d post-trauma, presented with deep frostbite on multiple fingers. Despite a 12-h delay, he received comprehensive, delayed treatment at the Chinese Academy of Medical Sciences and Peking Union Medical College Hospital. Contraindications for thrombolysis led to an alternative plan, including extended vasodilator use and high-pressure oxygen therapy from day 49 post-injury. This case emphasizes the vital importance of timely frostbite treatment and offers insights into managing delayed cases with contraindications.
- Citation: Wang XH, Li M, Cheng Y, Wang GJ, Lin GL, Liu WN. Comprehensive treatment of deep frostbite of multiple fingers after trauma: A case report. World J Clin Cases 2023; 11(34): 8219-8227
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8219.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8219
Frostbite is damage caused by the acute freezing of tissues exposed to extremely low temperatures. The severity of the injury depends on the temperature gradient of the skin surface and the duration of exposure. Severe cases can lead to permanent damage or even be life-threatening[1]. In recent decades, the incidence of frostbite has shifted from military personnel to the general population, particularly among those residing in cold environments. Frostbite is more frequent in persons with alcohol use disorder, mental health challenges, those with accidental injuries, and socially disadvantaged groups[2]. Currently, no consistent grading system exists for frostbite. One approach classifies it into first to fourth degrees based on the depth of tissue freezing[3]. For clinical purposes, frostbite is more commonly classified into superficial (grades 1 and 2) and deep frostbite (grades 1 and 2)[4]. Two distinct time periods characterize the response to frostbite: The pre-response period (stage of cold exposure that lasts until the tissue warms up) and the response period, which is further subdivided into the early response period (from tissue rewarming to the first day) and the late-response period (from the second day onward)[5]. Frostbite is best treated with consistent and effective treatment plans during the pre-response and early response periods. However, treatment plans for late-response frostbite vary widely and involve a long treatment cycle with an unclear prognosis. For deep frostbite, the treatment aims to reduce the area of the limb affected and improve limb function as much as possible. Studies have shown that most deep frostbite cases result in amputation[6-8]. Thrombolytic therapy within 24 h of frostbite can significantly reduce tissue damage[9]. Here, we report a case involving severe frostbite of several fingers of a 73-year-old man who had faced trauma and went missing for 48 h.
A 73-year-old man went missing following a car accident. When the rescue team found him, he had severe facial swelling, purple bruising, and scabbing. He could not open his eyes voluntarily, had frozen hands, and could not make a fist.
On January 18, 2023, at 06:00 PM, the patient was admitted to our emergency department after he had been missing for 2 d following a car accident. He experienced retrograde amnesia and impaired localization of function after being hit on the head on January 16, 2023, at around 03:00 PM. He went missing and was found by a rescue team in a neighboring village after 2 d. The incident occurred in winter, with the lowest nighttime temperature reaching -18 ℃. Upon presentation at our emergency department, the patient underwent a head computed tomography (CT) scan, which revealed a left frontal lobe contusion, a small hematoma, left frontal bone and bilateral orbital fractures, and a subarachnoid hemorrhage, suggesting contraindication for thrombolysis. Additionally, the patient had frostbite on all ten fingers and a soft tissue contusion in the left orbit. The patient had no history of smoking or drinking and no other medical history except for a self-reported untreated twist injury on the right ring and little fingers. The medical history was confirmed by his daughter.
The patient was dehydrated and weak, having not drunk or eaten in the 2 d when he was missing. He fell asleep in a thicket and was found wearing a cotton hat, clothes, and shoes, with only his hands exposed. When the rescue team found the patient, he had severe facial swelling, purple bruising, and scabbing. He could not open his eyes voluntarily, had frozen hands, and could not make a fist. Due to limited medical treatment in the area, the patient was transported by ambulance for 8 h. During this time, he received peripheral intravenous glucose and sodium chloride, and his hands were placed under his family member’s armpits for rewarming.
The patient was admitted to the general surgery ward at night and received an intramuscular injection of 250 IU tetanus human immunoglobulin. Laboratory tests were immediately performed; the abnormal results are listed in Table 1.
| Item | Value | Reference range |
| Lymphocytes (%) | 6.2 | 20.0-40.0 |
| Neutrophils (%) | 85.6 | 50.0-75.0 |
| White blood cells (L) | 9.95 × 109 | 3.50-9.50 |
| Red blood cells (L) | 3.14 × 1012 | 4.00-5.50 |
| Hemoglobin (g/L) | 115 | 120-160 |
| Prothrombin time (s) | 12.9 | 10.4-12.6 |
| D-dimer (mg/L FEU) | 3.18 | 0-0.55 |
| C-reactive protein | 30.40 | ≤ 8.00 |
| Amylase (U/L) | 537 | 35-135 |
| Total bilirubin (μmol/L) | 43.6 | 5.1-22.2 |
| Direct bilirubin (μmol/L) | 16.3 | ≤ 6.8 |
| Myoglobin (μg/L) | 1043 | ≤ 110 |
| Creatine kinase (U/L) | 3022 | 24-195 |
| Creatine kinase-mass (μg/L) | 43.3 | ≤ 5.0 |
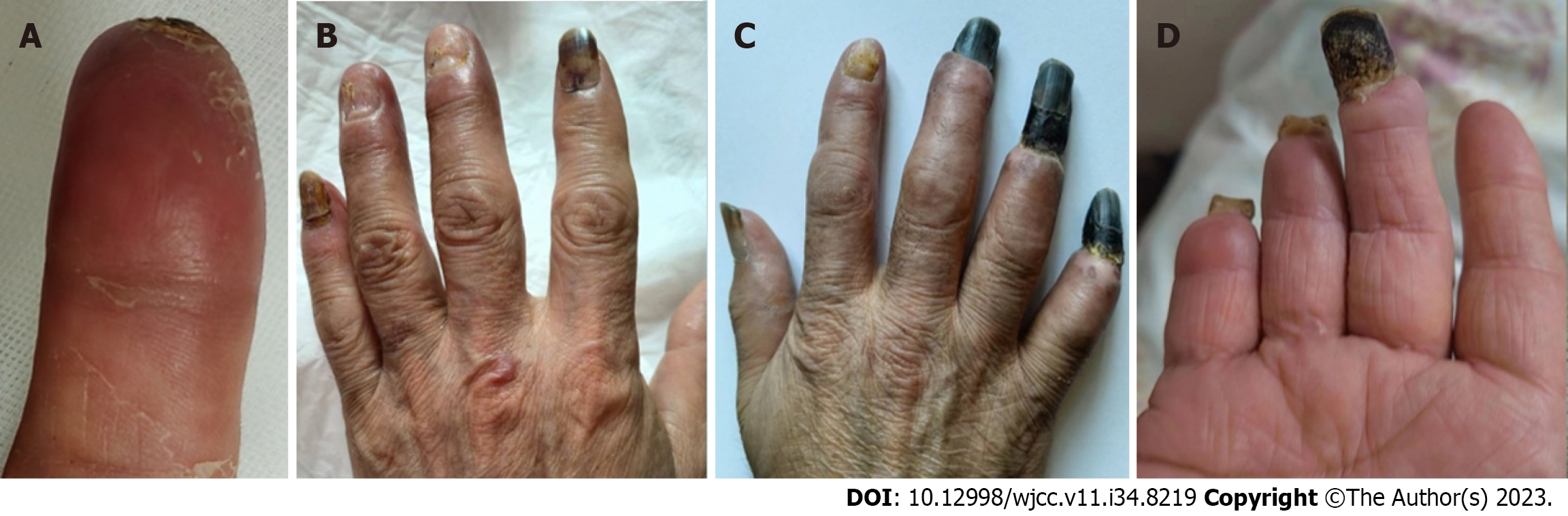
Physical examination revealed swollen joints in the patient’s hands. His fingers were frostbitten to varying degrees, with all ten fingers having cool skin and dark purple fingertips. Severe water blisters were observed on all five fingers of the right hand. The patient’s fingers were cleaned and wrapped with gauze after the ulcer was cleaned and then covered with a warm blanket. The patient received continuous intravenous fluid therapy and ertapenem. The following morning, the patient’s hands were severely swollen. All ten fingers were clubbed with large, tense, and bloody blisters (Figure 1A and B). The first, second, and fifth fingers of the left hand and the first finger of the right hand had superficial frostbites, whereas the third and fourth fingers of the left hand and the second to fifth fingers of the right hand had deep frostbites. We conducted a multidisciplinary consultation with the Departments of Plastic Surgery, Dermatology, and Vascular Medicine, and a wound specialist nurse intervened in the treatment.
The patient had no history of smoking or drinking and no other medical history except for a self-reported untreated twist injury on the right ring and little fingers.
Physical examination revealed swollen joints in the patient’s hands. His fingers were frostbitten to varying degrees, with all ten fingers having cool skin and dark purple fingertips. Severe water blisters were observed on all five fingers of the right hand.
Laboratory examinations showed the following results: Lymphocytes (%) 6.2 (reference range: 20.0-40.0); C-reactive protein 30.40 (≤ 8.00) mg/L; neutrophils (%) 85.6 (50.0-75.0); amylase 537 (35-135) U/L; white blood cell count 9.95 (3.50-9.50) × 109/L; total bilirubin 43.6 (5.1-22.2) μmol/L; red blood cell count 3.14 (4.00-5.50) × 1012/L; direct bilirubin 16.3 (≤ 6.8) μmol/L; hemoglobin 115 (120-160) g/L; myoglobin 1043 (≤ 110) μg/L; prothrombin time 12.9 (10.4-12.6) s; creatine kinase 3022 (24-195) U/L; D-dimer 3.18 (0-0.55) mg/L fibrinogen equivalent units; creatine kinase-mass 43.3 (≤ 5.0) μg/L.
Upon presentation at Chinese Academy of Medical Sciences and Peking Union Medical College Hospital emergency department, the patient underwent a head CT scan, which revealed a left frontal lobe contusion, a small hematoma, left frontal bone and bilateral orbital fractures, and a subarachnoid hemorrhage.
Magnetic resonance imaging (MRI) revealed a small effusion in the second to fifth metacarpophalangeal joints on the left side, subcutaneous soft tissue swelling on the palmar side of the left hand, and cystic changes in the proximal phalanx of the middle finger of the left hand. Multiple cystic lesions were observed at the proximal and distal ends of the first metacarpal bone and the distal end of the second proximal phalanx of the right hand. Effusion was observed in the second, third, and fourth metacarpophalangeal joints, and soft tissue swelling was observed around the second and third metacarpophalangeal joints.
Traumatic brain injury and deep frostbite of multiple fingers.
On day 1, after iodine disinfection, a suction bubble solution and low-position drainage were applied to protect the blistered skin. The blister fluid on the left hand was yellow, clear, and transparent, whereas the blister fluid on the right hand was slightly blood-tinged, clear, and transparent. The patient’s hands were soaked in 50 mL of chlorhexidine acetate solution and 1000 mL of warm water at 37 ℃-40 ℃ twice daily. After a warm water bath, mupirocin cream was externally applied, and the ulcer was wrapped with gauze. The patient reported no numbness or pain.
On day 2, the water-like blisters on the left hand and blood blisters on the right hand were still present, and the purple color had improved. The edges retreated towards the fingertips. The blister fluid was suctioned daily, and mupirocin and burn moist cream (MeiBao, MEBO) were externally applied. The patient reported experiencing sensation when his ten fingers were scraped with a cotton swab (Supplementary Figure 1). When the patient went to the examination room for CT, he accidentally injured the skin on their right index finger. The comprehensive treatment plan is highlighted in Table 2.
| Date | Therapeutic process |
| Day 2 | The wound appeared red and well-circumscribed. After applying a thick layer of bacitracin ointment, it was covered with petroleum gauze, and the dressing was changed daily |
| Day 3-6 | Epidermal growth factor gel, silver ion gel, and povidone-iodine were used to cover the calcium alginate dressing to prevent wound infection. Ulcer oil gauze and plain gauze were wrapped around the wound (Figure 1C and D) |
| Day 7 | Epithelialization of the wound was performed (Figure 2C). |
| Day 9 | The newly regenerated epidermis underwent crust formation (Figure 2D) |
| Days 12-16 | The scab gradually shed off from initial formation to complete detachment (Figure 3D) |
On day 3, the patient could not undergo tissue plasminogen activator (tPA) treatment due to anticoagulation contraindications and was administered an alprostadil injection (10 μg IV qd) for 12 consecutive days. On day 4, he was also orally administered 60 mg of loxoprofen sodium every 12 h. The tips of the third, fourth, and fifth fingers of the right hand turned black (Figure 1C). On day 5,there was no sign of infection on the index finger of the right hand (Figure 1D). The blister fluid was suctioned daily until it disappeared on day 7. The black area gradually expanded near the first finger joint. The frostbite on the tips of the left fingers gradually formed a dark red soft shell (Supplementary Figure 2).
On day 8, mucopolysaccharide polysulfate cream was applied to the abnormally colored skin of the ten fingers, and the patient was administered oxygen via a nasal cannula at a rate of 2 L/min. The patient's fingertips were dry, wrinkled, and had reduced volume (Figure 2A). Therefore, total parenteral nutrition was administered. On day 9, the patient took mecobalamin (0.5 g) orally three times daily, and we found that the new epithelium of the right index finger had turned into a black scab (Figure 2B). On day 12, the chlorhexidine acetate warm water bath was discontinued, and Sanyrenewas externally applied (Figure 2C).
On day 13, the patient underwent MRI and radiography of both hands. The radiographic image was normal. The MRI revealed a small effusion in the second to fifth metacarpophalangeal joints on the left side, subcutaneous soft tissue swelling on the palmar side of the left hand, and cystic changes in the proximal phalanx of the middle finger of the left hand. Multiple cystic lesions were observed at the proximal and distal ends of the first metacarpal bone and the distal end of the second proximal phalanx of the right hand. Effusion was observed in the second, third, and fourth metacarpophalangeal joints, and soft tissue swelling was observed around the second and third metacarpophalangeal joints.
On day 15, the black and hard scabs on the first joint of the back of the left hand were removed, and the patient could make a fist. The patient reported occasional pain in the little finger of the right hand and was administered 50 mg of etoricoxib tablets orally every 12 h. On day 16, the scabs on the back and fingertip of the left hand and the index finger of the right hand were removed after soaking them in warm water (Figure 2D; Supplementary Figure 3), and subsequently, the patient was discharged.
After discharge, the dry and hard scabs at the edges were gradually removed by the patient, and the nails gradually fell off (Figure 3A). On day 22, the broken index finger on his right hand has healed (Figure 3B). By day 27, the patient experienced noticeable constriction and swelling in the ring and little fingers of the right hand. The blackened edge of the scab was removed, revealing fresh tissue at the bottom. The edge of the black scab was shaved using a blade to relieve pressure (Supplementary Figure 4). Between day 49 and day 67, the patient underwent 20 sessions of hyperbaric oxygen therapy (HBOT) (Figure 3C). On day 90, the tips of the third finger of the right hand turned black and were deformed, necessitating a planned self-amputation (Supplementary Figure 5). On day 180, the tips of the fourth and fifth fingers of the right hand were amputated (Figure 3D).
Historically, frostbite injuries have occurred primarily during large-scale military operations. However, in recent years, it has impacted individuals living in cold environments in peaceful areas[1]. In China, people residing in temperate plains rarely experience frostbites[5,8]. Consequently, many hospitals, including the one mentioned in this report, lack established frostbite treatment protocols and experience, resulting in treatment delays for patients. On the second day after the patient was admitted to our hospital, we organized a multidisciplinary consultation involving neurosurgeons, orthopedics, vascular surgeons, dermatologists, plastic surgeons, general surgeons, and wound care nurses to devise a treatment plan led by the wound care nurses. We believe that treatment should not be discontinued for patients with deep frostbite who present after the optimum treatment timing. Bullae that no longer form (bloody) blisters within 24 h of aspiration should be removed. Mucopolysaccharide polysulfate cream has clinical value in frostbite treatment.
Frostbites can cause both cellular and ischemic vascular damage. Continuous freezing of body tissues leads to the formation of ice crystals in the extracellular fluid, which damages the cell membrane and alters the osmotic pressure of the cells, resulting in cell damage. When exposed to cold conditions, the body undergoes a physiological reaction to protect the limbs from cold-induced damage through a system of alternating vasoconstriction and vasodilation processes, known as the “hunting reaction”. However, this physiological reaction causes severe damage, including progressive thrombosis and tissue ischemia[2,3]. When formulating a treatment plan, it is essential to determine the patient’s exposure time to the cold. Unfortunately, in this case, the patient was lost for 2 d, and the exposure time to cold could not be determined. Therefore, we calculated the frostbite time and exposure time to the cold from the first day when he went missing until the patient was sent to the ambulance, which was approximately 36 h. The day of admission was designated as day 0 after the frostbite.
Unlike other skin injuries, the extent of frostbite gradually becomes apparent upon tissue rewarming, and the initial photographs do not show the extent of the injury[10]. Injuries are clinically classified into four grades according to the depth of the tissue frostbite[3]. Grade 1 injuries involve only the superficial skin layer frostbite, exhibiting white spots at the center surrounded by redness. Grade 2 injuries involve full-thickness skin freezing, resulting in the development of large clear blisters with redness and swelling around them within 24 h of rewarming. Grade 3 injuries involve subcutaneous tissue freezing, leading to tissue necrosis, hemorrhagic blisters, bluish-gray wax-like skin appearance, and black scab formation. Grade 4 injuries involve muscle, tendon, and bone freezing, resulting in the formation of hard black scabs and tissue mummification, ultimately necessitating amputation[3,4,11]. Another simple grading system includes superficial (grades 1-3) and deep injuries (grades 3 and 4). Superficial injuries rarely involve tissue loss, whereas deep injuries result in more extensive tissue loss and a generally poor prognosis[12]. Studies have shown that fluorescence microscopy angiography in the emergency department can rapidly identify perfusion defects after frostbite[13]. The accuracy of evaluating amputation levels can reach 84% when Technetium-99 bone scanning is performed on the second day after rewarming from frostbite[14]. Unfortunately, only an MRI scan was performed in this case.
Utilizing a water bath at 37 ℃-39 ℃ is generally recommended to prevent further damage to soft tissues during the rewarming stage for frostbite on-site[12]. Currently, there is no evidence-based protocol for frostbite hydrotherapy regarding the temperature, time, frequency, and duration after rewarming. In the present case, the patient underwent hydrotherapy on the first day after admission. The hydrotherapy treatment plan involved soaking the affected area in 1000 mL of warm water at 37 ℃-40 ℃ with a chlorhexidine acetate solution for 20 min, twice daily, for 12 d. Although no infections occurred during this treatment, its impact on promoting frostbite rehabilitation was found to be insignificant.
Frostbite is a thrombotic injury, and an increasing number of medical teams are attempting to use thrombolysis within 6-24 h after frostbite to salvage tissue in affected patients[9,15]. Early treatment with tPA can prevent amputation in 85%-90% of cases[16]. The Helsinki frostbite management protocol recommends the combined use of tPA and iloprost (a prostacyclin analog) to improve the prognosis of severe frostbite[17]. Cauchy et al[7] found that iloprost treatment alone for 8 d effectively prevents tissue loss.
The combination of aspirin and prostacyclin for stage 3 or higher frostbite is recommended, especially within 48-72 h of rewarming[18,19]. However, this patient had contraindications for thrombolysis due to combined trauma and intracranial hemorrhage; therefore, the thrombolysis treatment plan was abandoned. Iloprost was unavailable due to the limitations of the medicine used in our hospital. Consequently, prostaglandin E1, which is another vasodilator, was administered at a dosage of 10 µg/d approximately 80 h after rewarming.
The formation of blisters represents a distinct characteristic in the degree of the injury. Drainage is recommended because blister fluid contains high concentrations of anti-inflammatory substances, such as prostaglandin F2 alpha and thromboxane A2, which prevent the healing of the lower skin layers. However, controversy exists regarding the treatment of bleeding blisters, as there is a risk of bleeding during debridement[1,4]. In this case, both transparent and bleeding blisters were aspirated, and the blister skin was preserved. However, on the second day following the frostbite incident, the blistered skin on the patient's right index finger was accidentally torn during an outpatient CT examination. After using anti-infective dressings for 7 d, a black scab formed on the newly generated epidermis of the patient’s right index finger. The scab eventually detached, and the finger completely healed without any tissue loss. Blood-blistered skin on the third, fourth, and fifth fingers of the same hand also developed into hard black scabs. On day 24, the patient experienced significant constriction pain in the fourth and fifth fingers of the right hand. Subsequently, on day 26, the hard black scab near the junction was thinned using a blade, leading to a significant reduction in the patient’s pain. Simultaneously, the hard black scab was divided into two layers, with dry blood scabs in between. This observation may indicate that third-degree frostbite had damaged the dermis layer, and despite the newly formed epidermis, the skin layer turned black and scabbed. This scab combined with the dry blistered skin, forming a hard black scab that hindered the growth of new tissue. Therefore, if no new blisters formed within 24 h of aspiration treatment, debridement of the blistered skin would have been considered.
The 2019 Clinical Practice Guidelines[12] for the prevention and treatment of frostbite released by the Wilderness Medical Society suggests that the topical application of aloe vera gel can reduce the formation of prostaglandins and thromboxanes, thereby improving frostbite outcomes. However, aloe vera gel only benefits superficial injuries and does not penetrate deeply into tissues. In this case, the mucopolysaccharide polysulfate cream was used for external treatment, marking the first report of its application in frostbite treatment. The main active ingredient of mucopolysaccharide polysulfate cream is mucopolysaccharide polysulphate (MPS), which is chemically similar to heparin, being described as heparin-like. It accelerates the recovery of the permeability barrier and hydration of the stratum corneum, thus exerting antithrombotic and anti-inflammatory effects[20]. The study by Livaoğlu et al[21] showed that local application of mucopolysaccharide polysulfate cream could improve the survival rate of rat skin flaps. MPS can penetrate the human skin, with trace amounts entering the circulation, thereby affecting the coagulation system. In this case, the mucopolysaccharide polysulfate cream was externally applied for 14 consecutive days after the patient’s intracranial hemorrhage had stabilized (day 8). Mucopolysaccharide polysulfate cream promotes the resolution of edema and bruises[22]. Mucopolysaccharide polysulfate cream is used to treat venous inflammation at our hospital. Further investigation into the potential therapeutic effects of early mucopolysaccharide polysulfate cream application post-frostbite rewarming should be explored.
HBOT is an important adjunct for frostbite treatment. During HBOT, patients inhale high concentrations of oxygen within a pressurized chamber. This oxygen dissolves in the plasma and increases the oxygen partial pressure to over 20 times that of breathing indoor air at normal atmospheric pressure, resulting in hyperoxygenated plasma. This hyperoxygenated plasma can then be transported to hypoxic or ischemic tissues, promoting angiogenesis, reducing edema, and increasing the basal metabolic rate[23]. Masters et al[24] reported a 90% survival rate in a patient with severe frostbite after 20 sessions of HBOT combined with thrombolysis. Additionally, Kemper et al[25] reported a case where delayed HBOT treatment (21 d) resulted in positive outcomes for a patient with deep frostbite in the toes. However, HBOT for frostbite has potential side effects, including ear barotrauma, nausea, vomiting, anxiety, oxygen toxicity, and myopia changes[26]. Therefore, its application should be carefully considered based on the patient’s condition. In this case, the patient received HBOT on day 49 after the frostbite incident and reported significant pain in the affected finger during the treatment period, possibly related to increased blood circulation at the injury site. Therefore, delayed HBOT may be beneficial for wound healing; this merits further investigation.
Treatment timing plays a crucial role in frostbite recovery, and prompt treatment should be provided for deep frostbite with a risk of tissue loss. For blisters that are no longer filled within 24 h, de-roofing of the blisters can be attempted while maintaining a moist wound environment to prevent infection. Amputation should be carefully considered, as some medical institutions lack the necessary equipment to detect tissue perfusion at the injury site. Conservative observation of dry black scabs may reveal viable tissues, warranting patients with such scabs to await self-amputation of necrotic tissues. Mucopolysaccharide polysulfate cream has application value in frostbite treatment and can be externally applied to intact frostbite tissues after rewarming. This case provides insights into managing deep frostbite with contraindications for thrombolysis or missed optimal treatment timing. During the 6-mo follow-up post-injury, we found that the patient was anxious due to the uncertainty of the time of self-amputation. Attention should be paid to the patient’s psychological state.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH, Indonesia; Ding WW, China; Augustin G, Croatia S-Editor: Qu XL L-Editor: Wang TQ P-Editor: Guo X
| 1. | Sheridan RL, Goverman JM, Walker TG. Diagnosis and Treatment of Frostbite. N Engl J Med. 2022;386:2213-2220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Regli IB, Strapazzon G, Falla M, Oberhammer R, Brugger H. Long-Term Sequelae of Frostbite-A Scoping Review. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Joshi K, Goyary D, Mazumder B, Chattopadhyay P, Chakraborty R, Bhutia YD, Karmakar S, Dwivedi SK. Frostbite: Current status and advancements in therapeutics. J Therm Biol. 2020;93:102716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Persitz J, Essa A, Ner EB, Assaraf E, Avisar E. Frostbite of The Extremities - Recognition, Evaluation and Treatment. Injury. 2022;53:3088-3093. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Lipatov K, Komarova E, Asatryan A, Melkonyan G, Solov'eva E, Gorbacheva I, Vorotyntsev A, Maximov A, Shevchuk A. Frostbite of the upper extremities: Hot issues in diagnosis and surgical treatment (review). Burns. 2022;48:1279-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Lorentzen AK, Penninga L. Frostbite-A Case Series From Arctic Greenland. Wilderness Environ Med. 2018;29:392-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Cauchy E, Cheguillaume B, Chetaille E. A controlled trial of a prostacyclin and rt-PA in the treatment of severe frostbite. N Engl J Med. 2011;364:189-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 8. | Xiao Y, Hao D, Xin Y, Jiang X. A Tibetan adolescent girl suffered frostbite on the journey of pilgrimage: A case report. Chin J Traumatol. 2022;25:184-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Hickey S, Whitson A, Jones L, Wibbenmeyer L, Ryan C, Fey R, Litt J, Fabia R, Cancio L, Mohr W, Twomey J, Wagner A, Cochran A, Bailey JK. Guidelines for Thrombolytic Therapy for Frostbite. J Burn Care Res. 2020;41:176-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Van Wicklin SA. Frostbite 101. Plast Aesthet Nurs (Phila). 2023;43:64-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Laskowski-Jones L, Jones LJ. Frostbite: Don't be left out in the cold. Nursing. 2018;48:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | McIntosh SE, Freer L, Grissom CK, Auerbach PS, Rodway GW, Cochran A, Giesbrecht GG, McDevitt M, Imray CH, Johnson EL, Pandey P, Dow J, Hackett PH. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Frostbite: 2019 Update. Wilderness Environ Med. 2019;30:S19-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 13. | Raleigh SM, Samson M, Nygaard R, Endorf F, Walter J, Masters T. Bedside Fluorescence Microangiography for Frostbite Diagnosis in the Emergency Department. West J Emerg Med. 2022;23:872-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Handford C, Thomas O, Imray CHE. Frostbite. Emerg Med Clin North Am. 2017;35:281-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Lorentzen AK, Davis C, Penninga L. Interventions for frostbite injuries. Cochrane Database Syst Rev. 2020;12:CD012980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Shenaq DS, Beederman M, O'Connor A, Teele M, Robinson MR, Gottlieb LJ. Urban Frostbite: Strategies for Limb Salvage. J Burn Care Res. 2019;40:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Lindford A, Valtonen J, Hult M, Kavola H, Lappalainen K, Lassila R, Aho P, Vuola J. The evolution of the Helsinki frostbite management protocol. Burns. 2017;43:1455-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Pandey P, Vadlamudi R, Pradhan R, Pandey KR, Kumar A, Hackett P. Case Report: Severe Frostbite in Extreme Altitude Climbers-The Kathmandu Iloprost Experience. Wilderness Environ Med. 2018;29:366-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Irarrázaval S, Besa P, Cauchy E, Pandey P, Vergara J. Case Report of Frostbite with Delay in Evacuation: Field Use of Iloprost Might Have Improved the Outcome. High Alt Med Biol. 2018;19:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Yao Y, Guo P, Feng X, Shen C, Huang J, Zhang J, Elias PM, Hu L, Man MQ. A topical heparinoid-containing product improves epidermal permeability barrier homeostasis in mice. Exp Dermatol. 2019;28:956-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Livaoğlu M, Kerimoğlu S, Sönmez B, Livaoğlu A, Karaçal N. The effect of Hirudoid on random skin-flap survival in rats. J Plast Reconstr Aesthet Surg. 2010;63:1047-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Rostami K, Shahaboddin MA, Niazi F, Karimi Rouzbahani A, Nadri S, Mahmoudvand H. The Effect of Hirodoid Cream on Ecchymosis and Edema around Eyes after Rhinoplasty. World J Plast Surg. 2020;9:128-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Kahle AC, Cooper JS. Hyperbaric Physiological And Pharmacological Effects of Gases. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 24. | Masters T, Omodt S, Gayken J, Logue C, Westgard B, Hendriksen S, Walter J, Nygaard R. Microangiography to Monitor Treatment Outcomes Following Severe Frostbite Injury to the Hands. J Burn Care Res. 2018;39:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Kemper TC, de Jong VM, Anema HA, van den Brink A, van Hulst RA. Frostbite of both first digits of the foot treated with delayed hyperbaric oxygen:a case report and review of literature. Undersea Hyperb Med. 2014;41:65-70. [PubMed] |