Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8212
Peer-review started: October 3, 2023
First decision: November 1, 2023
Revised: November 11, 2023
Accepted: November 27, 2023
Article in press: November 27, 2023
Published online: December 6, 2023
Processing time: 63 Days and 17.7 Hours
Hemophagocytic lymphohistiocytosis (HLH) is a rare but life-threatening condition. It is an immune-mediated disease that has a wide range of causes, elicits a hyperinflammatory response, and results in multiple organ damage. Clinical presentations vary, and in some cases, jaundice occurs as the first symptom.
We report the case of a 71-year-old female patient who presented with jaundice. She was admitted to our hospital because of the occurrence of “jaundice for half a month”, and upon examination, obstructive jaundice with choledocholithiasis and gallstones was suggested. Cholecystectomy and choledocholithotomy were performed. However, the jaundice did not improve after surgery. We found splenomegaly, cytopenia, hypertriglyceridemia, hypofibrinogenemia, and elevated ferritin. Bone marrow biopsy revealed hemophagocytosis. Later, cardiac arrest occurred when she returned 3 wk after the surgery. We considered that HLH was triggered by septic shock. The patient’s condition deteriorated rapidly, with multiple organ dysfunction and severe gastrointestinal bleeding. Corticosteroid therapy and symptomatic treatment failed to save her life.
Jaundice rarely presents as the first symptom in HLH patients. The HLH in this case was triggered by septic shock with jaundice as the first symptom. Clinicians should try hard to reduce missed diagnoses and misdiagnoses.
Core Tip: We report the case of a 71-year-old female patient who presented with jaundice. Obstructive jaundice with choledocholithiasis and gallstones was suggested. Then, we found splenomegaly, cytopenia, hypertriglyceridemia, hypofibrinogenemia, and elevated ferritin. Bone marrow biopsy revealed hemophagocytosis. Later, cardiac arrest occurred when she returned after the surgery. We considered that hemophagocytic lymphohistiocytosis (HLH) was triggered by septic shock. The patient’s condition deteriorated rapidly, with multiple organ dysfunction. Corticosteroid therapy and symptomatic treatment failed to save her life. Jaundice rarely presents as the first symptom in HLH patients. Elevated direct bilirubin was associated with prognosis. Clinicians should try to reduce missed diagnoses and misdiagnoses.
- Citation: Wang DD, Wu S, Kong BB, Song LL. Hemophagocytic lymphohistiocytosis with jaundice as first manifestation: A case report. World J Clin Cases 2023; 11(34): 8212-8218
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8212.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8212
Hemophagocytic lymphohistiocytosis (HLH) is a syndrome of immunomodulatory abnormalities caused by aberrant activation of lymphocytes, monocytes, and macrophages, which release a large amount of inflammatory cytokines, eliciting an excessive inflammatory response. HLH can be classified as primary or secondary. This rapidly progressive disease has a low incidence, but the case fatality rate is high, with a more than 50% mortality rate in severe patients. Therefore, early recognition is crucial to improve the survival of patients with this disorder. We report a patient with HLH who presented with jaundice as the first symptom.
A 71-year-old woman was admitted to our emergency department after experiencing jaundice for half a month and was admitted to the hepatological surgery department in the first stage on February 7, 2023. She was admitted to the emergency department again 3 wk after receiving surgery for cardiac arrest on March 2, 2023.
First stage: In the previous 2 wk prior to her first admission to the hospital, the patient found that her skin and sclera turned yellow, accompanied by chills, but without fever. Obstructive jaundice was considered and treated with medication. However, the treatment did not work, and her jaundice worsened. Therefore, she was admitted to our hospital.
Second stage: Three weeks later, the patient returned to the hepatobiliary surgery department for follow-up. The patient entered cardiac arrest and was admitted to the emergency department.
The patient had a history of gallstones and choledocholithiasis.
The patient had no remarkable personal or family history.
The physical examination revealed a temperature of 37.1°C, pulse of 56 beats per minute, respiration rate of 23 breaths per minute, and blood pressure measured at 163/99 mmHg. Her skin and sclera were yellow, her abdomen was soft, with no tenderness or rebound pain, and Murphy’s sign was negative.
The results of a routine blood test were as follows: White blood cell count 4.67 × 109 /L; hemoglobin 153 g/L; and platelet count 127 × 109 /L. The biochemical test results were as follows: Alanine aminotransferase 309.4 U/L; aspartate aminotransferase 313.1 U/L; total bilirubin 193.9 μmol/L; direct bilirubin 162.4 μmol/L; albumin 32.2 g/L; cholinesterase 4739 U/L; blood urea nitrogen 4.4 mmol/L; creatinine 48 μmol/L; lactate dehydrogenase 419 U/L. Tumor markers were assessed as follows: Carbohydrate antigen-153 26.5 U/mL; alpha-fetoprotein 100.57 ng/mL; carbohydrate antigen-125 77.2 U/mL. Coagulation function results were as follows: Prothrombin time 14.3 s; prothrombin activity 59.2%; activated partial thromboplastin time 35 s; fibrinogen 1.07 g/L; D-dimer 1.19 mg/L; fibrinogen degradation products 3.59 mg/L. The myocardial enzyme series values were within normal limits.
Magnetic resonance cholangiopancreatography showed gallstones with cholecystitis, and there were stones in the common bile duct. The common bile duct was mildly dilated. The spleen was also enlarged.
After the patient entered cardiac arrest and was admitted to emergency, imaging examinations were as follows: Acute cerebrovascular lesions were not identified via head computed tomography(CT); chest CT indicated inflammation in the lower lobe of the right lung; abdominal CT showed no dilation of bile ducts inside or outside the liver, abnormal density, or splenomegaly.
The patient’s liver did not function normally since she was admitted to our emergency. Combined with the imaging results and elevated aminotransferases, gallstones with cholecystitis were considered. The patient underwent laparoscopic cholecystectomy and common bile duct exploration. During the operation, it was revealed that the gallbladder wall was hyperemic and edematous, and the common bile duct was widened, with a diameter of approximately 12 mm. The stones in the common bile duct were removed completely, and the T-tube was drained. The average drainage from the T-tube was 305 mL per day.
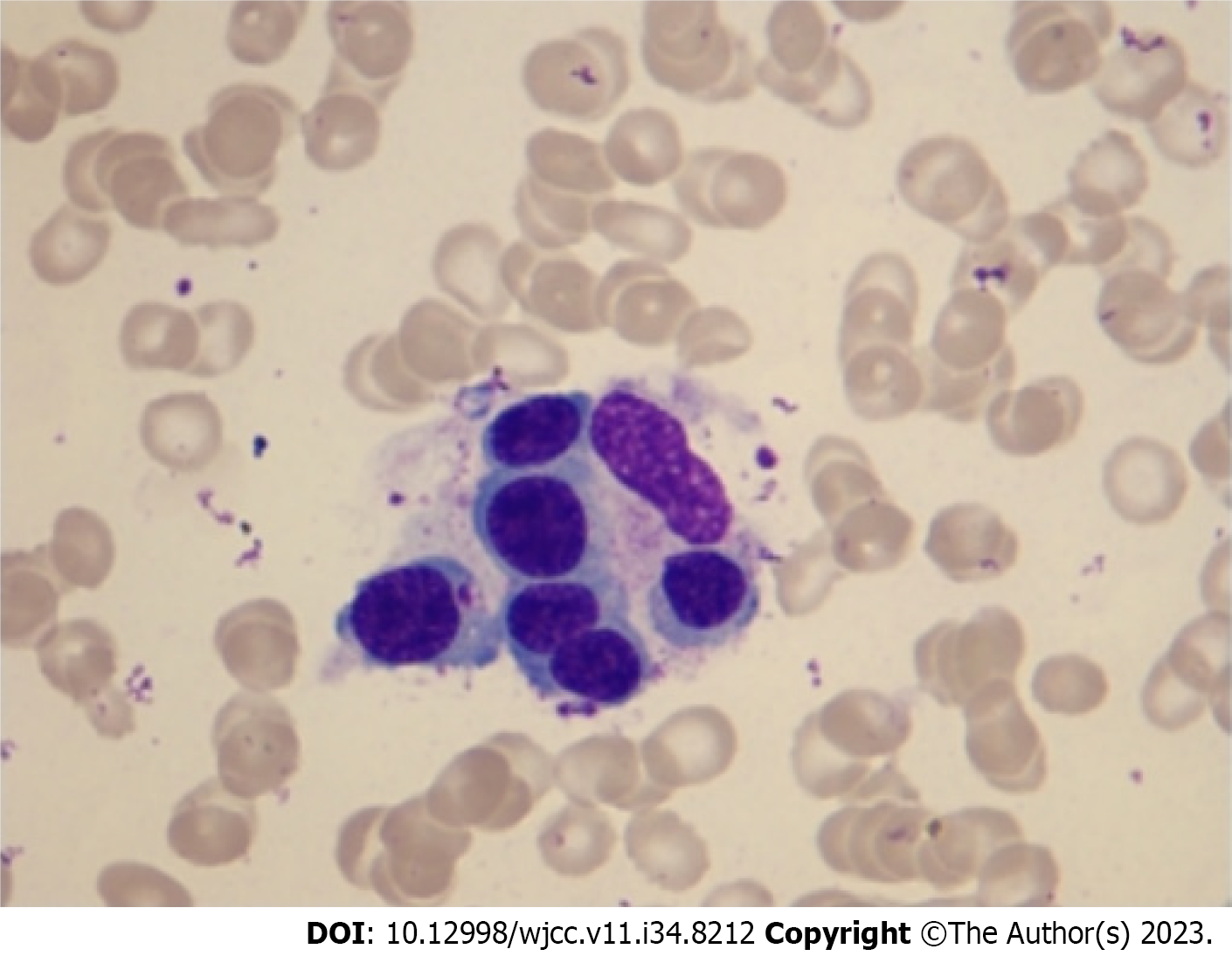
However, the jaundice worsened, and elevations in direct bilirubin were observed (Table 1). Other laboratory chemistry findings were as follows: Cytopenia affecting three lineages in the peripheral blood, hypertriglyceridemia, and hypofibrinogenemia. Re-examination of magnetic resonance cholangiopancreatography did not indicate dilation or obstruction in the intrahepatic and extrahepatic bile ducts. A series of tests, such as bone marrow morphology tests, were completed after hematologist consultation, and the patient was discharged from the hospital. Other relevant results were as follows: Ferritin 3881 μg/L; hemophagocytosis was found in the bone marrow (Figure 1); and normal results for immunoglobulin, complement, antinuclear antibodies, extractable nuclear antibodies, thyroid function, human parvovirus B19 (DNA), cytomegalovirus (nucleic acid), and Epstein–Barr virus (nucleic acid). We informed the patient's family that further diagnosis and treatment would be needed, and they intended to go to another hospital. When she returned to the hepatobiliary surgery department for follow-up, cardiac arrest occurred.
| Item | Feb. 7 | Feb. 10 | Feb. 14 | Feb. 21 | Mar. 2 | Mar. 3 | Mar. 5 | Mar. 8 |
| Hb (g/L) | 153 | 126 | 108 | 84 | 59 | 88 | 35 | 27 |
| WBC (× 109/L) | 4.67 | 3.36 | 6.24 | 2.07 | 38.68 | 19.79 | 2.47 | 7.2 |
| PLT (× 109/L) | 127 | 88 | 88 | 71 | 211 | 143 | 20 | 8 |
| ALT (U/L) | 309.4 | 205 | 102.2 | 36 | 78.2 | 183.5 | 105.1 | 409.6 |
| AST (U/L) | 313.1 | 215 | 117.4 | 55.3 | 265.4 | 871.2 | 367.6 | 2215 |
| TBIL (μmol/L) | 193.9 | 131.2 | 94 | 222.5 | 425.2 | 521.2 | 355.2 | 245 |
| DBIL (μmol/L) | 162.4 | 112.7 | 81 | 174.8 | 373.3 | 422.6 | 276.9 | 169.5 |
| PTA (%) | 68.2 | 59.2 | 70 | 67.3 | 22.5 | 28.3 | 35.4 | 8.3 |
| Cre (μmol/L) | 48 | 40 | 55 | 31 | 118 | 73 | 58 | 117 |
| LDH (U/L) | 419 | 367 | 245 | 413 | 793 | 1440 | 1182 | 3753 |
| Ferritin (μg/L) | - | - | - | 3881.0 | - | - | > 8000 | - |
| TG (mg/dL) | - | 2.89 | 2.38 | - | - | - | - | - |
| Fib (g/L) | 1.05 | 1.07 | 2.04 | 1.58 | 1.49 | 1.34 | 0.8 | 0.74 |
We considered septic shock, with a high possibility of biliary infection. Imipenem/cilastatin sodium (1 g per 8 h) was administered as an anti-infective, as well as for organ support. Considering that the T-tube was in place, T-tube drainage was continued. Later, peripheral blood culture and bile culture results indicated the presence of Klebsiella acidogenes (treated with cefoperazone sodium/sulbactam sodium, minimum inhibitory concentration 8 mg/L) and Enterococcus faecium with high levels of aminoglycoside resistance (HLAR) (treated with vancomycin, minimum inhibitory concentration 0.5 mg/L). According to the results regarding drug sensitivity, the anti-infection regimen was adjusted to cefoperazone sodium/sulbactam sodium combined with vancomycin.
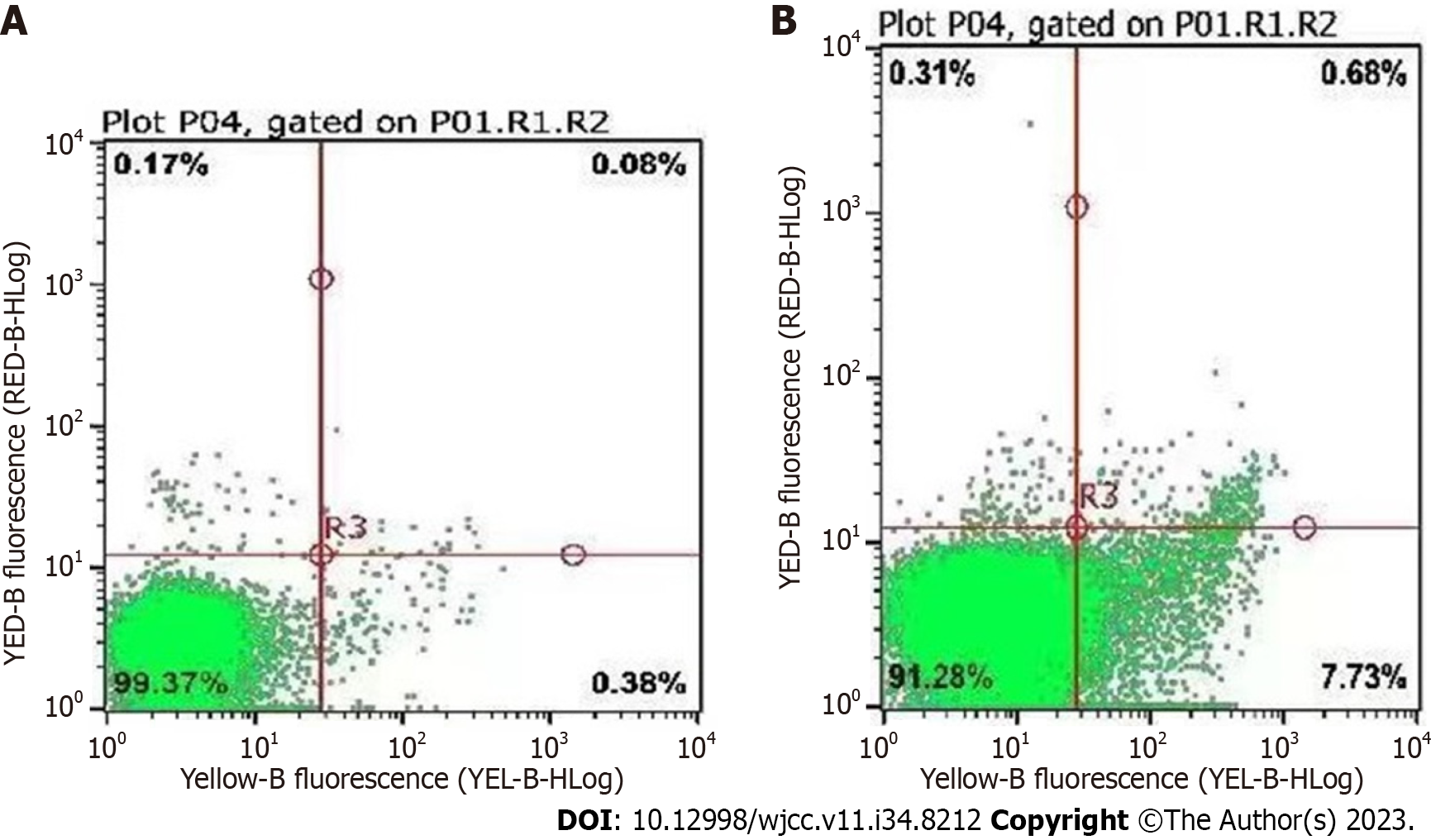
We consulted a hematologist again. Since the patient showed signs such as cytopenia affecting three lineages in the peripheral blood, hypertriglyceridemia, hypofibrinogenemia, ferritin > 500 ng/L, and hemophagocytosis in the bone marrow, HLH was considered. An examination of soluble interleukin-2 receptor alpha subunit and natural killer cell activity revealed that the soluble interleukin-2 receptor alpha subunit level was 22616 pg/mL (normal reference range < 6400 pg/mL) and natural killer cell activity was 8.14% (normal reference range ≥ 15.11%) (Figure 2), leading to a clear diagnosis of hemophagocytosis[1] (Table 2).
| Diagnostic criteria | |
| 1 | Molecular diagnosis consistent with HLH |
| 2 | Five of the following eight criteria are fulfilled |
| Fever | |
| Splenomegaly | |
| Cytopenias affecting at least two of the three lineages in the peripheral blood; hemoglobin < 90 g/L; platelets < 100 × 109; neutrophils < 1 × 109 | |
| Hypertriglyceridemia and/or hypofibrinogenemia | |
| Hemophagocytosis in bone marrow, spleen, or lymph nodes | |
| Low or absent natural killer cell activity | |
| Hyperferritinemia | |
| Soluble interleukin-2 receptor alpha subunit ≥ 2400 U/mL |
According to the consultation, HLH-1994 was suggested. For the patient, her general condition was extremely poor and complicated with severe gastrointestinal bleeding. She could not tolerate etoposide, so only corticosteroids were administered. Multiple organ support therapy was continued.
The patient continued to deteriorate and died on March 8, 2023.
HLH was first reported in 1939 by Scott and Robb-Smith as “medullary histiocytic reticulocytosis”[2], and since then, doctors have gradually learned more about the disease. HLH is characterized by fever, splenomegaly, and other atypical symptoms, and organ dysfunction occurs as the disease deteriorates. The pathogenesis of HLH involves systemic inflammation and severe cytokine storms caused by impaired natural killer cells and CD8+ cytotoxic cells[3,4]. HLH is classified as primary HLH and secondary HLH. Primary HLH is an autosomal or sex chromosomal recessive hereditary disease, while secondary HLH is triggered by infections, tumors, or autoimmune diseases[5]. Most studies on HLH involve pediatric patients, while few epidemiological data on adults have been published[6]. An international study in Japan that included children and adults showed that the incidence of HLH was 1/800000[7]. In adults, the proportion of secondary HLH can be as high as 90%. Malignancy, especially lymphoma and leukemia, is the main trigger factor[8]. The 30-d case fatality rate for HLH is approximately 27%[9], while it can reach 53%-57% in the intensive care unit, with sepsis as the main underlying factor[10,11].
HLH lacks typical symptoms in the clinic, resulting in a delay in diagnosis and treatment in most affected patients. Patients may present with persistent high fever, splenomegaly, lymph node enlargement, neurological symptoms, abnormal liver function, and coagulation dysfunction, which deteriorate rapidly to critical illness and shock[12,13]. Statistics on adult HLH show that it takes 1-93 d from the first symptom to diagnosis, and the average time to diagnosis is 10 d[14]. Among these patients, 93%-98% have fever, 84%-86% have splenomegaly, 36%-61% have hepatomegaly, 33%-50% have respiratory dysfunction, 31%-39% have neurological symptoms, and jaundice is present in only 11% of patients[8,14]. Therefore, few HLH patients present with jaundice as the first symptom, and it is crucial to recognize HLH with atypical symptoms and laboratory tests to avoid a delay in treatment.
The patient in this case report presented with jaundice as the first symptom. Since her elevated aminotransferase and bilirubin levels indicate that her liver did not function normally, we could not exclude the possibility that the jaundice was caused by biliary diseases; however, the jaundice and elevated aminotransferase persisted after the obstruction was resolved and progressively worsened. We consider HLH to be a more critical cause. Only two cases of HLH secondary to cholecystitis were retrieved. One of them did not record elevated bilirubin, and the other reported HLH with gallstones and elevated direct bilirubin, but details were not provided[12,15]. We consulted the literature and found that elevated aminotransferase could be found in the early phase of HLH and was associated with periportal vein lymphocyte infiltration, which means activation of the disease[16]. Elevated direct bilirubin was found in nearly 50% of HLH patients[17-19] and was found to be associated with prognosis[18,20,21]. Higher levels of direct bilirubin are associated with shorter patient survival[22]. A pathological study of liver damage in patients with primary HLH found[23] that lymphocyte-mediated bile duct damage was present in all specimens from HLH patients, and circumferential or clusters of monocytes or lymphocyte cells were interposed between the epithelium and its basal layer. Specimens from some patients showed cholestasis. The injury to the bile duct epithelium was mediated by infiltrating CD8+ and CD4+ T lymphocytes. The bile duct and portal inflammation observed in these specimens were similar to that in primary sclerosing cholangitis or primary cholestatic cirrhosis but without manifestations such as granuloma or bile duct sclerosis.
Treatment mainly follows three approaches[14]: (1) Immunosuppressants such as glucocorticoids, immunoglobulin, alemtuzumab, or etoposide are used to deplete immune cells and interrupt immune activation; (2) organ function support and the prevention of severe bleeding are initiated; and (3) treatment aims to mitigate trigger factors. The diagnosis of HLH was clear in our patient, and the trigger factor was sepsis. Blood culture and bile cultures obtained from the patient were consistent, with both indicating the presence of Klebsiella acidogenes and Enterococcus faecium (HLAR). Effective anti-infective treatment is crucial[24]. Bergsten’s studies have shown that etoposide is effective in improving patient outcomes and can be used as a first-line therapy[25]; however, recent studies have shown that the use of etoposide does not significantly improve survival[26]. In addition, etoposide could suppress immune function, which aggravates infection. For this reason, only glucocorticoids were used to treat the patient in the current study. The patient admitted to our hospital was of advanced age, was in extremely poor general health, had many comorbidities, and died.
HLH patients have low morbidity and a high mortality rate, and most of them have nonspecific symptoms. Many patients visit the emergency department first, so it is particularly important to improve the recognition of HLH. Few HLH patients have jaundice as the first symptom. In this patient, the jaundice was thought to be caused by biliary obstruction at first stage, causing elevated aminotransferase and bilirubin, but surgical treatment is ineffective. As the disease progressed, we found that the patient developed fever, splenomegaly, cytopenia, hypertriglyceridemia, hypofibrinogenemia, and elevated ferritin, and her HLH presented jaundice as the first symptom and was triggered by septic shock. We ultimately failed to save her. Clinicians should try hard to discover HLH as early as possible because early diagnosis can improve prognosis.
We would like to thank the patient and her family. We extend our thanks to the laboratory, radiology department, and EICU of the Beijing Tsinghua Changgung Hospital for facilitating the acquisition of the relevant materials.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tchilikidi KY, Russia S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3075] [Cited by in RCA: 3602] [Article Influence: 200.1] [Reference Citation Analysis (1)] |
| 2. | Griffin G, Shenoi S, Hughes GC. Hemophagocytic lymphohistiocytosis: An update on pathogenesis, diagnosis, and therapy. Best Pract Res Clin Rheumatol. 2020;34:101515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 202] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 3. | Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020;383:2255-2273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1324] [Cited by in RCA: 2104] [Article Influence: 420.8] [Reference Citation Analysis (0)] |
| 4. | Jordan MB, Allen CE, Greenberg J, Henry M, Hermiston ML, Kumar A, Hines M, Eckstein O, Ladisch S, Nichols KE, Rodriguez-Galindo C, Wistinghausen B, McClain KL. Challenges in the diagnosis of hemophagocytic lymphohistiocytosis: Recommendations from the North American Consortium for Histiocytosis (NACHO). Pediatr Blood Cancer. 2019;66:e27929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 265] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 5. | Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J, Requena-Caballero L, Jordan MB, Abdel-Wahab O, Allen CE, Charlotte F, Diamond EL, Egeler RM, Fischer A, Herrera JG, Henter JI, Janku F, Merad M, Picarsic J, Rodriguez-Galindo C, Rollins BJ, Tazi A, Vassallo R, Weiss LM; Histiocyte Society. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-2681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 974] [Article Influence: 108.2] [Reference Citation Analysis (0)] |
| 6. | Hayden A, Park S, Giustini D, Lee AY, Chen LY. Hemophagocytic syndromes (HPSs) including hemophagocytic lymphohistiocytosis (HLH) in adults: A systematic scoping review. Blood Rev. 2016;30:411-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 227] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 7. | Parikh SA, Kapoor P, Letendre L, Kumar S, Wolanskyj AP. Prognostic factors and outcomes of adults with hemophagocytic lymphohistiocytosis. Mayo Clin Proc. 2014;89:484-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 227] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 8. | Wang D, Tong X, Liu S, Zhang W, Wang L, Zhang S, Zhang T, Wang Q, Fan H. Clinical characteristics and risk factors for 90-day overall survival among 204 adult patients with secondary hemophagocytic lymphohistiocytosis: Experience from a single-center retrospective study. Front Med (Lausanne). 2022;9:774959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Apodaca E, Rodríguez-Rodríguez S, Tuna-Aguilar EJ, Demichelis-Gómez R. Prognostic Factors and Outcomes in Adults With Secondary Hemophagocytic Lymphohistiocytosis: A Single-center Experience. Clin Lymphoma Myeloma Leuk. 2018;18:e373-e380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Debaugnies F, Mahadeb B, Nagant C, Meuleman N, De Bels D, Wolff F, Gottignies P, Salaroli A, Borde P, Voué M, Corazza F. Biomarkers for Early Diagnosis of Hemophagocytic Lymphohistiocytosis in Critically Ill Patients. J Clin Immunol. 2021;41:658-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Bichon A, Bourenne J, Allardet-Servent J, Papazian L, Hraiech S, Guervilly C, Pauly V, Kaplanski G, Mokart D, Gainnier M, Carvelli J. High Mortality of HLH in ICU Regardless Etiology or Treatment. Front Med (Lausanne). 2021;8:735796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Al-Samkari H, Berliner N. Hemophagocytic Lymphohistiocytosis. Annu Rev Pathol. 2018;13:27-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 313] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 13. | Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383:1503-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 788] [Cited by in RCA: 962] [Article Influence: 87.5] [Reference Citation Analysis (0)] |
| 14. | Birndt S, Schenk T, Heinevetter B, Brunkhorst FM, Maschmeyer G, Rothmann F, Weber T, Müller M, Panse J, Penack O, Schroers R, Braess J, Frickhofen N, Ehl S, Janka G, Lehmberg K, Pletz MW, Hochhaus A, Ernst T, La Rosée P. Hemophagocytic lymphohistiocytosis in adults: collaborative analysis of 137 cases of a nationwide German registry. J Cancer Res Clin Oncol. 2020;146:1065-1077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 93] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 15. | Jin CQ, Dong HX, Zhou JW, Jia YX. Secondary hemophagocytic lymphohistiocytosis induced by cholecystitis: A case report and a review of the literature. Clin Chim Acta. 2016;460:236-239. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Ost A, Nilsson-Ardnor S, Henter JI. Autopsy findings in 27 children with haemophagocytic lymphohistiocytosis. Histopathology. 1998;32:310-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 87] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Li F, Yang Y, Jin F, Dehoedt C, Rao J, Zhou Y, Li P, Yang G, Wang M, Zhang R. Clinical characteristics and prognostic factors of adult hemophagocytic syndrome patients: a retrospective study of increasing awareness of a disease from a single-center in China. Orphanet J Rare Dis. 2015;10:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 18. | Bunchorntavakul C, Reddy KR. Hepatic Manifestations of Lymphoproliferative Disorders. Clin Liver Dis. 2019;23:293-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol. 2017;112:18-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 716] [Article Influence: 89.5] [Reference Citation Analysis (0)] |
| 20. | Yin G, Man C, Huang J, Liao S, Gao X, Tian T, Duan L, Xu J, Qiu H. The prognostic role of plasma fibrinogen in adult secondary hemophagocytic lymphohistiocytosis. Orphanet J Rare Dis. 2020;15:332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Zhou J, Wu ZQ, Qiao T, Xu HG. Development of Laboratory Parameters-Based Formulas in Predicting Short Outcomes for Adult Hemophagocytic Lymphohistiocytosis Patients with Different Underlying Diseases. J Clin Immunol. 2022;42:1000-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Cattaneo C, Oberti M, Skert C, Passi A, Farina M, Re A, Tozzi P, Borlenghi E, Rossi G. Adult onset hemophagocytic lymphohistiocytosis prognosis is affected by underlying disease and coexisting viral infection: analysis of a single institution series of 35 patients. Hematol Oncol. 2017;35:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Chen JH, Fleming MD, Pinkus GS, Pinkus JL, Nichols KE, Mo JQ, Perez-Atayde AR. Pathology of the liver in familial hemophagocytic lymphohistiocytosis. Am J Surg Pathol. 2010;34:852-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Chandrakasan S, Filipovich AH. Hemophagocytic lymphohistiocytosis: advances in pathophysiology, diagnosis, and treatment. J Pediatr. 2013;163:1253-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 173] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 25. | Bergsten E, Horne A, Aricó M, Astigarraga I, Egeler RM, Filipovich AH, Ishii E, Janka G, Ladisch S, Lehmberg K, McClain KL, Minkov M, Montgomery S, Nanduri V, Rosso D, Henter JI. Confirmed efficacy of etoposide and dexamethasone in HLH treatment: long-term results of the cooperative HLH-2004 study. Blood. 2017;130:2728-2738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 456] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 26. | Naymagon L, Tremblay D, Mascarenhas J. The Efficacy of Etoposide-Based Therapy in Adult Secondary Hemophagocytic Lymphohistiocytosis. Acta Haematol. 2021;144:560-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |