Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8205
Peer-review started: September 28, 2023
First decision: November 13, 2023
Revised: November 14, 2023
Accepted: November 24, 2023
Article in press: November 24, 2023
Published online: December 6, 2023
Processing time: 69 Days and 4.1 Hours
A Sister Mary Joseph nodule (SMJN) is an uncommon cutaneous metastasis found in the umbilicus, indicating an advanced malignancy. SMJNs typically originate from intra-abdominal sources, rarely from breast cancer. Diagnosis suggests a poor prognosis with a median survival of approximately 8 mo after detection. Managing patients with SMJNs is challenging, as most receive limited palliative care only. The optimal strategy for long-term survival of these patients remains unclear.
A 58-year-old female, previously diagnosed with right breast cancer 17 years ago and underwent breast-conserving surgery, adjuvant radiotherapy, and endocrine therapy, presented with a 2-cm umbilical nodule. Thirteen years previously, metastases were detected in the right supraclavicular, infraclavicular, hilar, and mediastinal lymph nodes. An umbilical nodule emerged four years before the date of presentation, confirmed as a skin metastasis of primary breast cancer upon excisional biopsy. Despite initial removal, the nodule recurred and grew, leading to her referral to our hospital. The patient underwent extensive excision of the umbilical tumor and immediate abdominal wall reconstruction. Endocrine therapy was continued postoperatively. Five years later, no local recurrence was observed, and the patient continued to work full-time, achieving over 9 years of survival following SMJN diagnosis.
This case study aimed to identify the optimal strategy for achieving extended survival outcomes in patients with SMJN through comprehensive treatment. We presented a case of the longest survival in a patient after undergoing a multidis
Core Tip: Sister Mary Joseph nodules (SMJN) typically present as firm, irregular periumbilical nodules, which are uncommon yet significant symptoms that indicate an advanced stage of malignancy with a poor prognosis. Although most patients receive limited treatment, the optimal systemic treatment strategy for long-term survival remains controversial. While treatment decisions should be based on the patient's overall health and condition, a multimodal treatment approach comprising timely and wide excision along with adjunctive therapy has the potential to control the disease, prolong survival, and improve the quality of life of patients with SMJNs without peritoneal dissemination.
- Citation: Kanayama K, Tanioka M, Hattori Y, Iida T, Okazaki M. Long-term survival of the Sister Mary Joseph nodule originating from breast cancer: A case report. World J Clin Cases 2023; 11(34): 8205-8211
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8205.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8205
The Sister Mary Joseph nodule (SMJN) is an unusual cutaneous metastasis in the umbilicus. It originates from intra-abdominal or pelvic sources and is rarely associated with breast cancer[1]. On physical examination, SMJN is an uncommon yet significant sign indicating an advanced stage of malignancy and a poor prognosis. The median survival duration after SMJN diagnosis was 7.9 mo, with a 95% confidence interval of 6.7 to 9.1 mo[2]. Because managing patients with SMJN is challenging, they generally receive limited treatments, such as palliative surgery or best supportive care. However, the optimal systemic treatment strategy for long-term survival remains controversial. This report presents a rare case of a patient diagnosed with SMJN originating from breast cancer who survived for over 9 years after receiving treatment with a multidisciplinary approach. The patient remained active in society, working full-time.
A painless 2-cm hard nodule with erosions in the umbilical region, which was first detected four years ago.
At age 41 (17 years ago), she underwent a right breast-conserving surgery (invasive ductal carcinoma, ER+, PR+, HER−, T2N2M0). The patient was treated with adjuvant chemotherapy (four cycles of Epirubicin and Cyclophosphamide), followed by adjuvant radiotherapy (50Gy/25Fr) and endocrine therapy (Tamoxifen). At age 45 (13 years ago), metastases were detected in her right supraclavicular to infraclavicular lymph nodes, right hilar lymph nodes, and mediastinal lymph nodes on positron emission tomography–computed tomography (PET-CT). Consequently, she was prescribed an LH-RH agonist (Leuprorelin) with Tamoxifen as a second-line treatment. Over time, the tumor showed a trend of reduction in both lymph node and lung metastases compared to their state before treatment, leading to the discontinuation of Leuprorelin. At age 53 (5 years ago), Tamoxifen was switched to Anastrozole as progressive enlargement of the right supraclavicular lymph node was found. One year later, Leuprorelin was resumed because the CT scan showed an increasing number of nodules in both the upper and lower lobes of the right lung. At age 54 (4 years ago), an umbilical nodule emerged, for which an excisional biopsy was performed, confirming skin metastasis originating from the primary breast cancer (adenocarcinoma, metastatic, ER+, PR+, HER−). Although endocrine therapy with Leuprorelin and Exemestane was initiated, the nodule recurred and gradually increased in size, leading to her referral to our hospital.
The patient has no significant medical history.
No notable abnormalities: Never smoked, no alcohol consumption, and no known allergies to drugs or food.
A hard, localized, and poorly mobile nodule accompanied by erosion was detected in the umbilical region. The nodule measured approximately 2 cm in diameter, with no redness, heat, pain, or tenderness (Figure 1A and B). A lymph node approximately 2 cm in diameter was palpable subcutaneously above the right clavicle, with no other palpable lymph nodes including the axillary or inguinal regions.
Her laboratory results were normal, with the carcinoembryonic antigen level at 3.1 ng/mL (normal reference value: 5 ng/mL), except for a slight elevation in the carbohydrate antigen (CA) 15-3 Level to 59 U/mL (normal reference value: 21 U/mL).
PET scans revealed increased 18F-fluorodeoxyglucose uptake in the umbilicus (SUVmax, 4.0), right supraclavicular fossa (SUVmax, 7.2), and bilateral lung fields (SUVmax, 1.2) (Figure 1C). Additionally, the PET-CT scan indicated no evident nodules suggesting tumor metastasis to the peritoneum in the abdominal cavity, nor was there any evidence of abdominal or pelvic fluid (Figure 1D).
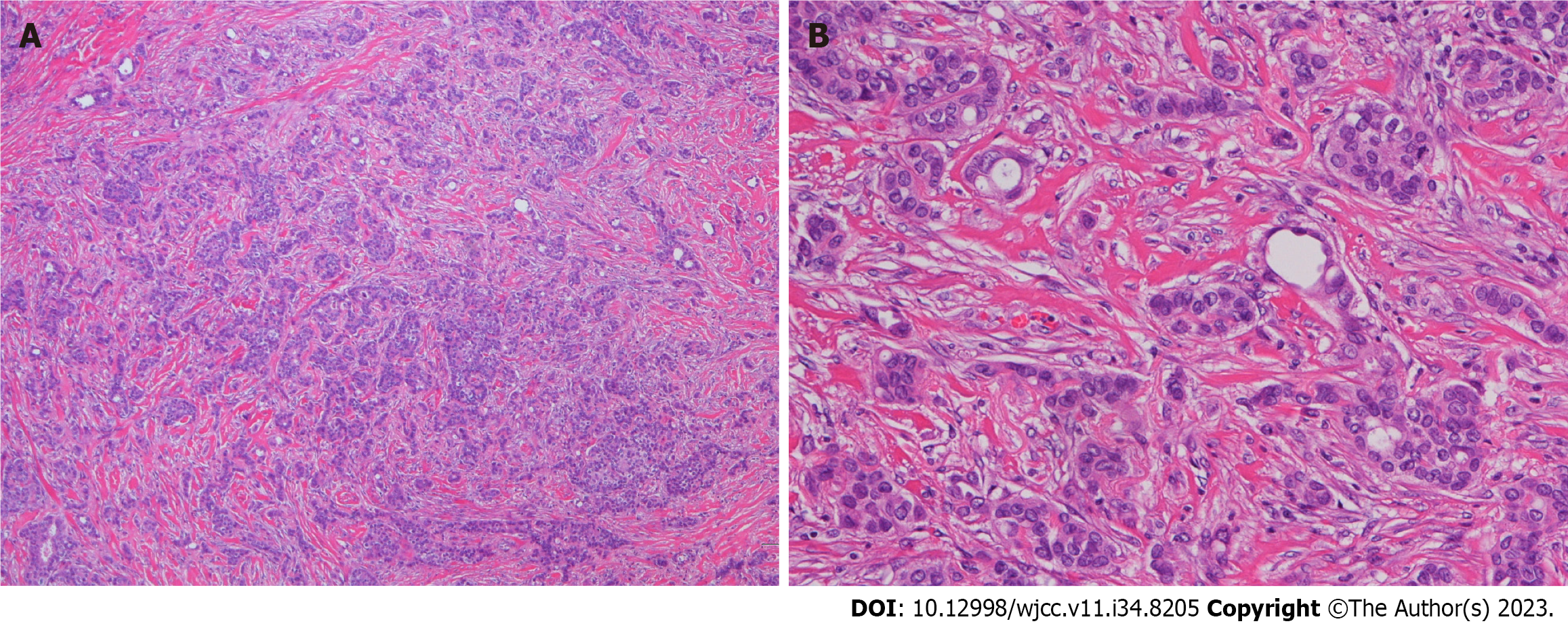
A puncture biopsy was performed, resulting in a diagnosis of recurrent metastatic adenocarcinoma originating from breast cancer. Histological examination confirmed adenocarcinoma with a foamy tubular arrangement (Figure 2). Immunohistochemistry was positive for ER and GCDFP-15, negative for PR and HER, and showed a low proliferative index of 7% for neoplastic cells on Ki67.
The tumor was excised with a 15 mm horizontal margin, involving combined resection of the peritoneum and falciform ligament (Figure 3A). No tumor was exposed to the abdominal cavity (Figure 3B and C), and no adhesions were observed in the intra-abdominal organs. There was no evidence of peritoneal dissemination. Given the large size of the defect, simple closure was challenging; therefore, we reconstructed the abdominal wall using a component separation technique (Figure 3D-F). Postoperative endocrine therapy with Toremifene citrate was initiated followed by adjuvant radiation therapy (45Gy/15Fr) for the enlarged right subclavian lymph nodes.
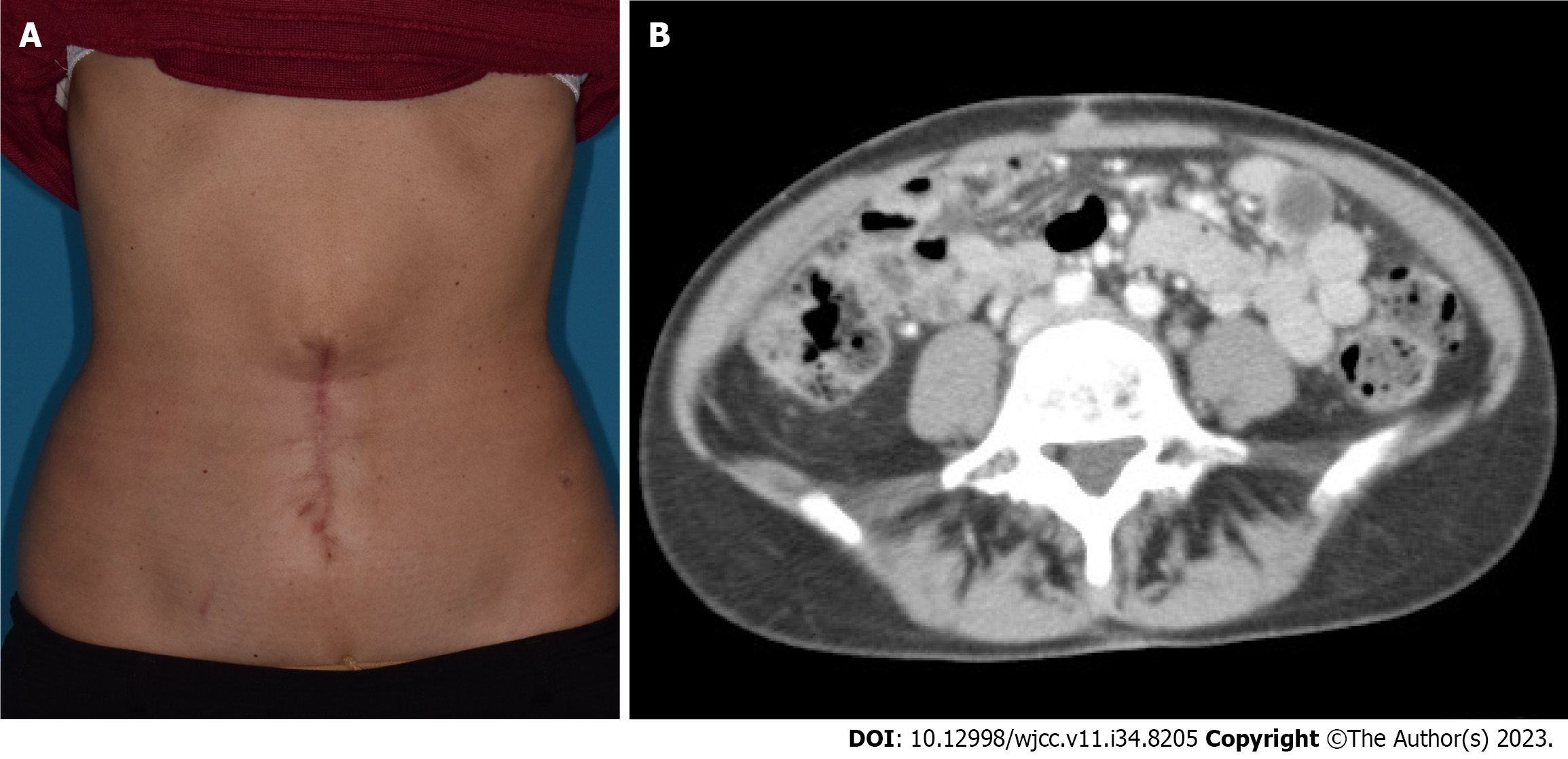
The wound healed completely, enabling the patient to return to work. Five years postoperatively, there was no evident local recurrence in the umbilical region, and the patient continued to work full-time, five days a week (Figure 4).
This report presents a case of long-term survival in a patient with an SMJN originating from breast cancer. SMJNs typically present as firm, irregular periumbilical nodules, usually measuring 0.5–2 cm. They may be painful, ulcerated, bloody, or suppurative[3]. For patients presenting with an umbilical nodule, the differential diagnosis should include primary umbilical neoplasms, metastatic umbilical nodules, umbilical hernias, umbilical endometriosis, keloids, pyoderma gangrenosum, and foreign bodies. Notably, SMJN may be the sole presenting complaint in some otherwise healthy patients. However, other patients may present with a poor clinical state and additional physical signs, such as ascites and pleural effusion[4]. A focused history and examination of the chest, abdomen, and regional lymph nodes can help identify the source of the primary neoplasm. Patients presenting with SMJN after treatment for a known neoplasm should be evaluated for recurrence. Biopsy of the umbilical nodule offers a convenient method for obtaining tissue samples for histological diagnosis. CT scan and magnetic resonance imaging can determine the extent of the malignancy.
Cutaneous metastases occur in up to 9% of malignancies, with only 10% localized to the umbilicus[5,6]. SMJN is typically associated with primary neoplasms of the gastrointestinal and genitourinary tracts. Other reported primary sites include the lungs, pancreas, liver, gallbladder, breast, kidney, prostate, and testicle[7,8]. However, the source of the primary neoplasm may remain unidentified in up to 30% of patients[5]. Only 1.7% of umbilical metastases originate from breast tissues[9].
The etiology of SMJN remains unclear. Proposed hypotheses include direct extension of the tumor to the umbilicus as well as lymphatic or hematogenous spread[10]. A literature review showed that 21 out of 23 (91%) patients with SMJN at presentation experienced peritoneal dissemination[11]. Although the mechanism of tumor spread from the breast to the umbilicus remains unclear, extensive vascular and lymphatic connections between the umbilicus and axillary and thoracic regions may facilitate the migration of breast tumor cells[5,6,12,13].
Patients diagnosed with SMJN typically have a poor prognosis: fewer than 30% of treated patients survive beyond 1 year, and fewer than 15% survive beyond 2 years[12]. To our knowledge, no report has described a patient with SMJN who survived for over 9 years. The recommended treatment approaches for SMJN remain controversial. Some physicians advocate an aggressive regimen combining surgery with adjunctive therapy[12,14], while others recommend avoiding surgery due to the poor prognosis[15]. Majmudar et al[12] demonstrated that an aggressive multimodality treatment approach, including both surgery and chemotherapy, improved survival (average survival 17.6 mo) compared to those treated with either surgery alone (average survival 7.4 mo) or adjunctive therapy alone (average survival 10.3 mo); patients who received no therapy had the lowest average survival of 2.3 mo. The prognosis of patients with SMJN is variable and may be most directly affected by the primary tumor type and location. Patients with a primary tumor originating from the pancreas had the poorest prognosis, with a median overall survival rate of approximately 3 mo from the date of diagnosis of umbilical metastasis, while those with primary tumors originating from the ovaries or endometrium had a median survival rate of approximately 10 mo[2].
When determining a management strategy, it is crucial to consider the patient's preferences, clinical condition, and the etiology of the primary malignancy. Although palliative care may be the only viable option for certain patients, others, when carefully selected, may benefit from more aggressive interventions such as surgery, chemotherapy, and radiotherapy. In the present case, the initial approach was local resection followed by endocrine therapy. However, due to disease progression, more extensive surgery was required. Timely and wide excision can prevent peritoneal dissemination and treat patients with SMJN. Peritoneal dissemination often distresses patients, manifesting as abdominal distension, constipation, pain, nausea, and vomiting. As the disease progresses, the patient's quality of life (QOL) can be impaired as a result of poor oral intake due to bowel obstruction, jaundice resulting from bile duct stenosis, and hydronephrosis caused by ureteral constriction. While such treatment decisions must align with the patient's overall health and condition, this strategy has the potential to control the disease, extend survival, and enhance the QOL in patients with SMJN.
The current study has limitations; as this is a report on just one patient's outcome, the results may not be generalizable to the broader population of patients with SMJNs originating from breast cancer. Additional studies with larger sample sizes are needed. Future studies could investigate potential biomarkers or clinical factors that could help identify SMJN patients who are more likely to respond positively to aggressive treatment approaches, similar to the case presented. This could lead to more personalized treatment plans.
This case study aimed to identify the optimal strategy for achieving extended survival outcomes in patients with SMJN through comprehensive treatment. We presented a case of the longest survival in a patient after undergoing a multidisciplinary treatment regimen. Our findings underscore the significance of adopting a multimodal treatment approach comprising timely and wide excision along with adjunctive therapy. This approach can control the disease, prolong survival, and improve the QOL in patients with SMJN.
We thank Drs. Aya Ushiku and Masako Ikemura, Department of Pathology, University of Tokyo Hospital, for their assistance in establishing the patient's pathological diagnoses.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He YF, China S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Brunelli M, Manfrin E, Miller K, Eccher A, Gobbo S, Reghellin D, Chilosi M, Remo A, Martignoni G, Menestrina F, Bonetti F. Her-2/neu evaluation in Sister Mary Joseph's nodule from breast carcinoma: a case report and review of the literature. J Cutan Pathol. 2009;36:702-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Hugen N, Kanne H, Simmer F, van de Water C, Voorham QJ, Ho VK, Lemmens VE, Simons M, Nagtegaal ID. Umbilical metastases: Real-world data shows abysmal outcome. Int J Cancer. 2021;149:1266-1273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Powell FC, Cooper AJ, Massa MC, Goellner JR, Su WP. Sister Mary Joseph's nodule: a clinical and histologic study. J Am Acad Dermatol. 1984;10:610-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 135] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Dar IH, Kamili MA, Dar SH, Kuchaai FA. Sister Mary Joseph nodule-A case report with review of literature. J Res Med Sci. 2009;14:385-387. [PubMed] |
| 5. | Gabriele R, Conte M, Egidi F, Borghese M. Umbilical metastases: current viewpoint. World J Surg Oncol. 2005;3:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Balakrishnan R, Rahman MA, Das A, Naznin B, Chowdhury Q. Sister Mary Jospeh's nodule as initial presentation of carcinoma caecum-case report and literature review. J Gastrointest Oncol. 2015;6:E102-E105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Abe H, Yamazaki K, Mori T, Kawai Y, Kubota Y, Umeda T, Ishida M, Tani T. Umbilical metastasis derived from breast cancer: report of a case. Surg Today. 2015;45:907-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Seymour NC, Rathinaezhil R. A rare case of umbilical metastasis after delayed transverse rectus abdominis myocutaneous flap reconstruction for invasive breast cancer. Breast Dis. 2017;37:33-35. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Galvañ VG. Sister Mary Joseph's nodule. Ann Intern Med. 1998;128:410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Salemis NS. Umbilical metastasis or Sister Mary Joseph's nodule as a very early sign of an occult cecal adenocarcinoma. J Gastrointest Cancer. 2007;38:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Otsuka I. Cutaneous Metastases in Ovarian Cancer. Cancers (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Majmudar B, Wiskind AK, Croft BN, Dudley AG. The Sister (Mary) Joseph nodule: its significance in gynecology. Gynecol Oncol. 1991;40:152-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 59] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Murata Y, Ogawa Y, Yamawaki Y, Kohsaki S, Kubota K, Nishioka A, Yoshida S, Tochika N. Umbilical metastasis from breast cancer related with tumor marker elevation. Radiat Med. 2006;24:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Chalya PL, Mabula JB, Rambau PF, McHembe MD. Sister Mary Joseph's nodule at a University teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013;11:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Requena Caballero L, Vázquez López F, Requena Caballero C, Urrutia Hernando S, Sánchez López M, Sánchez Yus E, Hernández Moro B. Metastatic umbilical cancer--Sister Mary Joseph's nodule: report of two cases. J Dermatol Surg Oncol. 1988;14:664-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |