Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8200
Peer-review started: September 24, 2023
First decision: October 24, 2023
Revised: October 31, 2023
Accepted: November 28, 2023
Article in press: November 28, 2023
Published online: December 6, 2023
Processing time: 72 Days and 18.6 Hours
Central venous catheter insertion is an invasive procedure that can cause complications such as infection, embolization due to air or blood clots, pneumothorax, hemothorax, and, rarely, chylothorax due to damage to the thoracic duct. Herein, we report a case of suspected thoracic duct cannulation that occurred during left central venous catheter insertion. Fortunately, the patient was discharged without any adverse events related to thoracic duct cannulation.
A 46-year-old female patient presented at our department to undergo cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. During anesthesia, we decided to insert a central venous catheter through the left internal jugular vein because the patient already had a chemoport through the right central vein. During the procedure, blood reflux was observed when the needle tip was not within the ultrasound field of view. We did not try to find the tip; however, a guide wire and a central venous catheter were inserted without any resistance. Subsequently, when inducing blood reflux from the distal port of the central venous catheter, only clear fluid, suspected to be lymphatic fluid, was regurgitated. Further, chest X-ray revealed an appearance similar to that of the path of the thoracic duct. Given that intravenous fluid administration was not started and no abnormal fluid collection was noted on preoperative chest X-ray, we suspected thoracic duct cannulation.
It is important to use ultrasound to confirm the exact position of the needle tip and guide wire path.
Core Tip: Central venous catheter insertion is an invasive procedure that requires detailed knowledge of the anatomy and attention of the proceduralist. It is recommended to use the right internal jugular vein for this procedure to avoid damaging the thoracic duct. However, regardless of right or left insertion, it is important to use ultrasound to confirm the exact position of the needle tip and guide wire path.
- Citation: Hwang GH, Eom W. Thoracic duct cannulation during left internal jugular vein cannulation: A case report. World J Clin Cases 2023; 11(34): 8200-8204
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8200.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8200
Central venous catheter insertion is performed to secure the route of administration of intravenous fluids and transfusions as well as to administer medications and measure central venous pressure[1]. The internal jugular, subclavian, and femoral veins are most commonly used for this procedure. Notably, central venous catheter insertion is an invasive procedure that can lead to various complications, including infections, embolism due to air or blood clots, arrhythmia, hematoma, arterial puncture, pneumothorax, hemothorax, and cardiac tamponade[2]. Thoracic duct injury can rarely occur as a complication of left internal jugular or subclavian vein cannulation; thus, cannulation of right-sided veins is preferred[3].
Notably, complications caused by central venous catheter insertion are decreasing because of the use of ultrasound[4]. Herein, we report a case of suspected thoracic duct cannulation despite central venous catheter insertion performed through the left internal jugular vein using ultrasound.
A 46-year-old female patient presented at our department to undergo cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) with chief complaints of intra-abdominal recurrence and metastasis of a sigmoid colon tumor.
In the preoperative assessment, the patient’s vital signs were stable and complete blood test results were within the normal range. Further, chest X-ray findings were unremarkable, except for the presence of a chemoport through the right central vein. Meanwhile, electrocardiogram revealed a normal sinus rhythm of 60 beats per minute.
The patient reported that she had undergone laparoscopic anterior resection of the colon 3 years ago. She also reported having the same medical conditions and undergoing CRS and HIPEC 2 years ago.
The patient had no family or genetic history of the disease.
Given that the patient had a chemoport through the right central vein, during anesthesia in the operating room, we decided to insert a central venous catheter through the left internal jugular vein. The location of the left internal jugular vein was confirmed using ultrasound, and the needle was inserted after confirming the course of the vein.
Although the internal jugular vein was distinctly visible on the ultrasound scan, blood reflux was noted when the needle tip was not within the ultrasound field of view. The guide wire was pushed through the needle, and we confirmed that it entered without resistance. Further, a 7-Fr 2-lumen central venous catheter was inserted along the guide wire without resistance. After inserting the catheter up to 15 cm, the guide wire was removed. Then, to remove the air, we regurgitated blood from the catheter and assessed blood reflux. However, after approximately 1 cc of blood was refluxed, we found that when blood reflux was induced, only clear fluid regurgitated from the 16-G distal port of the central venous catheter, but no blood regurgitated from the 18-G proximal port of central venous catheter. Because intravenous fluid administration was not started and no abnormal fluid collection was noted on preoperative chest X-ray, thoracic duct cannulation was suspected. Thus, we determined that central venous catheter could not be used as a central line. Accordingly, we reinserted the central venous catheter through the left subclavian vein under ultrasound guidance. Further, while carefully monitoring the needle tip and guide wire, we easily inserted the central venous catheter (Figure 1). The patient’s vital signs were stable. Meanwhile, the position of the tip of the internal jugular central venous catheter that was initially inserted was unclear. However, we determined that the catheter was unlikely to affect vital signs and that removing it without checking its position could cause problems. Therefore, we decided to leave it in the same position and checked its position after surgery.
Postoperative complete blood test results were within the normal range.
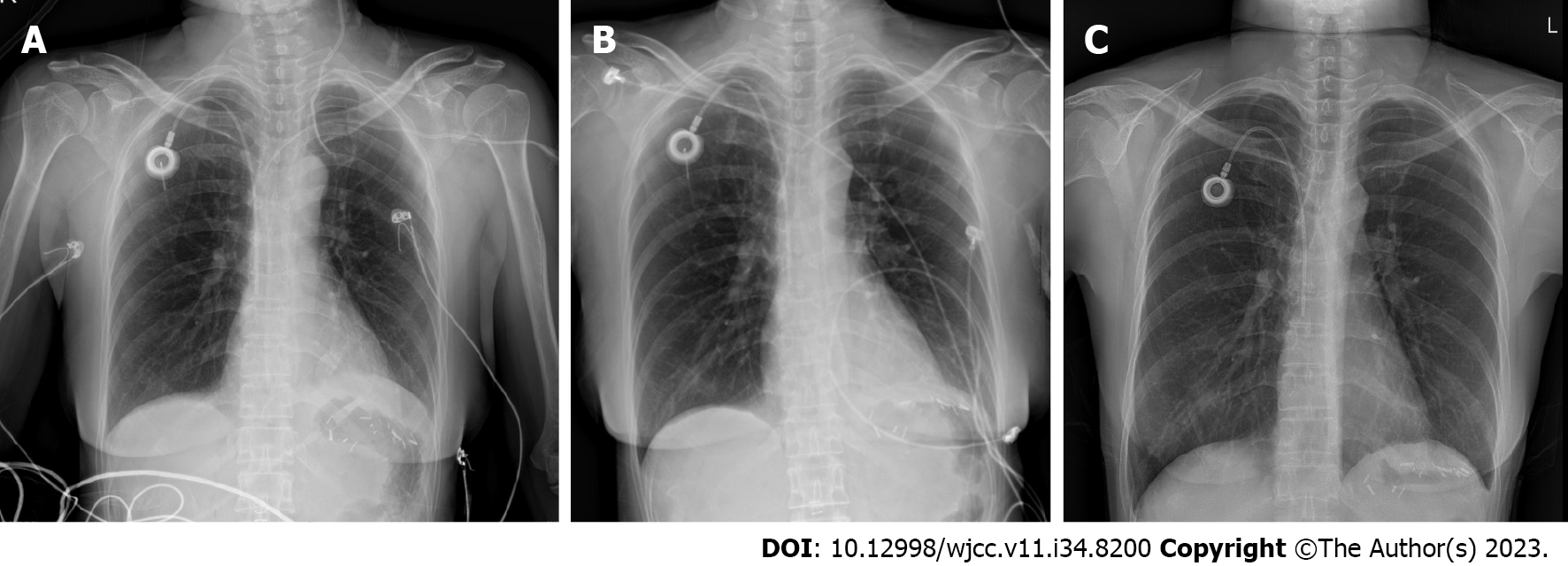
In the recovery room, a chest X-ray was obtained (Figure 2A), which revealed an appearance similar to that of the path of the thoracic duct.
The patient was diagnosed with thoracic duct cannulation. On preoperative chest X-ray, no abnormal fluid collection that could lead to clear fluid was noted. Further, during the procedure (i.e., during central venous catheter insertion through the left internal jugular vein), intravenous fluid administration was not started through the central venous catheter. From an anatomical perspective, the only structure that can produce clear fluid where the central venous catheter is located is the thoracic duct, which joins the left venous system. In addition to the abovementioned findings, given the clinical feature that only clear fluid suspected to be lymphatic fluid regurgitated when blood reflux was induced from the distal port of the central venous catheter and that the patient’s chest X-ray revealed an appearance similar to that of the path of the thoracic duct, we considered that the central venous catheter was inserted through the thoracic duct opening.
Although the patient’s vital signs were stable, she was transferred to the intensive care unit for observation owing to the possibility of pneumothorax and chylothorax. She exhibited no respiratory symptoms, such as shortness of breath, cough, or phlegm. Moreover, her condition remained unchanged and her vital signs were stable overnight. The next day, after consultation with the thoracic surgery department, the internal jugular central venous catheter was removed, and the patient was transferred to the general ward because her chest X-ray revealed no findings of chylothorax or pneumothorax. Furthermore, chest X-rays obtained on postoperative day 2 revealed no abnormalities (Figure 2B), and the patient was observed in the general ward.
The patient experienced no other significant complications postoperatively, and she was discharged on postoperative day 14. At that time, her chest X-ray revealed no abnormalities (Figure 2C).
In the present case, fortunately, there were no complications leading to the suspicion of chylothorax. However, caution should always be exercised in such cases because chylothorax may occur if the thoracic duct is damaged due to thoracic duct cannulation.
The anatomy of lymphatics varies widely. Normally, the thoracic duct is 38-45 cm long and 2-3 mm thick. It extends from the cisterna chyli at the L2 level to the neck and passes behind the aortic arch and the left subclavian artery. Further, thoracic duct forms an arch 3-5 cm above the clavicle, makes an acute angle near the left subclavian vein and the left internal jugular vein, and joins the venous system[5].
The flow rate of chyle is approximately 2.4 L/d. This rate is dependent on diet, activity level, and intestinal function and can increase with a triglyceride-rich diet. Conversely, the amount of chyle is significantly reduced if patients are immobilized, starved, or constantly suctioned with a nasogastric tube. This is why bowel rest is used as a treatment for chylothorax[6,7].
Chylothorax can be treated conservatively with bowel rest, somatostatin/octreotide medication to reduce chyle production, and drainage through a chest tube or catheter. However, patients who fail to respond to conservative treatment may require surgical intervention[6,7].
In the present case, a clear fluid regurgitated through the inserted catheter, and postoperative chest X-ray findings led to the suspicion of direct cannulation of the thoracic duct into the opening at the site where it joins the subclavian or internal jugular vein. For a more accurate diagnosis, the regurgitated fluid should be analyzed for triglyceride concentration to detect the presence of chyle; alternatively, computed tomography or lymphangiography may be needed.
Initially, the following cases were considered for cannulation of the thoracic duct: (1) Direct puncture from outside the thoracic duct; and (2) double puncture of the thoracic duct through the internal jugular vein. However, after removing the catheter, there were no remarkable findings, including chylothorax or pneumothorax, chylocele at the site of thoracic duct inlet, and hematoma. Thus, the catheter was thought to be directly cannulated through the thoracic duct opening, where the thoracic duct connects to the internal jugular or subclavian vein.
To avoid thoracic duct cannulation during central venous catheterization, it is important to use ultrasound to accurately identify the position of the needle tip and guide wire path during needle entry because the thoracic duct is located 3−5 cm above the clavicle. Moreover, the proceduralist should be alert and have a clear understanding of the anatomy.
Central venous catheter insertion is an invasive procedure requiring accurate knowledge of anatomy and proceduralist alertness. During this procedure, it is recommended to use the right internal jugular vein to avoid damage to the thoracic duct. Regardless of right or left insertion, it is important to use ultrasound to confirm the exact position of the needle tip and guide wire path.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shen ZY, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Practice Guidelines for Central Venous Access 2020: An Updated Report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2020;132:8-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 143] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 2. | Safety Committee of Japanese Society of Anesthesiologists. Practical guide for safe central venous catheterization and management 2017. J Anesth. 2020;34:167-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. Int J Crit Illn Inj Sci. 2015;5:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 182] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 4. | Katrancioglu N. Unusual mechanical complications of central venous catheterization. Saudi Med J. 2019;40:287-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Hematti H, Mehran RJ. Anatomy of the thoracic duct. Thorac Surg Clin. 2011;21:229-238, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Saxena P, Shankar S, Kumar V, Naithani N. Bilateral chylothorax as a complication of internal jugular vein cannulation. Lung India. 2015;32:370-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |