Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8184
Peer-review started: September 16, 2023
First decision: October 17, 2023
Revised: October 29, 2023
Accepted: November 24, 2023
Article in press: November 24, 2023
Published online: December 6, 2023
Processing time: 80 Days and 16.8 Hours
Cochineal red is an organic compound widely used in food, cosmetics, pharmaceuticals, textiles, and other fields due to its excellent safety profile. Poisoning caused by eating foods containing cochineal red is rare, and repeated atrial arrhythmia due to cochineal red poisoning is even rarer.
An 88-year-old Asian female patient was admitted to hospital due to a dis
Although cochineal red is a safe, natural food additive, excessive consumption or occupational exposure can induce cardiac arrhythmias.
Core Tip: Poisoning caused by eating foods containing cochineal red is rare, and repeated atrial arrhythmia caused by cochineal red poisoning is even rarer. For the first time, we report a case of repeated atrial arrhythmia caused by cochineal red poisoning. Through this case report, clinicians and the public will gain knowledge of the risks of excessive consumption of foods containing cochineal red pigment.
- Citation: Yang H, Wang YJ, Xu BP, Peng HW, Xu Q, Yu HB. Repeated atrial arrhythmia induced by cochineal red poisoning: A case report. World J Clin Cases 2023; 11(34): 8184-8191
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8184.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8184
Cochineal red is a natural pigment extracted from female cochineal insects. In its natural state, it is powdered and reddish or purplish red[1]. As an organic compound, cochineal red is widely used in food, cosmetics, pharmaceuticals, textiles, and other fields because of its excellent safety profile[2]. In China, cochineal red is commonly used to dye eggs for good wishes during the Dragon Boat Festival. Poisoning due to eating foods containing cochineal red is rare, and repeated atrial arrhythmia caused by cochineal red poisoning is even rarer.
Here, we report a case of cochineal red poisoning that presented as tender pink skin, purple–red urine, and repeated atrial arrhythmia in an 88-year-old patient, which improved rapidly after active treatment. Through this case report clinicians and the public can become aware of the risks of excessive consumption of food containing cochineal red pigment.
An 88-year-old Asian female patient was admitted to the hospital due to a disturbance of consciousness. Twelve hours prior to presentation, the patient ate 12 eggs containing cochineal red over a period of 2 h.
The patient had a disturbance of consciousness after eating 12 red eggs containing cochineal red before her family rushed her to hospital. Considering the potential risk of respiratory failure, the emergency department physician immediately intubated the trachea, and the patient was admitted to the intensive care unit.
The patient was diagnosed with hypertension 10 years prior to presentation. She managed her blood pressure with oral nifedipine tablets (10 mg, tid). She also experienced a cerebral infarction 2 years prior to presentation. The muscle strength in her left limb was grade 3, she was able to independently walk and get out of bed, and her speech was clear.
The patient had no significant personal or family history.
Upon physical examination, the patient’s temperature was 36.9 ℃, heart rate 131 beats/min, respiratory rate 20 breaths/min, blood pressure 149/74 mmHg, and peripheral capillary oxygen saturation (breathing 30% oxygen) 96%. The patient was in a coma and had a score of 6 on the Glasgow Coma Scale (E2 + VT + M4). The patient’s skin and mucous membranes were pink (Figure 1). The superficial lymph nodes were not enlarged. The pupils were equal in size and circular with a diameter of approximately 3 mm, and the light reflex was slow. The patient’s exhaled air was not abnormal. The breath sounds of both lungs were coarse, and scattered wet rales were heard. The heartbeat rhythm was irregular without any other pathological signs.
Initial blood investigations revealed a total white blood cell count of 20.79 × 109/L (normal range: 4 × 109-10 × 109/L), neutrophil count 19.39 × 109/L (normal range: 2 × 109-7.5 × 109/L), hemoglobin 109 g/L (normal range: 110-160 g/L), platelet count 176.0 × 109/L (normal range: 100 × 109-300 × 109/L), C-reactive protein 7.20 mg/L (normal range: 0-5 mg/L), procalcitonin 0.14 ng/mL (normal range: 0-0.5 ng/mL), and glycated hemoglobin 6.5% (normal range: 3.9%-6.5%). Electrolyte, coagulation function, liver and kidney function, amylase, cholinesterase, myocardial enzymes, troponin, B-type natriuretic peptide, and blood lipids were all within the normal range. A routine urine test showed purple urine (Figure 1), while other values were normal. Arterial blood gas analysis showed a pH of 7.414 (normal range: 7.35-7.45), partial pressure of oxygen 167 mmHg (FiO2: 35%, normal range: 83-108 mmHg), and partial pressure of carbon dioxide 30.2 mmHg (normal range: 35-48 mmHg). The residual base level was -4.3 mmol/L (normal range: -2.0 to 2.0 mmol/L), HCO3 was 20.9 mmol/L (normal range: 22-28 mmol/L), and plasma lactate level 5.84 mmol/L (normal range: 0.5-1.6 mmol/L).
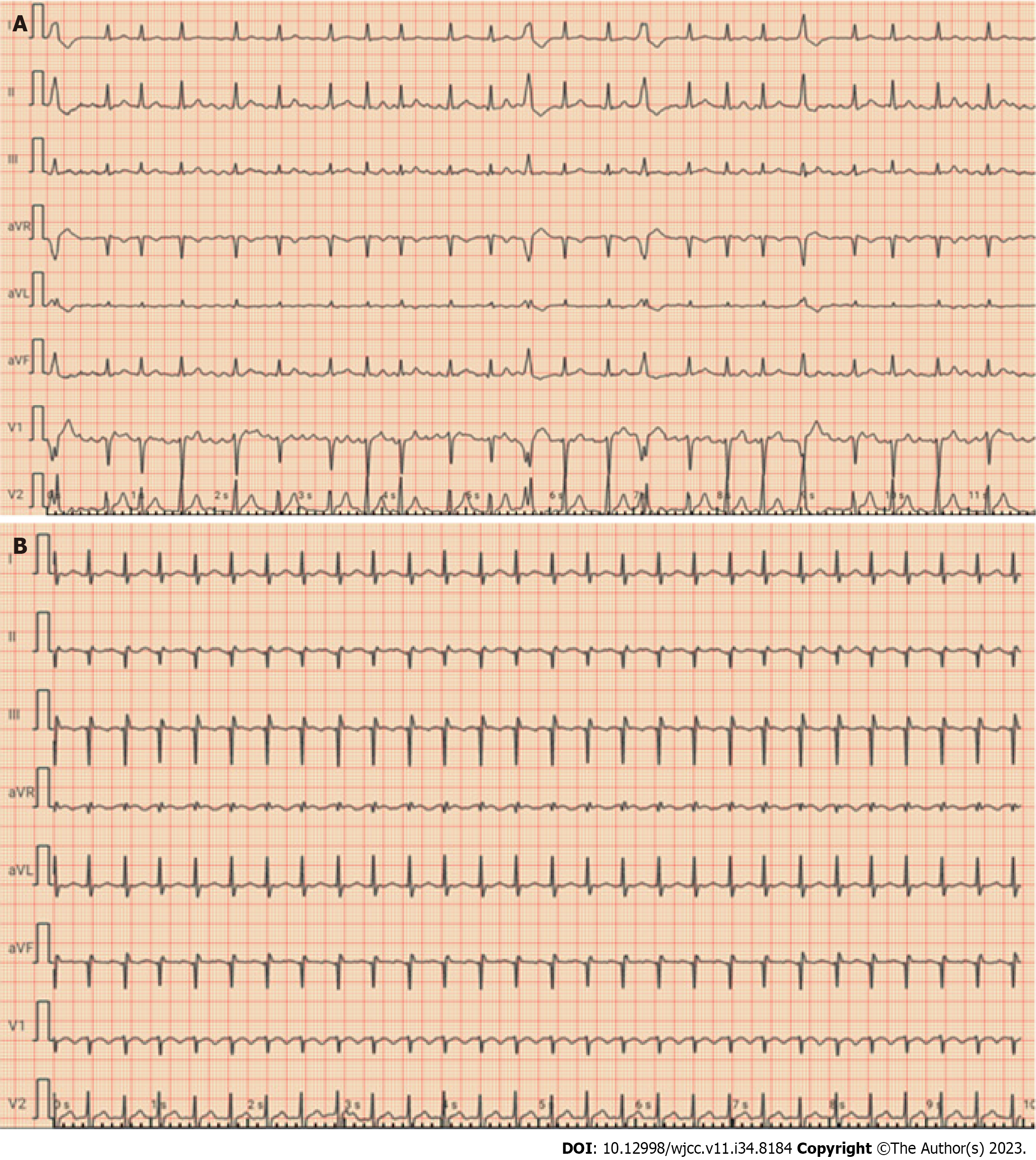
Echocardiography showed a left ventricular ejection fraction of 60% and no pericardial effusion. Electrocardiography (ECG) revealed rapid atrial fibrillation without any signs of ischemia (Figure 2A). Computed tomography of the brain, lung, and abdomen revealed no abnormalities.
The patient was diagnosed with acute cochineal red poisoning, hyperlactatemia combined with metabolic acidosis, and rapid atrial fibrillation.
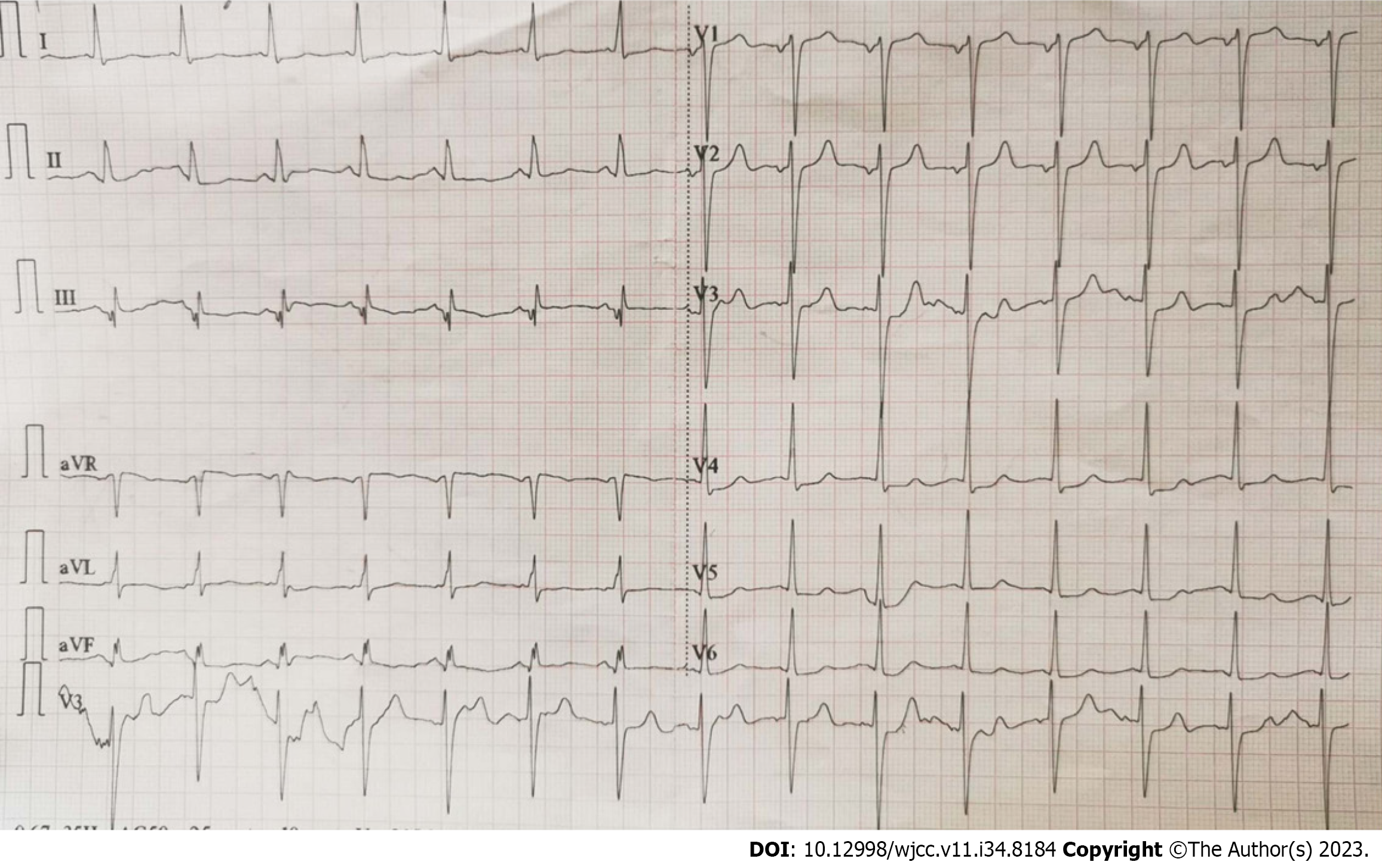
The patient received fluid replacement and began cedilan for arrhythmia correction. Shortly after admission, the atrial fibrillation converted to normal sinus rhythm. The arterial blood gas analysis and plasma lactate level returned to normal 8 h after admission. Approximately 18 h after admission, the patient regained consciousness. At 09:35 h, the patient had a sudden atrial flutter (Figure 2B), accompanied by hemodynamic instability (systolic blood pressure: 80-90 mmHg; diastolic blood pressure: 40-55 mmHg) and a rapidly declining arterial oxygen saturation between 85% and 90%. The sinus rhythm returned to normal after two electrical cardioversions, and intravenous microinfusion of amiodarone was administered. Electrolytes, myocardial enzymes, and troponin were re-examined and showed no abnormalities. The tracheal intubation was removed, but the skin color of the patient was still pink. We observed that the patient’s skin was slightly less pink on the day 3 after admission (Figure 3). Amiodarone was stopped on day 4 after admission because ECG showed a normal sinus rhythm (Figure 4).
Six days after admission, the pink tint in the patient’s skin significantly subsided (Figure 5), and the blood routine tests, coagulation function, liver and kidney function, electrolytes, and ECG were normal. The patient was transferred out of the intensive care unit because her symptoms were continuously improving. She was discharged after 12 d of hospitalization. At the 2-mo follow-up the patient was in good health with no recurrence of arrhythmia.
Cochineal red is a natural anthraquinone pigment extracted from female cochineal beetles growing on cacti[1]. It appears as a red crystal or reddish-brown powder in its natural state and is easily soluble in water. Carminic acid is the main active component of cochineal red, which contains eight hydroxyl groups and one carboxyl group in each molecule[3]. The physicochemical properties of cochineal red are stable, and it is stable in light and heat and when exposed to oxidants[1]. As an excellent colorant, cochineal red pigment is widely used in food additives due to its high safety profile and good affinity for meat proteins. In vitro and in vivo tests have also shown that it has no toxicity nor teratogenicity[4].
Cochineal red contains nonpigment components, such as insect proteins and lipids. These components can vary from batch to batch and may lead to rare allergic reactions and diseases[5]. Cochineal-red-related anaphylaxis[5], urticaria[6], occupational asthma[7], and allergic contact dermatitis[8] have been reported, and the main mechanism is IgE-mediated anaphylaxis[9]. Cochineal red may be a potentially overlooked allergen in patients with chronic allergic diseases and in children[10,11]. Cochineal red is also a cause of occupational respiratory allergies[7]. Therefore, people with allergic diseases are at an increased risk of adverse reactions when eating food containing the pigment or when exposed to cochineal-red-related products.
There are few clinical reports available on adverse reactions caused by cochineal red. However, repeated atrial arrhythmia caused by cochineal red has not been reported to date. Therefore, the clinical characteristics, treatment, and prognosis of atrial arrhythmia caused by acute cochineal red poisoning remain limited. In our patient, coagulation function, liver and kidney functions, electrolytes, amylase, cholinesterase, myocardial enzyme profile, troponin, B-type natriuretic peptide, and blood lipids were all within the normal range at admission. Emergency arterial blood gas analysis suggested hyperlactatemia with acidosis, while the ECG revealed rapid atrial fibrillation. The lactate level and acidosis quickly returned to normal, and the ECG revealed a normal sinus rhythm after initial intravenous fluid rehydration, antiarrhythmic application, and symptomatic treatment.
However, the skin of the patient remained pink, suggesting that cochineal red was not completely cleared from the body. Hyperlactacidemia and acidosis were considered possible causes of hypoxia during transportation to the hospital. On day 2 of hospitalization, the patient had a sudden atrial flutter but returned to a sinus rhythm after electric cardioversion. Re-examination of blood tests, liver and kidney functional electrolytes, myocardial enzymes, and troponin were normal, and intravenous fluids and symptomatic treatment were administered. On day 3 after admission, the pink color of the patient’s skin decreased. By day 6 of admission, the patient’s skin color returned to normal.
The patient had no previous history of arrhythmia. Initial ECG showed atrial fibrillation after admission, which was quickly resolved. The atrial flutter that occurred on the next day was also resolved quickly. According to the clinical manifestations, the patient was diagnosed with repeated atrial arrhythmia caused by cochineal red poisoning. After symptomatic treatment, the condition of the patient improved, and she recovered well with no recurrence of arrhythmia at the 2-mo follow-up.
To the best of our knowledge, this is the first reported case of repeated atrial arrhythmia associated with cochineal red poisoning. Therefore, for patients with cochineal red poisoning, routine fluid replenishment, diuresis, and maintenance of a stable internal environment can be performed. Blood purification therapy or hemoperfusion may also be performed to accelerate the internal excretion of cochineal red. However, evidence to show the effectiveness of this intervention is lacking.
The specific mechanism of repeated atrial arrhythmia caused by cochineal red remains unclear based on the limited literature. Some studies have suggested that cochineal red typically contains contaminating proteins, including a 38-kDa protein thought to be the primary allergen[2]. These proteins can induce an IgE-mediated food allergy and/or allergic diseases in patients using these products[12]. The toxicity of cochineal red in rats suggested that acute oral toxicity is low. The only adverse effect noted by the study was an unusual color[13]. Therefore, we hypothesize that repeated atrial arrhythmia may be caused by cochineal red allergy. However, more research on the safety and toxicity of cochineal red is needed to clarify the mechanism in the future.
There were some limitations to this study. Quantitative analysis of relevant toxicants can provide further information regarding the severity and prognosis of the disease. However, due to the limitations of objective conditions in our hospital, we were unable to obtain the concentration or specific metabolic components of cochineal red in the patient’s gastrointestinal tract, blood, or urine. The lack of cochineal red toxicological test results led to certain defects in the diagnosis of this patient.
Cochineal red is a safe, natural food additive. In China, it is widely used for red-dyed eggs. However, excessive consumption of food containing cochineal red or occupational exposure to the cochineal red pigment may induce allergic reactions, urticaria, allergic asthma, and cardiac arrhythmias. Therefore, clinicians and the public should know about the health risks of cochineal red.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gulel O, Turkey S-Editor: Qu XL L-Editor: Kerr C P-Editor: Zhao S
| 1. | Stathopoulou K, Valianou L, Skaltsounis AL, Karapanagiotis I, Magiatis P. Structure elucidation and chromatographic identification of anthraquinone components of cochineal (Dactylopius coccus) detected in historical objects. Anal Chim Acta. 2013;804:264-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Takeo N, Nakamura M, Nakayama S, Okamoto O, Sugimoto N, Sugiura S, Sato N, Harada S, Yamaguchi M, Mitsui N, Kubota Y, Suzuki K, Terada M, Nagai A, Sowa-Osako J, Hatano Y, Akiyama H, Yagami A, Fujiwara S, Matsunaga K. Cochineal dye-induced immediate allergy: Review of Japanese cases and proposed new diagnostic chart. Allergol Int. 2018;67:496-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Cox CE, Ebo DG. Carmine red (E-120)-induced occupational respiratory allergy in a screen-printing worker: a case report. B-ENT. 2012;8:229-232. [PubMed] |
| 4. | Grant D, Gaunt IF, Carpanini FM. Teratogenicity and embryotoxicity study of carmine of cochineal in the rat. Food Chem Toxicol. 1987;25:913-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Voltolini S, Pellegrini S, Contatore M, Bignardi D, Minale P. New risks from ancient food dyes: cochineal red allergy. Eur Ann Allergy Clin Immunol. 2014;46:232-233. [PubMed] |
| 6. | Kotobuki Y, Azukizawa H, Nishida Y, Murota H, Katayama I, Yoshikawa K. [Case of urticaria due to cochineal dye in red-colored diet]. Arerugi. 2007;56:1510-1514. [PubMed] |
| 7. | Lizaso MT, Moneo I, García BE, Acero S, Quirce S, Tabar AI. Identification of allergens involved in occupational asthma due to carmine dye. Ann Allergy Asthma Immunol. 2000;84:549-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Suzuki K, Hirokawa K, Yagami A, Matsunaga K. Allergic contact dermatitis from carmine in cosmetic blush. Dermatitis. 2011;22:348-349. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | De Pasquale T, Buonomo A, Illuminati I, D'Alò S, Pucci S. Recurrent Anaphylaxis: A Case of IgE-Mediated Allergy to Carmine Red (E120). J Investig Allergol Clin Immunol. 2015;25:440-441. [PubMed] |
| 10. | Sadowska B, Sztormowska M, Gawinowska M, Chełmińska M. Carmine allergy in urticaria patients. Postepy Dermatol Alergol. 2022;39:94-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Machler BC, Jacob SE. Carmine Red: A Potentially Overlooked Allergen in Children. Dermatitis. 2018;29:92-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Acero S, Tabar AI, Alvarez MJ, Garcia BE, Olaguibel JM, Moneo I. Occupational asthma and food allergy due to carmine. Allergy. 1998;53:897-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Cooksey CJ. The red insect dyes: carminic, kermesic and laccaic acids and their derivatives. Biotech Histochem. 2019;94:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |