Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8176
Peer-review started: August 29, 2023
First decision: October 9, 2023
Revised: October 25, 2023
Accepted: November 24, 2023
Article in press: November 24, 2023
Published online: December 6, 2023
Processing time: 98 Days and 19.8 Hours
Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease that can affect the gastrointestinal tract. Most cases of lupus enteritis (LE) involve the small intestine, while the involvement of the whole colon and rectum without the small intestine being affected is extremely rare.
A 35-year-old woman was diagnosed with colorectal LE after initially presenting with intermittent abdominal pain and vomiting for two months. She had a regular medication history for five years following the diagnosis of SLE but had been irregular in taking medications, which may have contributed to the onset of LE and led to her current hospital admission. According to the 2019 Classification criteria for SLE of the European League Against Rheumatism/American College of Rheumatology, this case scored 14. Additionally, abdominal computed tomo
Although colorectal LE without small intestine involvement is very rare, early diagnosis and excellent management with corticosteroids prevented the need for surgical intervention. Physicians should be aware of colorectal LE without small intestine involvement as a manifestation of lupus flare.
Core Tip: According to the 2019 Classification criteria for systemic lupus erythematosus of the European League Against Rheumatism/American College of Rheumatology classification criteria, the score of this case was 14. In addition, computed tomography of abdomen showed marked and dramatic wall edema of the whole colon and rectum, ischemia and hyperemia of ascending colon intestinal wall, engorgement of mesenteric vessels, increased attenuation of mesenteric fat, ascites and bilateral ureter-hydronephrosis, demonstrating colon and rectum lupus enteritis (LE). Moreover, laboratory tests revealed lower complement C3 and C4. The titer of antinuclear antibody was 1:100. Overall, whole colon and rectum LE invaded of this case without involving small intestine was clear which was one of the rare manifestations of Systemic lupus erythematosus (SLE). The patient was treated with 10 mg methylprednisolone sodium succinate and 100 mL of 0.9% sodium chloride, hydroxychloroquine (100 mg) and nutrition support. After one week therapy of methylprednisolone and hydroxychloroquine, her symptoms and disease activity of SLE were dramatically improved.
- Citation: Gan H, Wang F, Gan Y, Wen L. Rare case of lupus enteritis presenting as colorectum involvement: A case report and review of literature. World J Clin Cases 2023; 11(34): 8176-8183
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8176.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8176
Systemic lupus erythematosus (SLE) is an immune disease which may involve almost every organ and system in the body, and it shows protean manifestations. The influence of SLE correlating with the digestive organs may show as dental ulcers, protein-losing enteropathy, intestinal pseudo-obstruction, autoimmune pancreatitis, hepatic damage, Lupus Enteritis (LE), and various other complications. The gastrointestinal (GI) system involved in SLE manifests as gastritis, enteritis, colitis, and appendicitis, among others. Approximately half of the SLE-related GI manifestations are abdominal pain, diarrhea, nausea, loss of appetite, and vomiting[1].
LE is an opportunistic complication affecting patients with active SLE. It occurs in critically ill patients who are likely to have a worse prognosis. At present, we use large dose corticosteroid to treat patients of LE successfully as a strategy, leading to symptom improvement and the absence of complications related to infection[2]. Most cases of LE in SLE develop after the diagnosis of SLE, involving the small intestine. Therefore, it is difficult to recognize whether LE involving the colorectum is associated with SLE. A 35 year old woman presented with involvement of the entire colorectum instead of the small intestine, who demonstrated symptom improvement and disease activity after the administration of high-dose corticosteroid therapy.
A 35 year old woman came to the hospital with unexplainable abdominal pain, accompanied by vomiting. The patient had been taking her medication regularly for five years after the diagnosis of lupus nephritis and had been taking medications irregularly until two months prior to the onset of LE. There was no history of intestinal diseases in her family. Our study was approved by the Medical Ethics Committee of Xinqiao Hospital of Army Medical University (No. 2022-125-01) and received informed consent from the patient.
The physical examination upon admission and the pressure of blood, temperature, pulse rate, respiratory rate was normal.
On physical examination, the patient had diffused abdominal pain and pressing pain, without rebound tenderness. Laboratory tests revealed a high antinuclear antibody titer (ANA 1:100) and lower titers of C3 and C4. According to the European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) classification criteria[3,4], which added antinuclear antibodies to the entry criterion and provided an improved SLE diagnosis of combined sensitivity and specificity, the admission criterion ANA was equal or greater (1:80), the kidney biopsy of International Society of Nephrology (ISN) class IV lupus nephritis (diffuse proliferative glomerulonephritis) was 10 score, lower complement C3 and C4 was a score of 4, and the total score was 14 (≥ 10). The diagnosis of SLE was clear[5]. The sensitive indicator of active SLE often was a reduced level of complement C3[6].
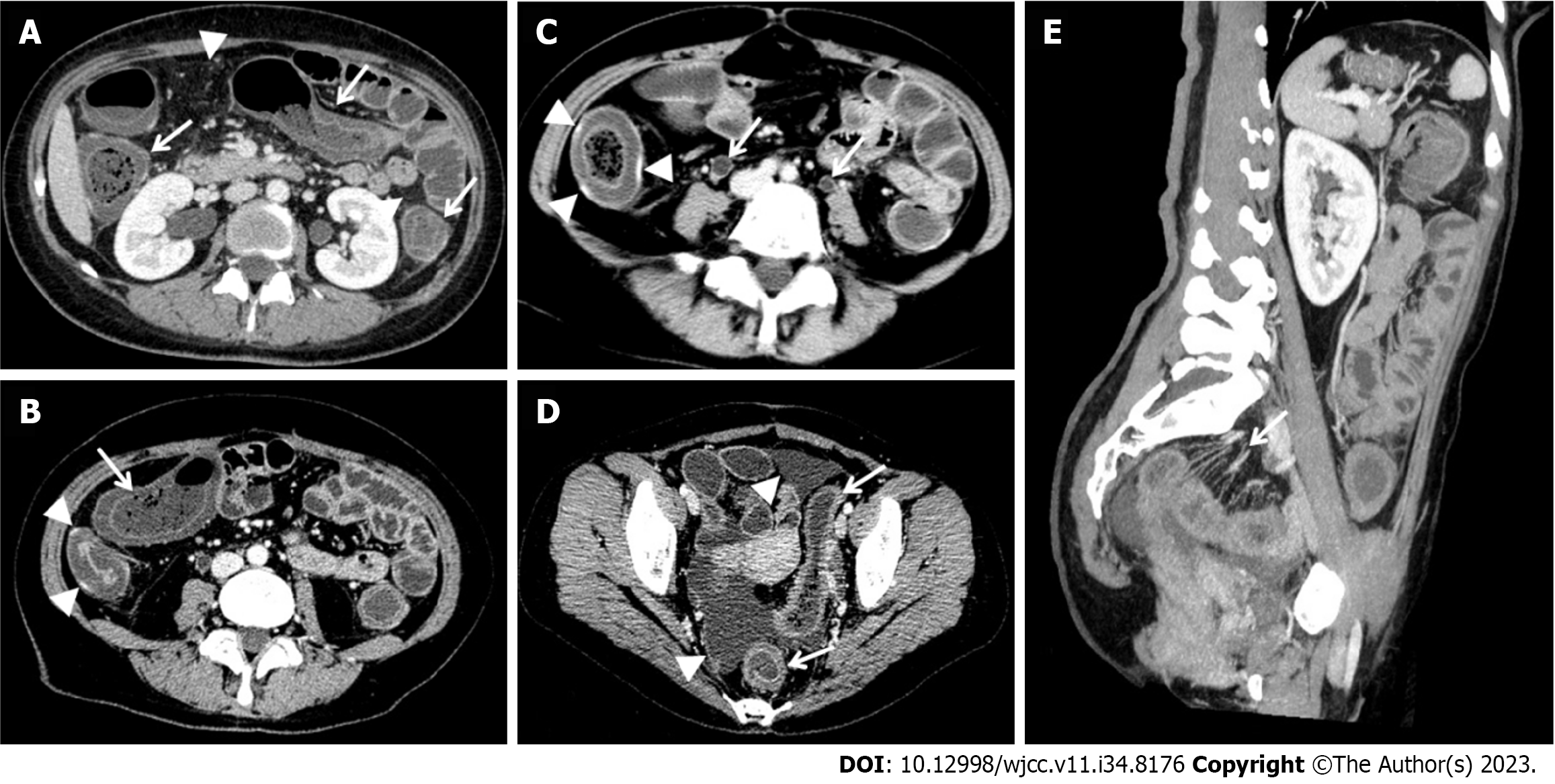
An abdominal contrast enhancement computed tomography (CT) was performed the day after admission. CT showed that there was marked and dramatic whole colon and rectum edema with the target sign or doughnut sign (Figure 1)[7,8], and the thickened intestinal wall was about 4mm to 13mm from the rectum to ascending colon. Ischemic and congestive changes were seen locally in the same bowel (Figure 1A-C), which could be seen as partially discontinuous with the ischemic segment intestinal wall, with gas shadows of a discontinuous mucosal line (Figure 1B). The mesenteric vessels were increased and thickened with the comb sign (Figure 1E)[8,9], which was accompanied by mesenteric fat attenuation (Figure 1A), bilateral ureter-hydronephrosis (Figure 1C) and ascites (Figure 1D).
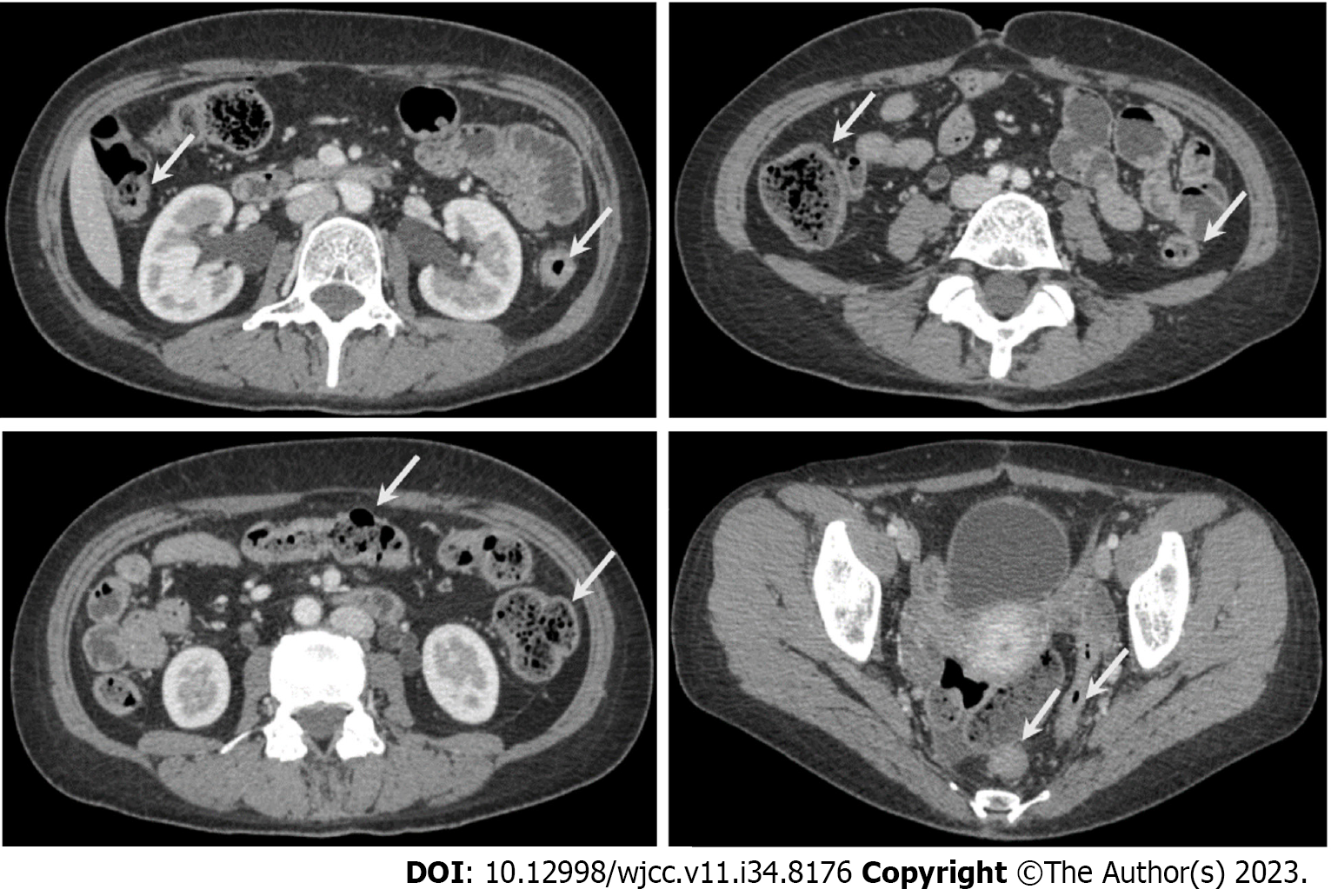
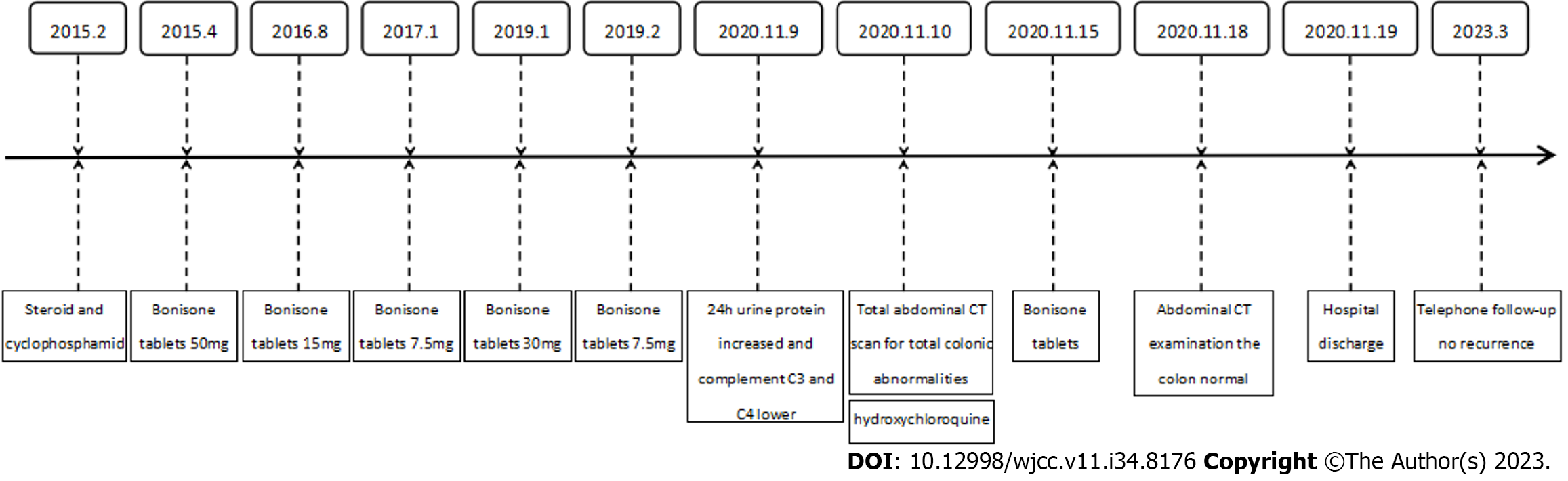
In previous reports, an active disease of SLE was related to flares of LE, so LE was regarded as the expression in SLE. Consequently, we administered 10 mg of methylprednisolone sodium succinate and 100 mL of 0.9% sodium chloride, hydroxychloroquine (100 mg) and nutrition support. After one week of the treatment, the symptoms, laboratory tests, and intestinal abnormalities on CT images were improved. A follow-up CT was performed 7 d before discharge and revealed no abnormal findings (Figure 2). The patient has been treated with a methylprednisolone and hydroxychloroquine tapering. The timeline for treatments and efficacy evaluations of this case is summarized in Figure 3.
She had no family history of intestinal diseases.
The kidney biopsy of ISN class IV lupus nephritis (diffuse proliferative glomerulonephritis).
She has no personal and family history.
On admission, the blood pressure was 93/72 mmHg, the body temperature was 36.5 °C, the pulse rate was 116/min, and the respiratory rate was 20/min.
On physical examination, diffuse abdominal pain and pressing pain, without rebound tenderness.
The admission criterion ANA is equal or greater (1:80), the kidney biopsy of ISN class IV lupus nephritis (diffuse proliferative glomerulonephritis) was 10 scores, lower complement C3 and C4 was 4 scores, the total scores was 14(≥ 10). The diagnosis of SLE is clear. A reduced level of complement C3 is often a sensitive indicator of active SLE.
An abdominal contrast enhancement CT was performed the day after admission. CT showed that there was marked and dramatic whole colon and rectum edema with the target sign or doughnut sign (Figure 1)[7,8], and the thickened intestinal wall was about 4mm to 13 mm from the rectum to ascending colon. Ischemic and congestive changes were seen locally in the same bowel (Figure 1A-C), which could be seen as partially discontinuous with the ischemic segment intestinal wall, with gas shadows of a discontinuous mucosal line (Figure 1B). The mesenteric vessels were increased and thickened with the comb sign (Figure 1E)[8,9], which was accompanied by mesenteric fat attenuation (Figure 1A), bilateral ureter-hydronephrosis (Figure 1C) and ascites (Figure 1D).
The admission criterion ANA is equal or greater (1:80), the kidney biopsy of ISN class IV lupus nephritis (diffuse proliferative glomerulonephritis) was 10 scores, lower complement C3 and C4 was 4 scores, the total scores was 14 (≥ 10). The diagnosis of SLE is clear.
Consequently, we administered 10 mg of methylprednisolone sodium succinate and 100 mL of 0.9% sodium chloride, hydroxychloroquine (100 mg) and nutrition support.
After one week of the treatment, the symptoms, laboratory tests, and intestinal abnormalities on CT images were improved. Follow-up CT was performed 7 d before discharge and revealed no abnormal findings. The patient has been treated with a methylprednisolone and hydroxychloroquine tapering.
However, at the most recent telephone follow-up, the patient presented for abdominal pain again in June 2023, considering the possibility of LE recurrence, the specific treatment was uncertain. Her recurrence was most likely associated with severe thickness of the bowel wall (> 8-9 mm), lupus nephritis and intestinal pseudo-obstruction in those with the large intestine-dominant type[10,11].
SLE had different features and expressions in every organ, such as the skin, kidneys, joints, liver, pancreas, and GI system[12,13]. Various manifestations of vasculitis occur in association with SLE such as stomachache (97%), ascitic fluid (78%), sick (49%), vomitus (42%), diarrhoea (32%), mesenteric vasculitis, protein-losing enteropathy, intestinal pseudo-obstruction, intussusception, and bowel gangrene[14,15]. The diagnosis of SLE has been mostly proposed by the EULAR/ACR 2019 sorting criterion. According to this criterion, the score of our case presented as 14 (≥ 10). The diagnosis of SLE was clear. Based on the typical CT findings of the colon and rectum, the diagnosis of colon and rectum LE is reliable. LE is an intestinal ischemia and congestive disease due to SLE activity involving the intestine.
SLE can affect the entire GI tract, from the oral mucosa to the rectum. The percent of patients of GI tract related symptom is up to 40%-50%[14], but the development of LE is present in only about 0.2% to 5.8% of SLE patients[8,16]. LE involving the jejunum and ileum (83% and 84%, respectively) are relatively common[17,18], but involvement of the colon (19%) and rectum (4%) without involvement of the small intestine is extremely rare[14]. In previous reports, LE has been described as two types: Small intestine-dominant and large intestine-dominant. Small intestine-dominant LE is more frequently seen with biopsy-proven lupus nephritis, with the jejunum and ileum being the most usual involvements reported frequently in the literature. However, the advantage of colon and rectum with or without small intestinal involved) was usually seen in elderly people, as well as in the vesicoureter and conduit involved. This case is the type of large intestine-dominant with extra-intestinal symptoms, such as hydroureter, but the patient of our case also had biopsy-proven lupus nephritis, which is often seen in the small intestine-dominant type[10,11,18]. However, in our case, only the colon and rectum were involved, while the small intestine was uninvolved. As we know, the rectum has a rich and multiple blood supply with two or more different origin vessels, so rectal involvement has been very rarely reported in the PubMed database[19]. As can be seen from the above description, LE of the colon and rectum without small intestinal involvement is extremely rare.
Acute and chronic abdominal pain is always the main LE manifestation, which is present in approximately 50% of cases[7]. The main manifestation of our patient was stomachache and vomiting. The diagnosis of LE was based on the clinical manifestation, laboratory tests and CT images. Now CT scanning has become the gold standard for the diagnosis of LE, which can supply the non-invasive assessment of bowel loops and intestinal blood supply[20]. In our patient, CT showed edema of all the colon and rectum walls with the target sign or doughnut sign, ischemia and hyperemia of transverse colon, ascending colon and descending colon walls. In the arterial phase, obvious spot-enhanced and patchy enhanced areas could be seen in the same colon walls. Gas appears to break through the intestinal wall beneath the ascending colonic wall, which is highly suggestive of perforation. Bowel perforation occurs because of lupus mesenteric vasculitis, which leads to the vessel thrombosis causing bowel wall infarction and perforation[21]. We could also see the mesangial vascular pectinate sign, and the increase in density of mesangial fat, ascites or bilateral ureter-hydronephrosis[18]. The above signs are relatively typical except for ascites, which occurs in 8%-11% of adults with SLE[16].
The diagnosis of LE was not easy, with no obvious active characteristic in SLE. LE may be considered if three of the following signs are presented on CT: Fluid levels, bowel wall thickening of ≥ 3 mm, the target sign or doughnut sign, dilatation of intestinal segments, mesenteric edema, mesangial angiitis, pectinate sign, increased mesangial fat attenuation and ascitic fluid[21-24]. The patient of our case had a definite history of SLE for five years and typical CT findings of the colon and rectum. Other causes of acute abdomen non-SLE-related and relation of SLE had been screened out, so the consideration of colon and rectum LE was relatively easy.
However, the above CT findings of bowel wall and mesenteric ischemia are quite common and lack specificity because these signs can also be seen in inflammatory bowel disease such as Crohn’s disease (CD), which can mimic LE. LE and CD have similar features like the "comb sign" and share clinical symptoms including abdominal pain and diarrhea. The endoscopic appearance and pathological examination are important ways to distinguish between the two diseases[25]. There were obvious characteristics with discrete areas of CD with cobblestoning. The common pathological features generally are focal crypt irregularity and inflammatory epithelial-giant cell granulomas. There are also some distinct features of CD on CT examination, such as bowel expansion, curve, and broadening of the mesareic arteries[9]. Also, the most common area of CD is the ileocecum. Colorectal involvement of CD is relatively rare and is often accompanied with involvement of other parts.
Although we don’t know the relationship between LE and angeitis completely, especially small or middle sized vessels injury causes, lupus mesenteric vasculitis (LMV), thrombosis, hypocomplementemia, inflammatory, immune-mediated diffuse smooth muscle dysfunction, immune dysregulation and SLE itself[7,26]. High disease activity and a long-standing history of SLE in patients usually causes LMV to occur[27]. Arteritis and venulitis of the colon and rectum may be the result of aggravation of SLE. Vasculitis is the most common cause of mucosal damage[22].The deposition of immune complexes in the vascular endothelium, arterial muscular and elastic elements by circulation autoantibodies may lead to leukocytoclastic vasculitis[10,24,28], thrombosis and vasculitis of vessels supplying of the intestine vessels walls and the target organ[8,29]. The involvement of the renal and intestinal small vessels may be the major cause due to the autoimmune disorder and active SLE, especially when other causes have been excluded[30]. There was also an article that suggested “visceral pseudo-obstruction" and vasculitis of the visceral smooth muscles leading to muscular damage may encompass the SLE GI involvement[26]. Among the extra-GI involvements, the urinary tract was the most frequently affected compartment[30]. Lupus nephritis can be concomitant with LE, which is present in about 65% of LE cases[8,15,22].
The patient had a history of immunosuppressive therapy for her SLE during the last five years. Irregularly taking medication for two months before the onset of LE was most likely the predisposing factor. A medication's side effects are also a factor causing LE[18]. Drug therapy leads to immune complex deposition, resulting in thrombosis of small mesenteric vessels, which causes submucosal edema and ischemia in the colon and rectum[19].
We observed thrombosis in this patient due to SLE. SLE patients are prone to thromboses and angeitis. Mesenteric inflammatory veno-occlusive disease is another rare cause of LE in patients, and it is detected on abdominal CT[2]. We considered that the angeitis may be the vital pathological features of our patient due to the marked improvement of the patient with hormone therapy.
There are few reports of secondary manifestations involving the colon and rectum of SLE. Generally, GI involvement is an important manifestation of reignition that occurs in someone with SLE. Typically, their average age range is 15-44 years[31]. Almost all patients were treated with high-dose corticosteroids and responded successfully to treatment.
The complication of SLE associated with LE involves high necrosis and perforation, and even death, with a mortality of 2.7%[15]. Due to the risk of eating tetter and treatment with large dose immune suppression treatment. LE patients have a higher rate (31.3%) of infectivity, as reported by the latest reported studies, which is one of the reasons for the majority of LE deaths[10]. The diagnose is difficult when it is only through the results of clinic and laboratorial, while CT manifestations are quite typical, so we should combine the CT images to improve the diagnosis accuracy. In the past, laparotomy or laparoscopy has been considered. However, corticosteroids play a crucial role in control of SLE symptoms of patients[32]. Corticosteroids therapy has been successfully used as the initial treatment, reducing surgical intervention. Hydroxychloroquine may reduce the risk of lupus flares and organ damage. Dose tapering should be slowed to avoid recurrence[13]. Most patients were in remission after treatment without recurrence. The literature reported that patients with bowel wall thickness ≥ 8-9 mm may experience recurrence, which is up to 23% of the LE cases. Koo et al[33] have identified colon and urinary tract involvement (especially lupus cystitis) was also the main risks factors of recurrence[5,10,33,34], because of lupus cystitis and LE, and there was a strong correlation in the pathogenesis[35]. According to the basic manifestations and danger elements, the patient was reposeful because of the significant improvement with drug treatment, and there were no confirmed recurrences during follow-up from November 2020 to May 2023. Large dose methylprednisolone and hydroxychloroquine may be the original strategies in LE of SLE. However, at the most recent telephone follow-up, the patient presented for abdominal pain again in June 2023; and after considering the possibility of LE recurrence, the specific treatment was uncertain. Her recurrence was most likely related to obvious intestinal wall thickness (> 9 mm), lupus nephritis and a pseudo bowel block in the colon and rectum[10,11].
The patient of our case presented with colorectal LE with main features of SLE. There was successful treatment by methylprednisolone and hydroxylation drugs. In spite of the rarity of SLE cases where the only GI involvement being due to colon and rectum LE, we should be aware of it and the severe activity of SLE, which can manifest as intestinal symptoms after exclusion of infection, and this can help avoid unnecessary ineffective interventions and potentially fatal complications[30]. Prolonged intestinal wall edema can lead to intestinal necrosis, intussusception, perforation, and an even more serious abdominal infection that can endanger the patient’s life. As we know, SLE is a common autoimmune disease, and its important features are autoantibodies and autoreactive T lymphocytes that may be activated at any time[6]. Therefore, we should also closely observe the possible recurrence of patients, which may be the manifestation of enteritis, or the corresponding symptoms of involvement of other abdominal organs, such as autoimmune pancreatitis, liver damage, cholecystitis, and cystitis.
As the initial treatment for colon and rectum LE related to SLE, we can use high-dose methylprednisolone and hydroxychloroquine for treatment combining general manifestation and individual dangerous element. We should emphasize that colon and rectum involvement may occur independently in LE, so it is critical to diagnose it early to prevent devastating organ damage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dauyey K, Kazakhstan S-Editor: Li L L-Editor: A P-Editor: Zhang XD
| 1. | Li YF, Wei MJ. Acute pancreatitis in childhood-onset systemic lupus erythematosus: Case report. Arch Argent Pediatr. 2019;117:e279-e283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Lee J, Lee YJ, Kim Y. Acute acalculous cholecystitis as the initial manifestation of systemic lupus erythematous: A case report. Medicine (Baltimore). 2021;100:e26238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, Smolen JS, Wofsy D, Boumpas DT, Kamen DL, Jayne D, Cervera R, Costedoat-Chalumeau N, Diamond B, Gladman DD, Hahn B, Hiepe F, Jacobsen S, Khanna D, Lerstrøm K, Massarotti E, McCune J, Ruiz-Irastorza G, Sanchez-Guerrero J, Schneider M, Urowitz M, Bertsias G, Hoyer BF, Leuchten N, Tani C, Tedeschi SK, Touma Z, Schmajuk G, Anic B, Assan F, Chan TM, Clarke AE, Crow MK, Czirják L, Doria A, Graninger W, Halda-Kiss B, Hasni S, Izmirly PM, Jung M, Kumánovics G, Mariette X, Padjen I, Pego-Reigosa JM, Romero-Diaz J, Rúa-Figueroa Fernández Í, Seror R, Stummvoll GH, Tanaka Y, Tektonidou MG, Vasconcelos C, Vital EM, Wallace DJ, Yavuz S, Meroni PL, Fritzler MJ, Naden R, Dörner T, Johnson SR. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019;71:1400-1412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 560] [Cited by in RCA: 1370] [Article Influence: 228.3] [Reference Citation Analysis (0)] |
| 4. | Jayawickreme KP, Subasinghe S, Weerasinghe S, Perera L, Dissanayaka P. A young girl with chronic isolated cervical lymphadenopathy found to have lupus lymphadenopathy, progressing to develop lupus nephritis: a case report. J Med Case Rep. 2021;15:328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Liao JL, Zha FY, Smyth B, Xiong ZY. A 28-Year-Old Woman Presenting with a Clinical Flare of Systematic Lupus Erythematosus and Abdominal Pain Due to Rectus Sheath Hematoma. Am J Case Rep. 2022;23:e935472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Chen L, He Q, Luo M, Gou Y, Jiang D, Zheng X, Yan G, He F. Clinical features of lupus enteritis: a single-center retrospective study. Orphanet J Rare Dis. 2021;16:396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 7. | Shrestha BM, Shrestha S, Kharel S, K C A, Pradhan S, Bhandari RS. Ileal perforation as an initial manifestation of systemic lupus erythematosus: A case report. Int J Surg Case Rep. 2021;87:106409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Ronen JA, Mekala A, Wiechmann C, Mungara S. A Flare-up of Systemic Lupus Erythematosus with Unusual Enteric Predominance. Cureus. 2020;12:e7068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Zhu XL, Xu XM, Chen S, Wang QM, Zhang KG. Lupus enteritis masquerading as Crohn's disease. BMC Gastroenterol. 2019;19:154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Muñoz-Urbano M, Sanchez-Bautista J, Ramírez A, Santamaría-Alza Y, Quintero-González DC, Vanegas-García AL, Vásquez G, González LA. Lupus enteritis: A 10-year experience in a single Latin American center. Lupus. 2023;32:910-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Tsuda S, Nagata J, Yamaguchi T, Cho T, Mori T, Yokota M, Fujimoto R, Hirose S, Ito H, Wakabayashi T, Yamamoto S, Watanabe N, Suzuki T. A Case of Lupus Enteritis in Which Multiple Colorectal Ulcers Were the Only Signs of Relapse. Tokai J Exp Clin Med. 2022;47:194-198. [PubMed] |
| 12. | Wen J, Chen W, Gao L, Qiu X, Lin G. Systemic lupus erythematosus simultaneously presenting with visceral muscle dysmotility syndrome and mechanical intestinal obstruction clinically relieved by surgery: a case report and literature review. BMC Gastroenterol. 2022;22:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Zhou JB, Chen WB, Zhu F. Hepatic Rupture Induced by Spontaneous Intrahepatic Hematoma. Case Rep Surg. 2018;2018:2026846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Alshehri AM, Alhumaidi HM, Asseri YM, Ahmed MEK, Omer HA. Mesenteric Vasculitis as a Rare Initial Presentation of Systemic Lupus Erythematosus: A Case Report. Saudi J Med Med Sci. 2020;8:223-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Gonzalez A, Wadhwa V, Salomon F, Kaur J, Castro FJ. Lupus enteritis as the only active manifestation of systemic lupus erythematosus: A case report. World J Clin Cases. 2019;7:1315-1322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (2)] |
| 16. | Shadhu K, Ramlagun D, Ping X. A rare case of laparoscopy towards SLE with lupus mesenteric vasculitis induced ascites. BMC Surg. 2019;19:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Potera J, Palomera Tejeda E, Arora S, Manadan AM. Lupus Enteritis: An Uncommon Presentation of Lupus Flare. Cureus. 2021;13:e18030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 18. | Atıcı SD, Engin Ö, Akpınar G, Tuğmen C. Corticosteroid associated lupus pancreatitis. Rev Assoc Med Bras (1992). 2020;66:1414-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Ezhilnilavan S, Priyamvada PS, Haridasan S, Rajesh NG, Parameswaran S. Acute gastric dilatation in a patient with lupus nephritis: An uncommon presentation of lupus mesenteric vasculitis. Saudi J Kidney Dis Transpl. 2018;29:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Liang Y, Di Re A, El Khoury T. A rare case of lupus-related gastrointestinal vasculitis presenting as rectal gangrene. J Surg Case Rep. 2019;2019:rjz128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Latif E, Musthafa S, Ahmed A, Abu Amr A. Stercoral Perforation of Sigmoid Colon in Systemic Lupus Erythematosus: A Rare Cause of Peritonitis. Cureus. 2020;12:e9495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Mauro A, Giani T, Di Mari C, Sandini M, Talenti A, Ansuini V, Biondi L, Di Nardo G, Bernardo L. Gastrointestinal Involvement in Children with Systemic Lupus Erythematosus. Children (Basel). 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Bindukumari Sureshkumar N, Gopinath P, Joshi A, Alumparambil Surendran S. Recurrent Lupus Enteritis While on Chronic Immunosuppressant Therapy. Cureus. 2022;14:e30149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 24. | Pavli P, Gioti O, Spyridopoulos TN, Katsikas G, Tsourous G, Elezoglou A, Kaziani K, Fanouriakis A. Acute Abdominal Situations as Presenting or Flaring Manifestations of Systemic Lupus Erythematosus: A Case Series. Mediterr J Rheumatol. 2022;33:339-345. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 25. | Yeh H, Wu RC, Tsai WS, Kuo CJ, Su MY, Chiu CT, Le PH. Systemic lupus erythematosus complicated by Crohn's disease with rectovaginal fistula. BMC Gastroenterol. 2021;21:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 26. | Chen Z, Zhou J, Li J, Zhou Y, Wang X, Li T, Gu L, Sun F, Wu W, Xu W, Sun S, Chen J, Lu L, Zhang W, Zhao Y, Ye S. Systemic lupus erythematosus gastrointestinal involvement: a computed tomography-based assessment. Sci Rep. 2020;10:6400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Alsolaimani R. Mesenteric Vasculitis and Urinary System Involvement Presenting As the Initial Manifestations of Systemic Lupus Erythematosus Treated Successfully With Glucocorticoids and Rituximab: A Case Report. Cureus. 2022;14:e31474. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Yamaguchi T. Characteristic target sign of the small intestine in a case of lupus enteritis. J Gen Fam Med. 2022;23:187-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Zhao Y, Jia X, Tong X, Niu G, Wang R, Liu L, Zhou F. Spontaneous perirenal hemorrhage in systemic lupus erythematosus: a rare case report and literature review. BMC Nephrol. 2021;22:217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 30. | Canale V, Minutoli F, Lucisano S, Bottari A, Zappulla Z, Cernaro V, Lupica R, Buemi M, Santoro D. [Lupus Nephritis and Enteritis, a dual simultaneous involvement with Arteriolar Thrombosis]. G Ital Nefrol. 2015;32. [PubMed] |
| 31. | Jin X, Wang G, Xu X, Bai Y, An R, Jiang D. Coexistence of Crohn's disease and systemic lupus erythematosus: a case report and literature review. Eur J Gastroenterol Hepatol. 2020;32:1256-1262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Barahimi E, Abbasi T, Hesarooeyeh ZG, Raad H, Karimi M, Shahi M. Colonic basidiobolomycosis in a patient with systemic lupus erythematosus (SLE). BMC Infect Dis. 2022;22:740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 33. | Koo BS, Hong S, Kim YJ, Kim YG, Lee CK, Yoo B. Lupus enteritis: clinical characteristics and predictive factors for recurrence. Lupus. 2015;24:628-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Halilu F, Qureshi A, Nash B. Lupus Enteritis in the Absence of a Lupus Flare. A Case Report and Review of Literature. J Community Hosp Intern Med Perspect. 2022;12:73-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 35. | Wang G, Zhuo N, Tian F, Li J, Wen Z. Two complications in patients with systemic lupus erythematosus: lupus cystitis and lupus enteritis. Arch Med Sci. 2022;18:822-824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |