Published online Nov 26, 2023. doi: 10.12998/wjcc.v11.i33.8065
Peer-review started: September 7, 2023
First decision: October 17, 2023
Revised: November 5, 2023
Accepted: November 17, 2023
Article in press: November 17, 2023
Published online: November 26, 2023
Processing time: 77 Days and 19.4 Hours
Female anorectal malformation is a correctable congenital defect. Delayed manifestations in patients with anal deformities are uncommon, especially after adolescence.
The clinical data of a 19-year-old adult female patient with congenital anal atresia accompanied by rectovestibular fistula as the main manifestation was retrospectively analyzed. Diagnosis was made based on the patient's clinical symptoms, signs, imaging showing the fistula, X-ray and magnetic resonance imaging results. The preoperative examination was improved. Anorectoplasty was performed. The patient exhibited an improvement in quality of life and presented no evidence of fecal incontinence during the 6-mo follow-up.
Transfistula anorectoplasty is a reasonable and reliable surgical method for the treatment of adult congenital anal atresia and rectovestibular fistula.
Core Tip: This paper reports the case of an adult patient with congenital anal atresia combined with rectovestibular fistula who underwent transfistulae anorectoplasty with clear visual field exposure the ability to separate the rectovaginal septum under direct vision, greatly reducing the possibility of vaginal injury, ensuring the integrity of the sphincter, and causing minimal intraoperative damage to normal tissues. It is a reasonable and reliable surgical method for the treatment of congenital anal atresia and rectovestibular fistula.
- Citation: Wang J, Zhang XY, Chen JH, Jin HY. Treatment of adult congenital anal atresia with rectovestibular fistula: A rare case report. World J Clin Cases 2023; 11(33): 8065-8070
- URL: https://www.wjgnet.com/2307-8960/full/v11/i33/8065.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i33.8065
Anorectal malformation (ARM) is a common deformity in children, and anal atresia is the main manifestation of it, with a morbidity of 1/5000-1/1500[1,2]; 75%-95% of patients have fistula, which occurs more frequently in women than men. Congenital anal atresia with rectovaginal fistula is most common in females, while congenital anal atresia with rectoperineal fistula is most common in males[3]. At present, the pathology and pathogenesis of ARM are not completely clear, and it is mainly caused by developmental disorders of the enteric nervous system and perianal muscles during the embryonic period. Most children with ARM undergo complete anorectoplasty at preschool age, and the prognosis is generally good. However, it is rarely reported that anoplastic surgery is performed in adulthood, as reported below.
A 19-year-old unmarried Chinese woman presented to the anorectal surgery clinic with a complaint of congenital anal atresia from birth.
Abdominal pain and distension appeared again 6 d prior and could not be relieved.
The patient had a history of abdominal distension caused by constipation, and unformed loose stools were produced during defecation. At the age of 1 year, she was diagnosed but was not treated. Four months before admission, the patient was found to have abnormal bowel habits for 2-4 d a month, and the symptoms of abdominal pain and distension were relieved after resolving a large amount of loose stool. Computed tomography (CT) examination revealed intestinal obstruction, colon and rectum dilation with a large amount of contents, intestinal wall edema and thickening.
The patient denied any family history of intestinal diseases.
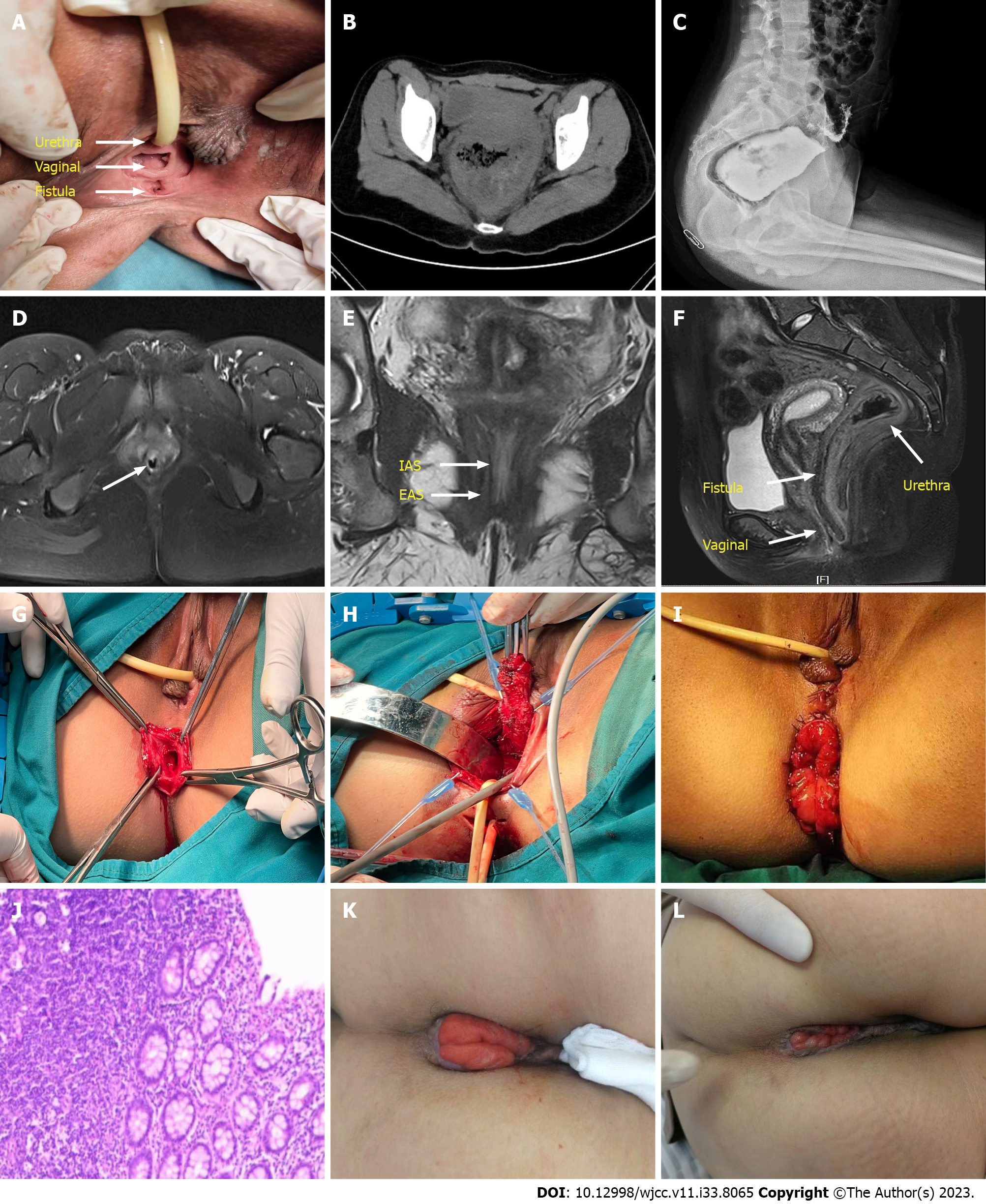
Physical examination on admission: There were no abnormalities in the general examination of skin and mucosa; however, the physical examination of the perineum showed that there was no anus in the normal anal position, but there was an anal incisure, and a red and swollen defecation fistula measuring 10 mm in diameter in the rectovestibular, and no abnormalities in the location or appearance of the labia majora, labia minora, vagina or urethra opening (Figure 1A).
No abnormality was found in routine blood and urine analyses.
Auxiliary examination: (1) Abdominal CT: Rectal dilation with intestinal wall thickening, with a maximum diameter of approximately 10 cm (Figure 1B); (2) X-ray imaging: The distal end of the rectum was the blind end and located approximately 6 cm away from the anal notch (Figure 1C); (3) pelvic MRI: A gap was visible in the upper section of the transverse anal canal (Figure 1D), the thickness of the internal sphincter of the anus was approximately 1 mm in the coronal position, some of the internal sphincter was discontinuous, the thickness of the external sphincter was approximately 2 mm in the sagittal position (Figure 1E), the positions of the rectum, vagina and fistula were visible in the sagittal position, and the fistula was adjacent to the posterior wall of the vagina (Figure 1F).
Combined with the patient’s medical history, the final diagnosis was congenital anal atresia with a rectovestibular fistula.
Postoperatively, the patient recovered well. The incision completely healed (Figure 1K) during the 2 mo after the operation. Anorectal manometry showed that the anal tube pressure at rest was low, with an average of 24 mmHg, while the anal tube resting pressure was low when squeezed, the duration was shorter than normal, and the anal stool control ability was weakened. The initial rectal sensation, initial bowel intention and maximum tolerance threshold were high, indicating a decrease in rectal sensitivity.
At the 4-mo follow-up, the rectal mucosa was almost retracted (Figure 1L). The resting pressure of the anal canal reached 48 mmHg after 2 courses of pelvic floor rehabilitation treatment. At present, the patient has undergone stoma closure and defecates 3 to 5 times a day without fecal incontinence.
Congenital anal atresia is one of the most common malformations in children, especially newborns. It is most common in female infants. Up to 95% of female cases may be complicated with fistula, among which congenital anorectal combined with rectovaginal fistula or vestibular fistula is more common. Congenital anal atresia occurs more frequently in eastern China than in central and western China, which may be related to environmental pollution[4] and gene mutations[5]. Anal malformation is a correctable congenital malformation that can have a good prognosis. Most of these abnormalities can be easily detected in the clinical examination of newborns, and most patients are surgically treated in infancy. It is rare for this patient to be treated at age 19. The main reason for the delay in surgery is the patient’s parents. Moreover, the severity of the deformity increases with age, and its clinical manifestations are mainly constipation. Long-term constipation can be secondary to megacolon, and the operation is more difficult.
On the one hand, whether patients with congenital anal atresia can obtain good anal function after surgery depends on whether the pelvic floor muscles are developed, and more importantly, whether the anatomical structure of the rectal canal is restored through reasonable operation, and whether damage to the pelvic tissue is minimized, which reduces the risk of damage to the defecation receptors so as to ensure a normal defecation reflex after surgery.
Pena et al[6] originally proposed that anal atresia should be operated in three stages, namely, first-stage fistulae, second-stage anorectoplasty and third-stage fistula closure. The purpose is to avoid infection during anal reconstruction and subsequent anal retraction, anal stenosis, and fistula recurrence. In recent years, most scholars have advocated that one-stage surgery, despite the high risk of incision infection, can reduce the number of operations, reduce treatment costs, and avoid complications such as skin erosion, wound infection, and ostomy prolapse[7]. However, the patient was admitted to the hospital for emergency ileus, and the problems of difficult defecation and nutritional problems should be solved first. It is necessary to fully evaluate the condition and blindly performing a one-stage operation, which may lead to an increased incidence of anastomotic fistula and an increased chance of infection, leading to the failure of the operation.
The common surgical methods for congenital anal atresia with rectovestibular fistula include anterior and posterior sagittal approach anorectoplasty. The advantages are that the surgical field is wide and the operation is performed under direct vision. However, the surgical injury is large, the operation time is long, and the incision infection rate is high. Incision of the sphincter is needed during the operation, which increases the probability of postoperative fecal incontinence. Patients with poor stool control function are prone to rectal mucosal prolapse. Transfistula anorectoplasty is advantageous in that it causes less trauma, has a short operation time, and is safe. The integrity of the sphincter is not compromised; the procedure does not damage the important nerves or blood vessels on the side or back of the rectum. The fistula was completely resected in the patient, and no fistula recurrence was observed during postoperative follow-up. Therefore, the technical requirements for resection of a free fistula are high, and the fistula must be completely and carefully resected.
The patient was an adult with disuse sphincter atrophy, which may have poor stool control function after surgery. During the operation, the remaining muscle should be protected and utilized as much as possible, and the physiological and anatomical position of the rectum should be restored as much as possible, which is the key to obtaining good postoperative stool control ability. After fistula resection, vestibular area repair can also achieve good cosmetic results.
The most common complication after anorectoplasty is poor defecation control, with an incontinence rate as high as 10%-75%. Some surgeons have noted that the distal rectum lacks normal innervation and a muscle layer. To ensure good anal function after surgery, it is recommended to remove at least 3 cm of the distal rectum, while some scholars believe that the distal rectum should have an internal sphincter structure[8]. Pathological studies have shown that patients with congenital anal atresia have abnormal changes at the end of the rectum, such as dysplasia of ganglion cells in the intestinal wall, muscle fibrosis in the rectal wall and no relaxation reflex of the internal rectal sphincter, and even postoperative development of intractable constipation secondary to megacolon, requiring surgical treatment. The absence of expression of ganglion cells and Cajal interstitial cells will affect the signal transmission process of the bowel defecation reflex after surgery, thus affecting postoperative defecation dysfunction[9]. In this patient, rectal inflammation and thickening were obvious, and the function was poor. The distal diseased rectum was removed during the operation, and a new rectum was rebuilt.
Because the patient has not defecated in a normal position for many years, the thickness of the sphincter is significantly reduced compared with that of normal people, so there is a high possibility of postoperative anal dysfunction. Anorectal manometry at 2 mo postoperatively showed that the anorectal resting pressure and contraction pressure were both lower than the normal range. The patient was advised to actively perform pelvic floor rehabilitation and anal lift training exercises before the fistula closure procedure to enhance their bowel control ability. After anal lift training, the rectal mucosa was more retracted than before. Some surgeons’ excessive aesthetic pursuits lead to postoperative rectal retraction and narrowing. In addition, the patient was an unmarried woman who would later become pregnant and give birth, and cesarean section may be a safer operation for her to prevent damage to the anal sphincter and vagina.
In short, treatment of anal atresia is relatively rare after adulthood. The patient underwent transfistulae anorectoplasty with clear visual field exposure and the ability to separate the rectovaginal septum under direct vision, greatly reducing the possibility of vaginal injury and ensuring the integrity of the sphincter. It is a reasonable and reliable surgical method for the treatment of congenital anal atresia and rectovestibular fistula and is worth clinical promotion and application. However, the patient is more likely to experience anal dysfunction in the long term. Regular pelvic floor rehabilitation training is recommended, and further follow-up is needed.
The authors thank the patient who consented to having her data published in this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hidaka E, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Rintala RJ. Congenital anorectal malformations: anything new? J Pediatr Gastroenterol Nutr. 2009;48 Suppl 2:S79-S82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Wang JH, Zhao XW, Dai CJ. Clinical application of laparoscopic assisted primary arthroplasty of high anal atresia. Guangdong Med. 37:876-878. [DOI] [Full Text] |
| 3. | Bhatnagar S. Anorectal malformations (part 1). J Neonatal Surg. 2015;4:7. [PubMed] |
| 4. | Yuan P, Qiao L, Dai L, Wang YP, Zhou GX, Han Y, Liu XX, Zhang X, Cao Y, Liang J, Zhu J. Spatial distribution patterns of anorectal atresia/stenosis in China: use of two-dimensional graph-theoretical clustering. World J Gastroenterol. 2009;15:2787-2793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Priyatini T, Roziana. Transfistula anorectoplasty on adult female anorectal malformation: A rare case report. Int J Surg Case Rep. 2020;74:182-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 6. | deVries PA, Peña A. Posterior sagittal anorectoplasty. J Pediatr Surg. 1982;17:638-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 331] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Amanollahi O, Ketabchian S. One-stage vs. three-stage repair in anorectal malformation with rectovestibular fistula. Afr J Paediatr Surg. 2016;13:20-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Lombardi L, Bruder E, Caravaggi F, Del Rossi C, Martucciello G. Abnormalities in "low" anorectal malformations (ARMs) and functional results resecting the distal 3 cm. J Pediatr Surg. 2013;48:1294-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Zhan JH, Hu B, Luo X. Clinicopathological study of remote rectal resection of congenital anal atresia. Zhonghua Xiaoer Waike Zazhi. 2011;32:154-156. [DOI] [Full Text] |