Published online Nov 6, 2023. doi: 10.12998/wjcc.v11.i31.7732
Peer-review started: September 19, 2023
First decision: September 20, 2023
Revised: September 22, 2023
Accepted: October 17, 2023
Article in press: October 17, 2023
Published online: November 6, 2023
Processing time: 48 Days and 6.2 Hours
We report on the case of a 21-year-old female who could not walk due to a huge Bartholin's cyst occupying the right vulvar region. The patient was treated by marsupialization of the Bartholin’s cyst and postoperative antibiotic therapy.
A 21-year-old female without a medical history of sexually transmitted diseases presented to our outpatient clinic with complaints of a painful vulvar lump and a green-yellowish discharge for 4 d. A large Bartholin’s cyst, 10 cm in diameter, was suspected over the right side of the vulva. She was advised to be admitted to the ward for intravenous antibiotic treatment and to perform marsupialization several days later. However, the patient requested immediate surgery because of time limitations. The patient underwent marsupialization under local anesthesia. The procedure was well-tolerated. After making the incision, a significant amount of malodorous pus (approximately 30 mL) was removed from the abscess. The patient was followed up for 1 wk postoperatively. The Bartholin’s cyst regressed, and the surgical wound healed well.
Our case shows that an initial marsupialization followed by oral antibiotic therapy can be an appropriate treatment option for a large Bartholin’s cyst. However, depending on the patient’s condition, a suitable treatment, either cystectomy or marsupialization, can be considered.
Core Tip: We report on a case of a large Bartholin’s cyst. We present updated information regarding the symptoms, signs, diagnosis, and treatment of this condition. Because of the rarity of large Bartholin’s cysts, we developed a strategy to diagnose and treat this type of cyst.
- Citation: Li HY, Ding DC. Huge Bartholin’s cyst managed by primary marsupialization: A case report. World J Clin Cases 2023; 11(31): 7732-7737
- URL: https://www.wjgnet.com/2307-8960/full/v11/i31/7732.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i31.7732
Bartholin’s cysts occur when the ducts of the Bartholin’s glands are blocked, preventing fluid drainage. This blockage leads to the formation of a fluid-filled cyst. These cysts can vary in size and may or may not cause symptoms[1].
The Bartholin’s glands are located on either side of the vaginal opening and respond to vaginal lubrication. The most common symptoms include pain or discomfort in the vaginal area, swelling near the vaginal opening, and sometimes redness or tenderness[2].
The exact cause of a Bartholin's cyst is unclear; however, they can result from infection, trauma, or irritation of the Bartholin's glands. In some cases, they may develop spontaneously without an apparent cause.
A physical examination can be performed to diagnose Bartholin’s cysts. In some cases, further tests, such as a biopsy, may be required to rule out other conditions. Bartholin’s cysts or abscesses are vulvar lesions in 2%–3% of adult females. Bartholin’s cysts are usually 2–4 cm in diameter[3].
Treating large Bartholin's cysts can be controversial in the medical field owing to several factors and considerations[4]. One controversy is deciding when to intervene. Some doctors argue for immediate surgical drainage to relieve patient discomfort and prevent infection. Others believe in a more conservative approach, opting to wait and see if the cyst resolves independently before pursuing surgical intervention[5].
Treatment options depend on the size of the cyst and the presence of symptoms. Small asymptomatic cysts may not require treatment and can resolve spontaneously. Warm sitz baths and pain relievers can help ease the discomfort. If the cyst is large, painful, or infected, drainage may be recommended, which involves making a small incision to drain the fluid. Surgery to remove the cyst or the entire Bartholin’s gland may sometimes be necessary. A simple Bartholin’s cyst may require marsupialization and antibiotic therapy is not usually recommended[6].
However, the standard treatment for a large Bartholin’s cyst is poorly understood[7,8]. Herein, we report on the case of a 21-year-old female with a large Bartholin’s cyst occupying the right vulvar region, which was treated with marsupialization and postoperative antibiotic therapy.
A 21-year-old female presented to our hospital with a 4-d history of a painful vulval lump with green-yellowish discharge.
The patient visited the emergency room because she could not walk owing to the painful vulvar mass and required a wheelchair. She had a sickly appearance. A vulva abscess was suspected, and the patient was subsequently transferred to our outpatient department for further evaluation. Her medical history indicated an absence of recent sexual activity and no reported incidents of trauma or injury. She reported regular menstrual periods and was noted to be nulliparous.
No known drug allergy history was noted. She had no surgical history.
The patient experienced menstrual cycles lasting approximately 7 d every 28–30 d. No notable medical conditions in her family history existed, and she had no previous history of sexually transmitted diseases.
Vital signs were as follows: temperature of 36 °C; respiration of 16 breaths/min; pulse rate of 58 beats/min; and blood pressure of 95/62 mmHg. No pale conjunctiva was noted. The heart-lung examination was normal. Additionally, no tenderness or rebound pain over the abdomen was noted. A vaginal examination revealed a painful, tender lump on the right side of the vulva, approximately 10 cm in diameter. We observed redness in the area on the right side of the vulva. Additionally, there was a slight green-yellowish vaginal discharge present.
Complete blood and differential counts were all within normal limits (white blood cell: 9.62 103/mL, and neutrophil and lymphocyte percentages were 65.4% and 26.0%, respectively). Electrolytes and coagulation profiles were all within normal limits. The above values indicated that no systemic infection was present.
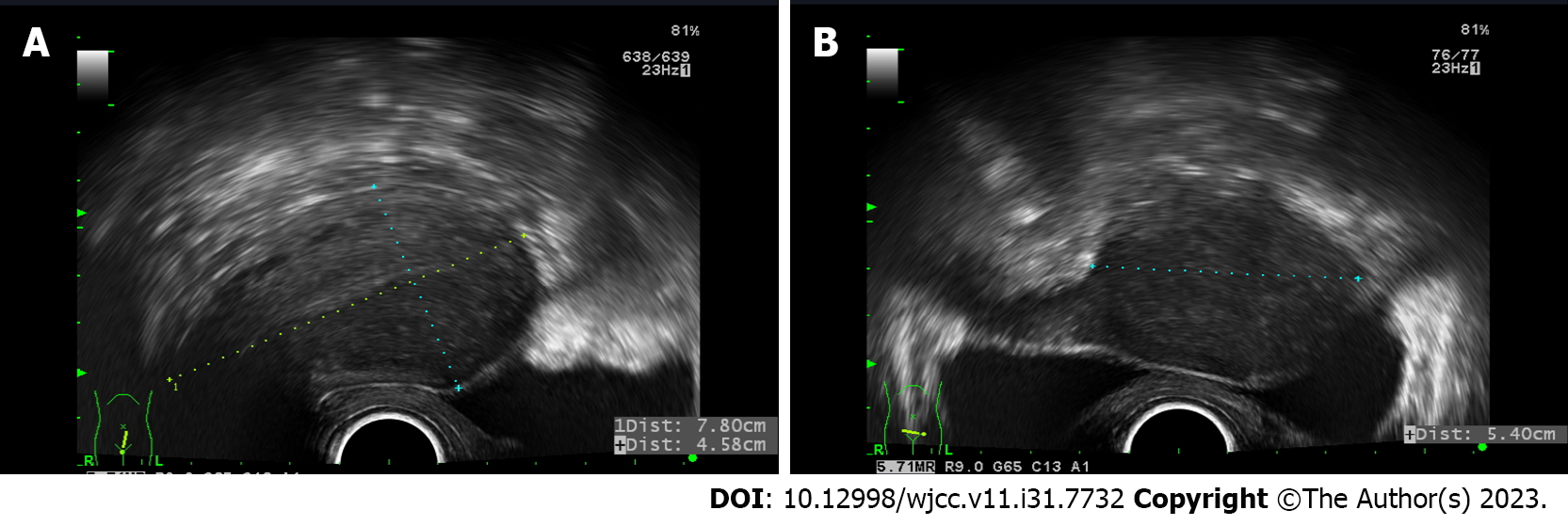
Pelvic ultrasound revealed an anteverted 7.8 cm × 4.5 cm × 5.4 cm uterus with a thin endometrium (Figure 1). The adnexa appeared normal.
The patient was diagnosed with a large Bartholin’s cyst in the right vulvar region (Figure 2A).
Admission to the ward for initial intravenous antibiotic treatment, followed by marsupialization scheduled for a few days later, was recommended. Nevertheless, the patient declined admission because of time constraints and instead requested immediate surgery. Marsupialization was performed under local anesthesia (Figure 2B and C). The patient was placed in a lithotomy position, and the Bartholin's gland abscess was exposed. Local anesthesia using 1% xylocaine was administered in the introitus area near the Bartholin’s duct. A scalpel was used to create an incision in the cyst wall to facilitate fluid drainage and alleviate pressure. After making the incision, a significant amount of malodorous pus (approximately 30 mL) was removed from the abscess. To maintain ongoing cyst drainage into the vaginal cavity, the edges of the incision were sutured using 2-0 Vicryl (Ethicon, Raritan, NJ, United States), effectively forming a small pouch. Oral amoxicillin (500 mg every 8 h) and naproxen (250 mg thrice daily) were prescribed for 1 wk.
The patient was followed up for 1 wk postoperatively. The Bartholin’s cyst regressed, and the surgical wound healed well (Figure 2D).
In our case, a large Bartholin’s cyst occupied the right hemivulvar region and was accompanied by tenderness and purulent discharge. We initially suggested intravenous antibiotic therapy. However, the patient decided to undergo marsupialization. Postoperative oral antibiotics were administered. At the 1-wk follow-up, the vulvar region had a normal appearance upon examination. Initial marsupialization and subsequent antibiotic therapy for large Bartholin’s cysts can be an appropriate treatment for this type of case.
Benign vulvar masses are frequently observed in adult women[9,10]. Among these, glandular cysts are the most common[11]. Bartholin's gland lesions, such as cysts and abscesses, are the most prevalent and the primary representations of such lesions. Notably, abscesses occur at a rate three times higher than that of cysts[12].
The Bartholin's glands are small, pea-sized glands located on either side of the vaginal opening, and they are responsible for secreting fluid to lubricate the vaginal area. When the ducts of these glands become blocked or obstructed, a cyst can form[4]. Some common causes and factors that may contribute to developing a Bartholin's cyst include duct obstruction, infection, trauma or injury, hormonal change, foreign bodies, chronic inflammation, and idiopathic causes[13]. In our case, no apparent inflammation existed, as indicated by a normal white blood cell count. Nevertheless, pus was discovered within the Bartholin’s cyst, although it had not progressed to systemic inflammation. Incomplete patient-provided information, such as any potential trauma or injury associated with sexual activity, makes it difficult to speculate the cause of this illness. However, we believe that the cyst's substantial size may have originated from an initial duct obstruction, followed by pus formation, possibly in an environment conducive to developing a large cyst within the duct. In this case, the etiology may include idiopathic factors.
The initial approach involves performing an incision and drainage procedure and placing a Word catheter[6]. This procedure provides immediate pain relief by draining the accumulated pus. The Word catheter is typically left in place for 4–6 wk to facilitate epithelization. Alternatively, Jacobi rings can also be utilized for drainage and re-epithelization of the cysts. In a randomized study comparing the treatment of Bartholin cysts using Jacobi rings and Word catheters, similar outcomes were observed, although patients reported greater satisfaction with the rings. However, in the same study, 4%–17% of cases experienced recurrence when the catheter was left in place, and premature dislodgment of the catheter before epithelialization of the tract was common[14]. This treatment approach may not be advisable for deep cysts and abscesses[14]. Antibiotics are not routinely administered because cultures from Bartholin's cysts are sterile in > 80% of all cases, and approximately 33% of cultures from Bartholin's abscesses also show no bacterial growth[12].
Another commonly employed method for treating Bartholin gland cysts involves marsupialization, which entails making a small incision, typically 1.5–3 cm, directly over the cyst, allowing for the drainage of accumulated secretions[4]. In a randomized prospective study (2009) involving 83 women who underwent marsupialization, the most frequently reported postoperative symptoms included discharge at the surgical site and swelling of the labia[15]. Additionally, 24.1% of patients experienced recurrence; scar formation occurred in 68.7% of cases[16].
Other therapies, including alcohol sclerotherapy, silver nitrate sclerotherapy, and incision and drainage, can also be used[15].
In a randomized prospective study (2009) that compared marsupialization with the application of silver nitrate in treating Bartholin’s cysts and abscesses, both methods appeared to be equally effective[15]. However, using silver nitrate resulted in complete healing with less scar formation.
In a 2012 study that explored the management of Bartholin’s cysts using CO2 laser vaporization, out of 127 patients, only 86.6% were cured after a single laser treatment. The cyst sizes in this study ranged from 1.5–5.0 cm[17]. Managing larger cysts with CO2 laser ablation has not been extensively discussed in the literature.
In a systematic review conducted in 2020, the authors concluded that all available treatments for Bartholin's cysts were associated with lower recurrence rates, faster healing, and minimal adverse events[2]. However, the optimal treatment approach for larger cysts has not been definitively identified in the existing literature.
Nevertheless, the treatment of huge Bartholin’s cysts is not well understood. We reviewed case reports, and only five patients with giant Bartholin’s cysts were reported (Table 1). Four cases underwent total Bartholin’s cyst excision, and one underwent marsupialization. Kozawa et al[18] (2008), Kallam et al[12] (2017), and Karaman et al[9] (2015) suggested that excision is the best way to treat large Bartholin’s cysts. Moreover, in another report, Noval et al[7] (2019) also suggested cyst removal. Lilungulu et al[5] (2017) suggested that marsupialization is an effective method for treating large Bartholin cysts. All patients in the previous reports received broad-spectrum antibiotics after surgery, and no recurrence was noted. Regarding the treatment time for a large Bartholin cyst, most case reports recommended to commence promptly. Only one case report[5] prescribed 1 wk of antibiotics before marsupialization. In our case, marsupialization was performed immediately, followed by 1 wk of oral antibiotics.
| Ref. | Size | Treatment | Pathology |
| Kozawa et al[18], 2008 | 10 cm × 9 cm | Cyst excision | Bartholin cyst |
| Díaz de la Noval et al[7], 2019 | 10 cm × 8 cm | Cyst excision | Dermoid cyst |
| Kallam et al[12], 2017 | 10 cm × 7 cm | Cyst excision | Infected Bartholin cyst with hemorrhage |
| 23 cm × 11 cm, 6 cm × 6 cm | Cyst excision | Dermoid cyst | |
| Karaman et al[9], 2015 | 11 cm × 8 cm × 10 cm | Cystectomy | Epidermoid cyst |
| Lilungulu et al[5], 2017 | 10 cm | Antibiotic treatment for 1 wk, then Marsupialization | None |
| This study, 2023 | 10 cm | Marsupialization | None |
A limitation of our report is that the findings of this single case may not be universally applicable to all other patients. Gathering data from a more extensive case series in the future may be beneficial.
While Bartholin's cyst abscesses typically present as a vulval mass, those involving a giant cyst, as seen in our case, are exceptionally rare. The approach to managing these cases may differ from standard presentations depending on the discomfort level experienced by the patient and the size and extent of the mass. A diagnosis can often be made through a physical examination. Surgical management involving marsupialization with antibiotic prophylaxis remains the definitive treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emran TB, Bangladesh S-Editor: Lin C L-Editor: Filipodia P-Editor: Lin C
| 1. | Speck NM, Boechat KP, Santos GM, Ribalta JC. Treatment of Bartholin gland cyst with CO2laser. Einstein (Sao Paulo). 2016;14:25-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Illingworth B, Stocking K, Showell M, Kirk E, Duffy J. Evaluation of treatments for Bartholin's cyst or abscess: a systematic review. BJOG. 2020;127:671-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 3. | Aldrich ER, Pauls RN. Benign Cysts of the Vulva and Vagina: A Comprehensive Review for the Gynecologic Surgeon. Obstet Gynecol Surv. 2021;76:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 4. | Lee MY, Dalpiaz A, Schwamb R, Miao Y, Waltzer W, Khan A. Clinical Pathology of Bartholin's Glands: A Review of the Literature. Curr Urol. 2015;8:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Lilungulu A, Mpondo BCT, Mlwati A, Matovelo D, Kihunrwa A, Gumodoka B. Recurrent Huge Left Bartholin's Gland Abscess for One Year in a Teenager. Case Rep Infect Dis. 2017;2017:9151868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Karabük E, Ganime Aygün E. Marsupialization vs Word catheter in the treatment of Bartholin cyst or abscess: retrospective cohort study. J Turk Ger Gynecol Assoc. 2022;23:71-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Díaz de la Noval B, García Fernández I, Álvarez Fernández B. Bulky Bartholin's gland cyst: Case report of an incidental finding. Case Rep Womens Health. 2019;22:e00115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Bringas LAH, Billod JA. Gigantic vulvar masses: a case series of benign large vulvar tumors. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2021;10:2476-82. |
| 9. | Karaman E, Çim N, Akdemir Z, Elçi E, Akdeniz H. Giant vulvar epidermoid cyst in an adolescent girl. Case Rep Obstet Gynecol. 2015;2015:942190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kessous R, Aricha-Tamir B, Sheizaf B, Shteiner N, Moran-Gilad J, Weintraub AY. Clinical and microbiological characteristics of Bartholin gland abscesses. Obstet Gynecol. 2013;122:794-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Eilber KS, Raz S. Benign cystic lesions of the vagina: a literature review. J Urol. 2003;170:717-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Kallam AR, Kanumury V, Bhimavarapu N, Soorada B. A Report of Two Cases of "Giant Bartholin Gland Cysts" Successfully Treated by Excision with Review of Literature. J Clin Diagn Res. 2017;11:PD11-PD13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Mayeaux EJ Jr, Cooper D. Vulvar procedures: biopsy, bartholin abscess treatment, and condyloma treatment. Obstet Gynecol Clin North Am. 2013;40:759-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Bati-Paracha A, Sharma M. Management of Bartholin’s cyst and abscess. Obstet Gynaecol. 2023;25:72-77. |
| 15. | Ozdegirmenci O, Kayikcioglu F, Haberal A. Prospective Randomized Study of Marsupialization versus Silver Nitrate Application in the Management of Bartholin Gland Cysts and Abscesses. J Minim Invasive Gynecol. 2009;16:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Shariff FO, Septian D, Fajarwati DD, Siagian ET, Lasmawati E, Aprillya E, Hanifa F, Lawren J. Recurrent Bartholin’s Cyst: Literature Review and Case Report. Muhammadiyah Medical Journal. 2022;3:19-26. |
| 17. | Figueiredo AC, Duarte PE, Gomes TP, Borrego JM, Marques CA. Bartholin's gland cysts: management with carbon-dioxide laser vaporization. Rev Bras Ginecol Obstet. 2012;34:550-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Kozawa E, Irisawa M, Heshiki A, Kimura F, Shimizu Y. MR findings of a giant Bartholin's duct cyst. Magn Reson Med Sci. 2008;7:101-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |