Published online Nov 6, 2023. doi: 10.12998/wjcc.v11.i31.7699
Peer-review started: September 3, 2023
First decision: September 28, 2023
Revised: October 19, 2023
Accepted: October 27, 2023
Article in press: October 27, 2023
Published online: November 6, 2023
Processing time: 64 Days and 2 Hours
Meralgia paresthetica (MP) is an entrapment mononeuropathy of the lateral femoral cutaneous nerve (LFCN). Although structural abnormalities in nerve tissues can be confirmed using ultrasonography, this is not routinely performed.
Herein, we present the case of a 52-year-old woman who developed MP after laparoscopic gynecological surgery. The patient was referred to our clinic from an obstetrics and gynecology clinic with symptoms of numbness and a tingling sen
This case demonstrates the value of ultrasonography in detecting anatomical variation and diagnosing persistent MP. Ultrasonography should be considered an adjunct to electromyography for optimal MP management. Further, this case would help other clinicians determine patient prognosis and decide on targeted treatment strategies.
Core Tip: We describe a woman who developed meralgia paresthetica (MP) after laparoscopic gynecological surgery in the lithotomy position. The patient had an anatomical variation of the lateral femoral cutaneous nerve, entrapped within the inguinal ligament and detected by ultrasonography. The case suggests ultrasonography can help prevent and treat MP by identifying anatomical variations and nerve status before and after surgery.
- Citation: Park HW, Ji KS, Kim JH, Kim LN, Ha KW. Ultrasonographic identification of lateral femoral cutaneous nerve anatomical variation in persistent meralgia paresthetica: A case report. World J Clin Cases 2023; 11(31): 7699-7705
- URL: https://www.wjgnet.com/2307-8960/full/v11/i31/7699.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i31.7699
Meralgia paresthetica (MP) is defined by sensations of burning, tingling, numbness, and pain along the course of the lateral femoral cutaneous nerve (LFCN)[1-3]. MP pathogenesis remains poorly understood; however, its etiology and risk factors are under investigation. MP has been associated with several etiological factors, including iatrogenic injury, medical conditions, and operative/postoperative complications[1-3]. Furthermore, the association between MP and surgical procedures performed in the lithotomy position (LP) has been reported[4-6]. The LFCN has several anatomical variations that may affect MP incidence and prognosis[2,3,7-10]. For example, the main compression section is located around the anterior superior iliac spine (ASIS), and the location of the LFCN may negatively impact prognosis. Ultrasonography is a quick and easy method to verify the condition of muscles, ligaments, and nerves; however, it is not commonly used to evaluate the LFCN. Herein, we report the case of a woman with persistent MP, whose LFCN anatomical variation was discovered via ultrasonographic examination. This case implies that performing ultrasonography pre- and post-operation in the LP may help prevent MP. Moreover, the insights gained from this case can aid other clinicians in predicting patient outcomes and selecting suitable treatment approaches.
A 52-year-old woman (height; 151 cm, weight; 52 kg) was referred to our clinic from an obstetrics and gynecology clinic with symptoms of numbness and tingling sensation in the left anterolateral thigh following a laparoscopic myomectomy 5 mo prior.
The patient had undergone surgery in the LP, during which her legs were fixed using the instrument shown in Figure 1, with hip flexion of 45°, knee flexion of 45°, and thighs apart by 90°. During the surgery, while handling the endoscopic surgical instrument, the patient was repeatedly repositioned so that the left hip joint extended parallel to the operating table to secure space for the surgeon (Figure 1). Laparoscopic adenomyomectomy and myomectomy were performed following adhesiolysis. The operation lasted 75 min. The patient complained of decreased sensation in her left outer thigh the day after the surgery, and her symptoms gradually worsened after 5 mo. In addition, the tingling sensation in that area began 2 wk before the visit.
The patient had no relevant medical history or history of issues in this region. The patient had a surgical history of left ovarian mass removal 17 years prior, appendectomy 15 years prior, and right ectopic pregnancy surgery 10 years prior; however, she had experienced no side effects after the previous surgeries.
The patient had no relevant family history or history of issues in this region.
Physical examination revealed no signs of trauma. Neurological examination showed that the strength of all lower extremity muscles was intact. Numbness and tingling sensations in the left anterolateral thigh were the only symptoms. A positive Tinel’s sign was observed on the medial side of the left ASIS.
Needle electromyography (EMG) and nerve conduction studies (NCS) were performed in the bilateral lower extremities. The sensory response of the right LFCN was within the normal limits; however, that of the left LFCN showed no response. All other motor and sensory responses were within the normal limits (Table 1). Needle EMG showed normal motor unit potentials in all examined muscles.
| Nerve | Stimulation | Latency (ms) | Amplitude (μV) | NCV (m/s) |
| Motor | Onset latency | |||
| Lt. Common peroneal | Ankle | 3.05 | 7.2 | |
| Fib head | 7.45 | 6.9 | 56.8 | |
| Knee | 8.35 | 6.8 | 55.6 | |
| Lt. Tibial | Ankle | 3.35 | 23.0 | |
| Fib head | 8.55 | 18.3 | 55.8 | |
| Sensory | Peak latency | |||
| Lt. Sural | 2.90 | 21.5 | ||
| Rt. LFCN | 2.90 | 6.5 | ||
| Lt. LFCN | NR |
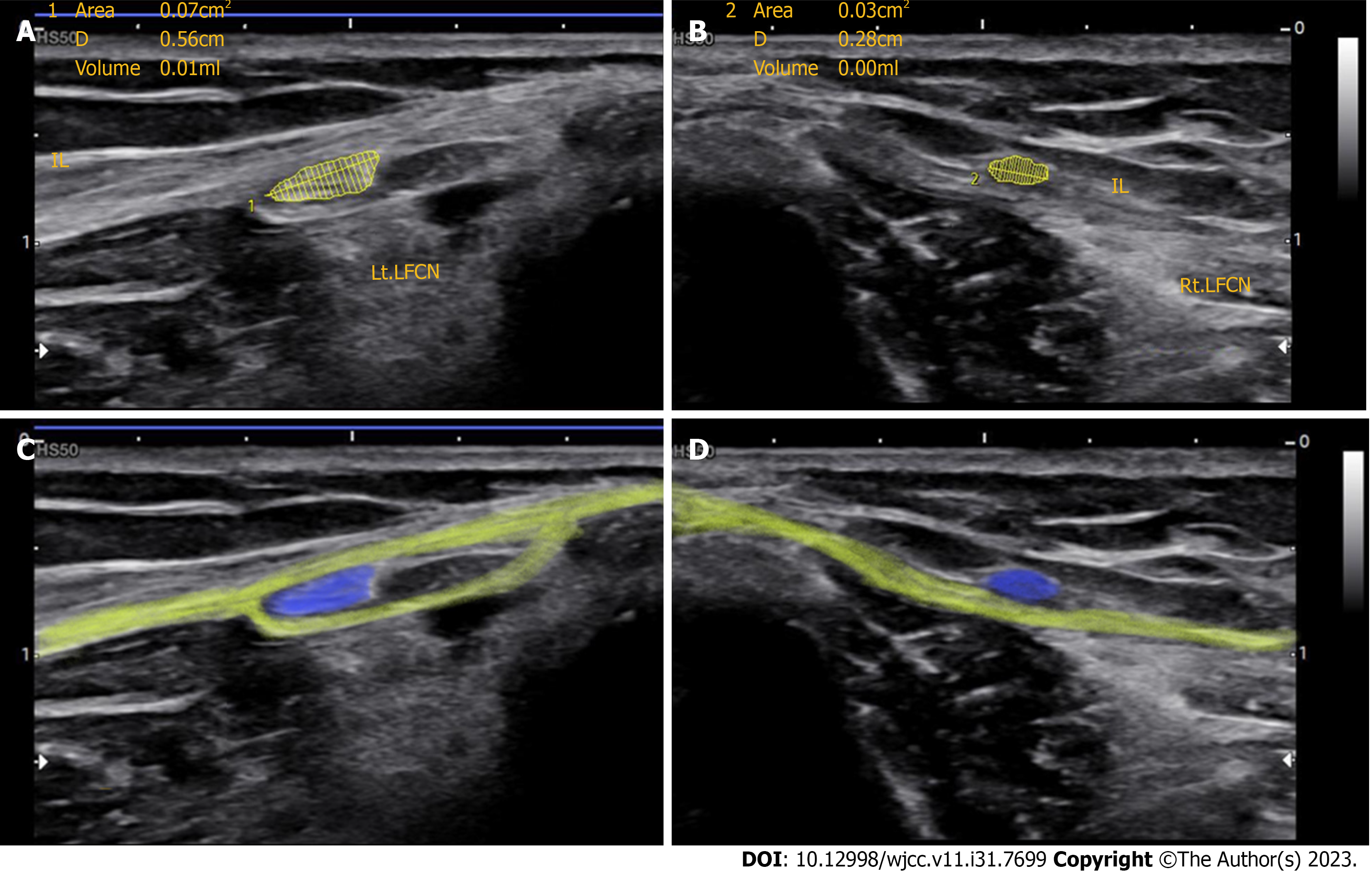
We subsequently performed ultrasonography to confirm the condition of the bilateral LFCN. The cross-sectional area (CSA) of the left LFCN was 7 mm2, and the longitudinal diameter (LD) was 5.6 mm. The CSA of the right side was 3 mm2, and the LD was 2.8 mm (Figure 2). According to a previous study, the normal ranges for the CSA and LD of the LFCN are 4.5 ± 1.0 mm2 and 3.5 ± 0.3 mm, respectively[11]. Unlike the right LFCN of the patient, which passed over the inguinal ligament (IL), the left LFCN was entrapped within the IL and became swollen around it (Figure 2).
Combined with the patient' surgical history, EMG results, and ultrasonography result, the final diagnosis was persistent MP due to anatomical variation of the LFCN.
We warned the patient that tight pants may interrupt recovery and recommended that she wear loose clothes until the next visit. We further prescribed gabapentin (300 mg/d) for a week to relieve her symptoms.
Twenty weeks later, we performed NCS and ultrasonography in the bilateral LFCN. The amplitude of sensory nerve action potential of the left LFCN was 3.7 mV on NCS, showing improvement compared to earlier tests. The left LFCN CSA was 5 mm2 on follow-up ultrasonography, indicating that it had decreased from its abnormally enlarged state and had normalized[11].
MP is an entrapment mononeuropathy of the LFCN[1,2,5,12]. Although MP is well-known to physical medicine and rehabilitation experts, its diagnosis remains obscure, and few physicians from other fields know it. The most common symptoms are pain, paresthesia, and sensory loss in the anterolateral aspect of the thigh[1,2,5,12]. The primary cause of MP remains unknown, although its occurrence is associated with several etiological factors. Various causes of MP have been reported, including direct trauma; tight clothing; abdominal, spinal, and pelvic surgeries; abdominal and pelvic tumors; obesity; pregnancy; diabetic polyneuropathy; and idiopathic causes[1,2,5,12].
Undergoing surgery in the LP is a rare cause of MP. In a previous prospective study, 4 of 991 patients who underwent surgery in the LP developed MP[7]; however, only a few reports of an association between MP and LP exist[5-7,13]. Nevertheless, as hip flexion and abduction are performed simultaneously in the LP, the LFCN could become compressed and angulated by soft tissue. In particular, LFCN stretching or irritation may occur in patients undergoing laparoscopic surgery alternating between two positions (Figure 1). Because we did not identify any other factor that could have caused MP in this patient, it is reasonable to consider LP as the primary cause.
It is important to recognize anatomic variations in the LFCN during MP diagnosis and treatment[2,8,10,11,14,15]. The course of the LFCN is highly variable, with numerous anatomical studies reporting these variations[2,3,8,14-19]. Several studies have investigated the location of the LFCN in relation to the ASIS and iliac crest[10,14-19]. Kosiyatrakul et al[15] examined 96 cadaveric specimens and divided LFCN variation into three types according to the relationship with the ASIS and iliac crest. Mutara et al[18] classified the variation of the LFCN into four types based on the relationship with the ASIS and IL in a 205 nerve sample. Mischkowski et al[19] investigated 34 cadaveric specimens and categorized LFCN variation into five types depending on the relationship with the ASIS. However, none of these studies mentioned LFCN variations as the nerve passes through the IL[15,18,19]. Aszmann et al[10] examined 52 specimens and categorized LFCN variation into five types according to the site through which the LFCN exits the abdomen, as shown in Figure 3. According to their research, in 27% of cases, the LFCN was surrounded by the IL[10]. In this case, the LFCN of the patient had been entrapped in the IL, suggesting that the anatomical LFCN course may correspond to type B. The aforementioned study suggested that types A, B, and C likely involved damage during surgery[10].
In a cadaveric study, Deveneau et al[20] observed stretching of the femoral nerve in the LP. All examined femoral nerves exhibited some degree of stretching in the LP, with the hip extending below the bed level between 10° and 20°, and the knee flexing at approximately 90°. Furthermore, the femoral nerve moved under the IL during repositioning.
In the present case, the affected LFCN passed along the IL, similar to the femoral nerve. However, as the LFCN is thinner and weaker than the femoral nerve, it is more likely to be stretched in the LP or be irritated when caught between the IL during repeated repositioning. According to a meta-analysis study by Tomaszewski et al[3], 3.7% of LFCNs pass through the IL, as in the current case. The authors suggested that identifying anatomical variations using preoperative ultrasonography would help prevent postoperative MP[3]. In our case, the patient was instructed to wear loose clothes and prescribed gabapentin after an EMG examination. Her symptoms improved partially and significantly at the 2 and 5-mo follow-ups, respectively.
Ultrasonography has shown its usefulness in assessing peripheral nerve disease for diagnosis, prognosis, treatment, and rehabilitation decisions[21,22]. Ultrasonography has the advantage of showing the course and morphological changes of the LFCN and can guide nerve blocks. Additionally, a nerve with an anatomical variation can be visualized via ultrasonography[23,24]. This report differs from previous studies, as ultrasonography was performed in addition to EMG to check the nerve status of the patient and determine any anatomical variation, as her symptoms showed no natural improvements. Although previous large-scale studies have investigated neuropathies in the lower extremities that occurred after gynecological surgery, most patients underwent open surgery, and no studies have used methods other than EMG[6,7,13]. Furthermore, Chen and Kowalski[6] described patients with persistent symptoms that lasted more than 3 mo and differed from general clinical features, but the disease cause could not be identified. The unique feature of this report is that it indicates that by assessing the cause of MP by performing ultrasonography on a patient with persistent symptoms, which differed from those in general clinical patterns. Although several studies have evaluated LFCN in patients with MP using ultrasonography, none has suggested the cause of MP with persistent symptoms[9,11,25]. Because this study is based on a single patient, generalizing the findings is challenging; however, the study introduces the possibility of anatomical variations causing persistent MP. The variations can be identified through ultrasound examinations. If this information is utilized effectively in clinical practice, it could expedite and enhance the accuracy of treatments for patients with MP experiencing persistent symptoms. We anticipate that future large-scale studies could provide a more precise understanding of this association, enhancing patient care.
This case report highlights the importance of considering anatomical variations and the use of ultrasonography in diagnosing and treating persistent MP. Our findings suggest that ultrasonography can be a valuable tool in identifying anatomical variations that may contribute to MP development, particularly in cases where symptoms persist despite conservative treatment. In conclusion, this case report emphasizes the need for clinicians to consider the potential for MP occurrence in patients undergoing surgery in the LP. Furthermore, we propose the use of ultrasonography in addition to EMG to ensure more targeted treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ewers A, Austria; Valderrama-Canales FJ, Spain S-Editor: Qu XL L-Editor: A P-Editor: Xu ZH
| 1. | Solomons JNT, Sagir A, Yazdi C. Meralgia Paresthetica. Curr Pain Headache Rep. 2022;26:525-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Kesserwani H. Meralgia Paresthetica: A Case Report With an Update on Anatomy, Pathology, and Therapy. Cureus. 2021;13:e13937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Tomaszewski KA, Popieluszko P, Henry BM, Roy J, Sanna B, Kijek MR, Walocha JA. The surgical anatomy of the lateral femoral cutaneous nerve in the inguinal region: a meta-analysis. Hernia. 2016;20:649-657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Peters G, Larner AJ. Meralgia paresthetica following gynecologic and obstetric surgery. Int J Gynaecol Obstet. 2006;95:42-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Brandt L, Albert S, Brandt KL. [Meralgia paraesthetica as complication of patient positioning : A not fully controllable risk]. Anaesthesiologie. 2022;71:858-864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Chen E, Kowalski JT. Natural history of postoperative neuropathies in gynecologic surgery. Int Urogynecol J. 2022;33:2471-2474. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Warner MA, Warner DO, Harper CM, Schroeder DR, Maxson PM. Lower extremity neuropathies associated with lithotomy positions. Anesthesiology. 2000;93:938-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Mandal P, Russe E, Schwaiger K, Wechselberger G, Feigl G. Anatomical Analysis of the Lateral Femoral Cutaneous Nerve and Its Passage beneath the Inguinal Ligament. Plast Reconstr Surg. 2022;149:1147-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Becciolini M, Pivec C, Riegler G. Ultrasound of the Lateral Femoral Cutaneous Nerve: A Review of the Literature and Pictorial Essay. J Ultrasound Med. 2022;41:1273-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100:600-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 152] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Lee JS, Kwon E, Kim DH, Hwang M. Ultrasonographic findings of the lateral femoral cutaneous nerve in normal adult women. J Korean Assoc EMG Electrodiagn Med. 2008;10:130-134. [DOI] [Full Text] |
| 12. | Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8:883-893. [PubMed] |
| 13. | Seo MJ, Han GA, Jung JW, Lee SJ, Choi WJ, Lee SA, Lee JH, Baek WY. Clinical findings in patients with femoral cutaneous sensory change after gynecologic operation. Korean J Obstet Gynecol. 2000;43:2008-2013. |
| 14. | Kokubo R, Kim K, Morimoto D, Isu T, Iwamoto N, Kitamura T, Morita A. Anatomic Variation in Patient with Lateral Femoral Cutaneous Nerve Entrapment Neuropathy. World Neurosurg. 2018;115:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Kosiyatrakul A, Nuansalee N, Luenam S, Koonchornboon T, Prachaporn S. The anatomical variation of the lateral femoral cutaneous nerve in relation to the anterior superior iliac spine and the iliac crest. Musculoskelet Surg. 2010;94:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Moritz T, Prosch H, Berzaczy D, Happak W, Lieba-Samal D, Bernathova M, Auff E, Bodner G. Common anatomical variation in patients with idiopathic meralgia paresthetica: a high resolution ultrasound case-control study. Pain Physician. 2013;16:E287-E293. [PubMed] |
| 17. | Carai A, Fenu G, Sechi E, Crotti FM, Montella A. Anatomical variability of the lateral femoral cutaneous nerve: findings from a surgical series. Clin Anat. 2009;22:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000;82:746-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Mischkowski RA, Selbach I, Neugebauer J, Koebke J, Zöller JE. Lateral femoral cutaneous nerve and iliac crest bone grafts--anatomical and clinical considerations. Int J Oral Maxillofac Surg. 2006;35:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Deveneau NE, Forbis C, Lipetskaia L, Kinman CL, Agrawal A, Herring NR, Francis SL. The Effect of Lithotomy Position on Nerve Stretch: A Cadaveric Study. Female Pelvic Med Reconstr Surg. 2017;23:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Coraci D, Tsukamoto H, Granata G, Briani C, Santilli V, Padua L. Fibular nerve damage in knee dislocation: Spectrum of ultrasound patterns. Muscle Nerve. 2015;51:859-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Padua L, Paolasso I, Pazzaglia C, Granata G, Lucchetta M, Erra C, Coraci D, De Franco P, Briani C. High ultrasound variability in chronic immune-mediated neuropathies. Review of the literature and personal observations. Rev Neurol (Paris). 2013;169:984-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Damarey B, Demondion X, Boutry N, Kim HJ, Wavreille G, Cotten A. Sonographic assessment of the lateral femoral cutaneous nerve. J Clin Ultrasound. 2009;37:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Hurdle MF, Weingarten TN, Crisostomo RA, Psimos C, Smith J. Ultrasound-guided blockade of the lateral femoral cutaneous nerve: technical description and review of 10 cases. Arch Phys Med Rehabil. 2007;88:1362-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Chang KV, Mezian K, Naňka O, Wu WT, Lou YM, Wang JC, Martinoli C, Özçakar L. Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. J Clin Med. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 96] [Article Influence: 13.7] [Reference Citation Analysis (0)] |