Published online Nov 6, 2023. doi: 10.12998/wjcc.v11.i31.7684
Peer-review started: August 29, 2023
First decision: October 10, 2023
Revised: October 14, 2023
Accepted: October 27, 2023
Article in press: October 27, 2023
Published online: November 6, 2023
Processing time: 68 Days and 22.9 Hours
Forehead osteoma is a commonly encountered benign facial bone tumor. Endoscopic excision of benign forehead masses is widely performed. Here, we report a rare case of recurrent forehead osteoma that disseminated after a previous osteoma excision.
A 54-year-old female patient had previously undergone endoscopic removal of a single forehead osteoma at 30 years of age. However, she had a recurrent osteoma around the same site and underwent another endoscopic resection at 40 years of age. During her first visit to our outpatient clinic, she presented with a cobble
To prevent recurrence, it is essential to conduct additional meticulous burring and a thorough inspection of the surface after copious irrigation.
Core Tip: This case showed that remnant particles of resected osteoma tend to be neglected in the endoscopic approach, and these particles may induce recurrence due to inoculation, even having devastating results of widely disseminated growth of osteoma. Thorough observation of the bony surface, sufficient burring, and copious irrigation for complete removal of the bony segments after ostectomy are essential to prevent recurrence and related complications.
- Citation: Lee DY, Lim S, Yoon JS, Eo S. Recurred forehead osteoma disseminated after previous osteoma excision: A case report. World J Clin Cases 2023; 11(31): 7684-7689
- URL: https://www.wjgnet.com/2307-8960/full/v11/i31/7684.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i31.7684
Craniofacial osteoma is a benign, slow-growing, osteogenic lesion characterized by the proliferation of cortical or cancellous bone. Trauma, inflammation, developmental disorders, and genetic defects are considered causative factors[1-3]. Craniofacial osteomas can arise from the periosteum or endosteum and are commonly found in the skull, paranasal sinuses, maxilla, and mandible[2]. However, a detailed analysis of their incidence and morphology has not yet been systematically established[1,2].
Most cases of frontal bone osteoma are identified as solitary lesions on the forehead, and patients usually complain of changes in facial morphology. Although resection of the osteoma is possible after a direct skin incision on the mass, there is a growing preference for endoscopic resection to reduce the risk of scar formation[4-8]. However, a bicoronal incision could also be performed in cases of large size or specific locations, such as the glabella and temple region[9,10]. In this report, we present a rare case of recurrent forehead osteoma disseminated from the previous endoscopic resection site of a solitary forehead osteoma. To the best of our knowledge, this case has not previously been reported in the literature.
A 54-year-old female patient visited our clinic with a wide, cobblestone-shaped, disseminated firm mass on her forehead that was palpated 10 years after her last surgery.
She had previously undergone endoscopic removal of a small single forehead osteoma at a military hospital during military service at 30 years of age. She palpated a recurrent, larger cobblestone-like surface area on her forehead and underwent endoscopic resection at another local medical center at the age of 40. However, 9 years later, she developed an irregular uneven surface on her forehead with gradual growth of small, hard masses.
The patient denied any previous history of trauma or aesthetic procedures.
The patient had no family history of similar findings or other medical complications.
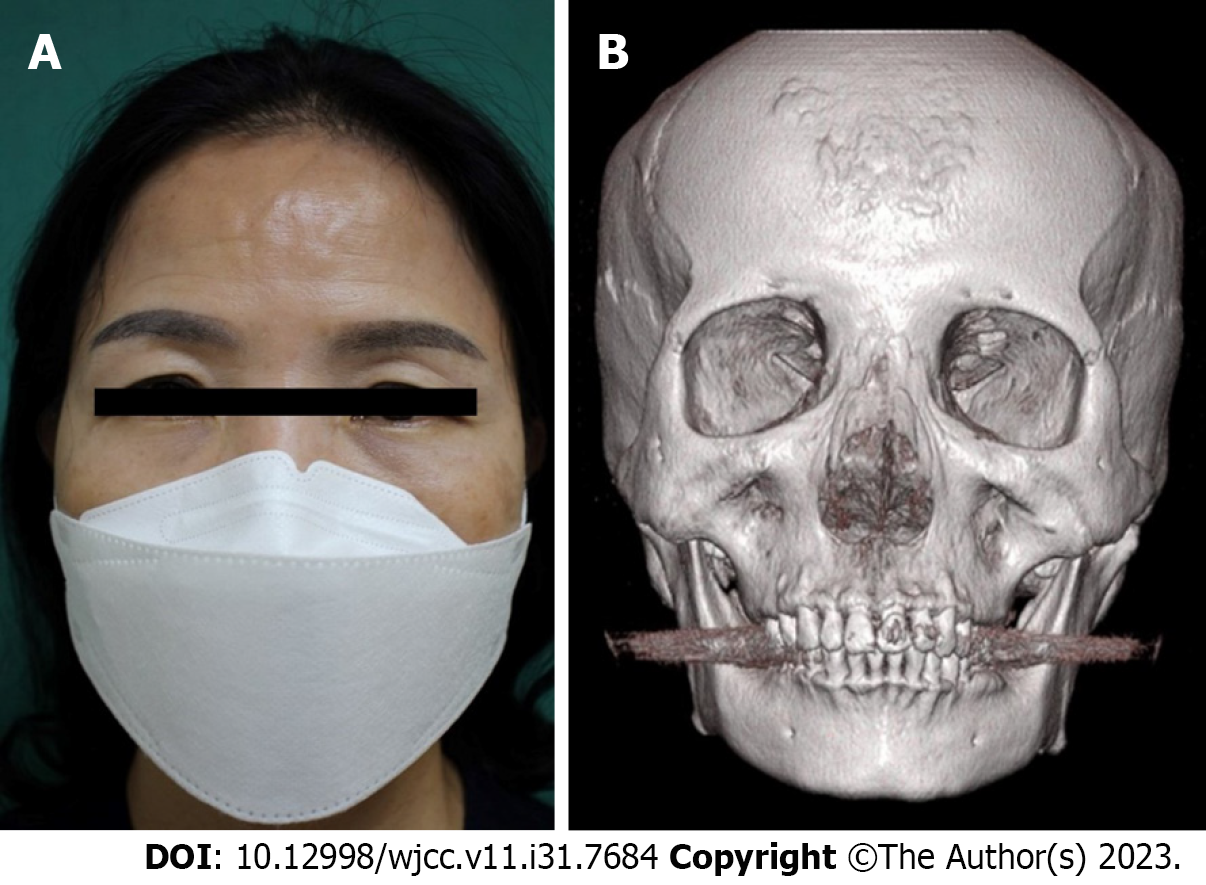
The surface of her forehead was palpated and revealed a hard-bone-like tumor. The firm and ragged surface of the forehead was palpable on physical examination, without any skin lesions (Figure 1A).
Laboratory investigations revealed normal white blood cell count (5080 cells/μL), hemoglobin (12.9 g/dL), platelet count (202000 cells/μL), and C-reactive protein level (< 0.06 mg/L). No signs of an acute infection were observed.
Preoperative computed tomography with 3-D reconstruction of the facial bone revealed widespread osteoma dissemination on the outer table of the frontal bone (Figure 1B).
The patient was diagnosed with widespread osteoma inoculation on the outer table of the frontal bone.
Under general anesthesia, we performed a modified bicoronal approach without invading the sideburns, with an incision line 1.5 cm behind the anterior hairline. The periosteum was dissected using a monopolar Bovie device and the periosteal layer was elevated using a Freer elevator. Upon exposure of the skull vault lesion on the forehead, the palpated surface was identified as a widely inoculated osteoma located on the outer table of the frontal bone (Figure 2A). A sessile lesion measuring a total of 5.2 cm × 4.1 cm in size with an irregular margin was noted. Relatively large protruding bone lesions were removed by partial ostectomy using an osteotome and chisel (Figure 2B). The excised frontal bone was meticulously resurfaced using an electrical bur and surgical rasps. After thorough irrigation to completely remove any remaining particles, bone wax was applied to the bone surface for bleeding control and optimal aesthetic appearance (Figure 2C). The periosteum was repaired with simple interrupted sutures using 4-0 Vicryl, and layer-by-layer wound closure was performed with simple interrupted sutures using 5-0 blue nylon, taking care not to tighten the hair follicles (Figure 2D).
Pathological examination of the resected specimen revealed a benign osteoma of the compact bone without cancellous tissue (Figure 3). At the 1-year postoperative follow-up visit in the outpatient clinic, the smooth contour of the forehead was confirmed by gross observation and palpation (Figure 4). The patient was satisfied with the surgical outcome, which included no recurrence or complications during the 2-year follow-up period.
Osteoma is a rare benign tumor characterized by gradual proliferation, with a general prevalence of approximately 0.01%-0.43% of the total population[1]. Patients most frequently present with a bony lesion in the third and fourth decades of life, and men are affected more frequently[2]. Genetic mutations, developmental abnormalities, trauma, chronic inflammation, and hormonal imbalances have all been proposed as potential contributors to osteoma formation. However, the exact mechanism and specific causative factors remain unclear[1,2].
Craniofacial osteomas are mostly seen in the frontal sinus and occur in the order of the ethmoid, maxillary, and sphenoid sinus[1-3]. Most frontal osteomas are solitary rather than multiple occurrences[2]. The tumor is often slow-growing and asymptomatic and is diagnosed incidentally on radiographs. Later, it can achieve a faster growth rate as the rate of osteogenesis increases and can cause deformation of the bone, morphological abnormalities of the forehead, and compression of the adjacent structures. They usually appear as unilateral, sessile, or pedunculated, well-circumscribed, mushroomlike masses, ranging from 1.5 to 40 mm in diameter[2]. Osteomas are distinguished as compact, cancellous, and mixed types according to histopathologic findings[1-3]. The compact type is comprised of solid bone, such as the Harversian system, with partial inclusion of fibrotic tissue. The cancellous type consists of trabecular bone structure and bone marrow and is often identified in the maxilla, ethmoid sinus, and marginal lesions of the compact bone[2]. In accordance with these classifications, our case was the periosteal type of the skull vault osteoma with the compact bone on histology. Moreover, the attachment was sessile with a wide base.
Other than the recurrence of solitary bone tumors, widely disseminated multiple osteomas on the frontal bone are extremely rare and can arise from specific syndromes with clinically significant genetic factors or unknown etiology[11-13]. Rare cases of four to five distinctive frontal osteomas in one patient have been previously reported[14]. Multiple intracranial osteomas have been reported as forms of multifocal cavernous hemangiomas, or subarachnoid osteomas[15-17]. Multiple osteomas of compact bone in the skull vault have only been reported as an accompanying symptom of Gardener’s syndrome, principally on the mandible and frontal bones. Gardener’s syndrome is an autosomal dominant form of polyposis characterized by the presence of asymptomatic multiple polyps in the colon together with extra-colonic tumors[11]. Our patient was confirmed to have no specific findings on esophagogastroduodenoscopy and colonoscopy had been performed during a regular checkup a year prior. There have been no reports of non-syndromic disseminated multiple osteomas without other gastrointestinal lesions[11-17], and our case is noteworthy in that the widely inoculated osteoma was unrelated to Gardener’s syndrome and had an indistinct morphological demarcation.
A differential diagnosis is required for a firmly palpated forehead mass. Because distinguishing between a forehead osteoma and a deeply located retromuscular lipoma can be challenging through palpation alone, a computed tomo
Resection of the osteoma is possible after a direct skin incision on the mass, which can visually expose the bony lesion and allow clear identification of the margin, resulting in transverse scars. Endoscopic resection techniques are increasingly preferred in recent years to reduce the risk of scar formation[4-9], but surgeons may have difficulty verifying the complete removal of the lesion and identifying the resected surface, with possibly longer operation times[4-7]. With the endoscopic approach, remnant particles of resected osteoma tend to be easily neglected, which may induce recurrence due to inoculation. This can result in devastating, widely disseminated growth of the osteoma around the surface of the frontal bone. In addition, a bicoronal incision is made in cases of large sizes or specific locations, such as the glabella and temple regions[9,10,14]. Our case is a rare phenomenon, suspected to be caused by the recurrence of remnant particles after incomplete ostectomy and dissemination.
Many cases of recurrent skull osteomas have been reported in the literature, especially after a non-radical surgery (curettage or partial resection) and radiofrequency treatment[14,18]. Owing to small patient cohorts and the variability of surgical techniques, the recurrence rate is unknown, although for radiofrequency treatment, the rate is thought to be approximately 7% overall, with higher rates in younger patients[18]. Several hypotheses may explain the recurrence. Endoscopy may have complicated visualization and complete resection of the lesion or may have caused unintentional seeding during the procedure[4-8,18]. Therefore, radical excision with a wide surgical field is the best treatment option for osteoma. After radical excision of the giant osteoma, skull defect reconstruction with an autologous bone graft or Medpor Titan plate for recontouring might be needed[10]. In our case, several shallow depressions after ostectomy and bone bleeding were covered with bone wax.
In conclusion, this case showed that the remnant particles of resected osteomas tend to be neglected in the endoscopic approach, and these particles may induce recurrence due to inoculation, even with devastating results of widely disseminated osteoma growth. Athorough observation of the bony surface, sufficient burring, and copious irrigation for the complete removal of the bony segments after ostectomy are essential to prevent recurrence and related complications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hashimoto K, Japan S-Editor: Qu XL L-Editor: A P-Editor: Zhao S
| 1. | Haddad FS, Haddad GF, Zaatari G. Cranial osteomas: their classification and management. Report on a giant osteoma and review of the literature. Surg Neurol. 1997;48:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Eshed V, Latimer B, Greenwald CM, Jellema LM, Rothschild BM, Wish-Baratz S, Hershkovitz I. Button osteoma: its etiology and pathophysiology. Am J Phys Anthropol. 2002;118:217-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Patel TR, Borah GL. Frontal bone periosteal osteomas. Plast Reconstr Surg. 2004;114:648-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Lai CH, Sun IF, Huang SH, Lai CS, Lin SD. Forehead osteoma excision by endoscopic approach. Ann Plast Surg. 2008;61:533-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Raponi I, Giovannetti F, Cacciatore F, Di Carlo D, Valentini V. Endoscopic Forehead Approach for Minimally Invasive Frontal Osteoma Excision. J Craniofac Surg. 2020;31:e767-e769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Lin SD, Lee SS, Chang KP, Lin TM, Lu DK, Tsai CC. Endoscopic excision of benign tumors in the forehead and brow. Ann Plast Surg. 2001;46:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Lopez M, Vermersch S, Varlet F. Endoscopic Excision of Forehead and Eyebrow Benign Tumors in Children. J Laparoendosc Adv Surg Tech A. 2016;26:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Steele MH, Suskind DL, Moses M, Kluka E, Liu DC. Orbitofacial masses in children: an endoscopic approach. Arch Otolaryngol Head Neck Surg. 2002;128:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Savić DL, Djerić DR. Indications for the surgical treatment of osteomas of the frontal and ethmoid sinuses. Clin Otolaryngol Allied Sci. 1990;15:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Chang SC, Chen PK, Chen YR, Chang CN. Treatment of frontal sinus osteoma using a craniofacial approach. Ann Plast Surg. 1997;38:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Ben Lagha N, Galeazzi JM, Chapireau D, Oxeda P, Bouhnik Y, Maman L. Surgical management of osteoma associated with a familial Gardner's syndrome. J Oral Maxillofac Surg. 2007;65:1234-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Sahoo MR, Nayak AK, Pattanaik A, Gowda MS. Gardner's syndrome, a rare combination in surgical practice. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | McNab AA. Orbital osteoma in Gardner's syndrome. Aust N Z J Ophthalmol. 1998;26:169-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Uemura T, Kawano H, Watanabe H, Kikuchi M. Multiple Peripheral Osteomas Related to Frontal Exposure by Bicoronal Incision. J Craniofac Surg. 2016;27:733-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Kuzeyli K, Usul H, Cakir E, Caylan R, Rei A, Baykal S, Peksoylu B, Yazar U, Arslan E. Multifocal intradiploic cavernous hemangioma of the skull associated with nasal osteoma. Acta Neurochir (Wien). 2003;145:323-6; discussion 326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Akiyama M, Tanaka T, Hasegawa Y, Chiba S, Abe T. Multiple intracranial subarachnoid osteomas. Acta Neurochir (Wien). 2005;147:1085-9; discussion 1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Kar A, Gaikwad M, Patnaik M. A Rare Occurrence of Multiple Intracranial Osteomas in the Cranial Cavity of a Cadaver With a Short Review on Subdural Osteoma. Cureus. 2021;13:e17737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Sampath SC, Sampath SC, Rosenthal DI. Serially recurrent osteoid osteoma. Skeletal Radiol. 2015;44:875-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |