Published online Nov 6, 2023. doi: 10.12998/wjcc.v11.i31.7635
Peer-review started: July 13, 2023
First decision: September 25, 2023
Revised: October 10, 2023
Accepted: October 23, 2023
Article in press: October 23, 2023
Published online: November 6, 2023
Processing time: 116 Days and 6.2 Hours
Superior vena cava (SVC) aneurysms are a relatively uncommon disease that has not been widely reported. The conventional surgical approach for treating SVC aneurysms includes open thoracotomy and mid-sternotomy. However, in this case, the aneurysm could be safely resected by thoracoscopic simultaneous lateral and subxiphoid access methods.
A 58-year-old male presented with intermittent chest pain and persistent dis
Aneurysms located within the mediastinum can be accessed through thoracoscopic approach without open surgery and safely resected using vascular staples.
Core Tip: Superior vena cava (SVC) aneurysms, which are relatively rare, may be symptomatic or cause thrombotic events if large in size, often necessitating surgical intervention. The conventional surgical approach for treating SVC aneurysms includes open thoracotomy and mid-sternotomy. However, in this case, the aneurysm could be safely resected by thoracoscopic simultaneous lateral and subxiphoid access methods. The approach site was 1 cm below the xiphoid process, the fifth mid-axillary line and the seventh anterior axillary line on the right side. To facilitate surgery, CO2 insufflation was used. The aneurysm was safely resected with the use of a vascular staple.
- Citation: Kim SP, Son J. Simultaneous lateral and subxiphoid access methods for safe and accurate resection of a superior vena cava aneurysm: A case report. World J Clin Cases 2023; 11(31): 7635-7639
- URL: https://www.wjgnet.com/2307-8960/full/v11/i31/7635.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i31.7635
Superior vena cava (SVC) aneurysms are a relatively uncommon disease that has not been widely reported. In some instances, where the aneurysm is large, they may cause discomfort or bleeding-related symptoms. In such cases, surgical intervention is often considered when symptoms are present, and the possibility of a thrombotic event exists. The conventional surgical approach primarily utilizes open surgery with the application of cardiopulmonary bypass (CPB) as necessary[1,2]. Herein, we present a case in which we adopted a minimally invasive approach to treat an SVC aneurysm. In addition, we successfully performed a safe and accurate procedure using simultaneous lateral and subxiphoid access methods to ensure safe access to the SVC.
A 58-year-old male presented with intermittent chest pain and persistent discomfort in the chest area.
Symptoms started several months ago and there was no other present illness.
The patient had no any History of past illness.
The patient had no any family history of venous aneurysm.
On physical examination, no abnormal findings were observed.
On laboratory testing, no abnormal findings were observed.
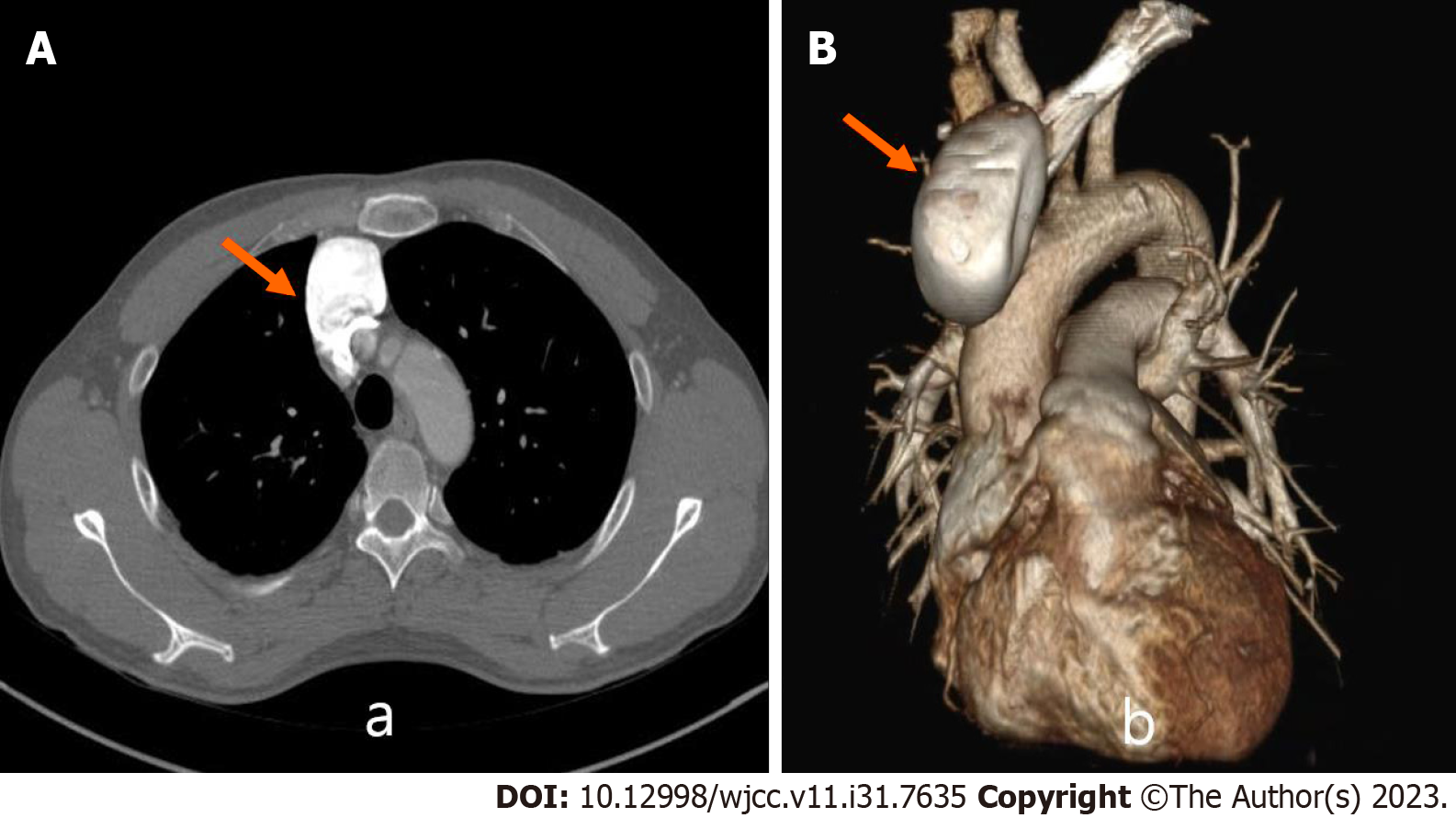
A chest computed tomography (CT) scan revealed a 6.2 cm aneurysm in the left innominate vein and SVC junction (Figure 1). The aneurysm had a saccular appearance with no evidence of a thrombus. In cases of venous aneurysms, the rupture risk is not high, but given the patient’s symptoms and the large size of the aneurysm, which raised concerns regarding a potential thrombotic event, surgical resection was deemed necessary after obtaining patient consent.
The final diagnosis was a 6.2 cm aneurysm in the left innominate vein and SVC junction.
Simultaneous lateral and subxiphoid access were planned to achieve optimal proximal and distal aneurysm control. The patient was intubated and placed in the left semi-lateral position. A 3-cm longitudinal skin incision was made approximately 1 cm below the xiphoid process. After making the skin incision, a wound protector was inserted, and a 10 mm port was formed at the fifth mid-axillary line and the seventh anterior axillary line on the right side. Once the port was inserted, CO2 insufflation at 10 mmHg was performed to retract the pericardium and create sufficient substernal space for surgery.
First, the camera was inserted on the right side to secure the substernal space, and mediastinal dissection was performed through the right side. Next, the camera was removed from the right side and inserted into the subxiphoid site, and the surgery continued. The thymus, innominate vein, and SVC were dissected to secure Aneurysm of distal and proximal site. After umbilical tape encircling, clipping was performed to reduce venous blood flow from the left side. After this procedure, the stalk of the SVC was confirmed and partially resected using a vascular stapler (Covidien, Mansfield, MA, United States) for safe resection of the aneurysm stock, after which its size was reduced by stapling. The remaining aneurysm was resected from the stalk portion using a stapler (see Video 1).
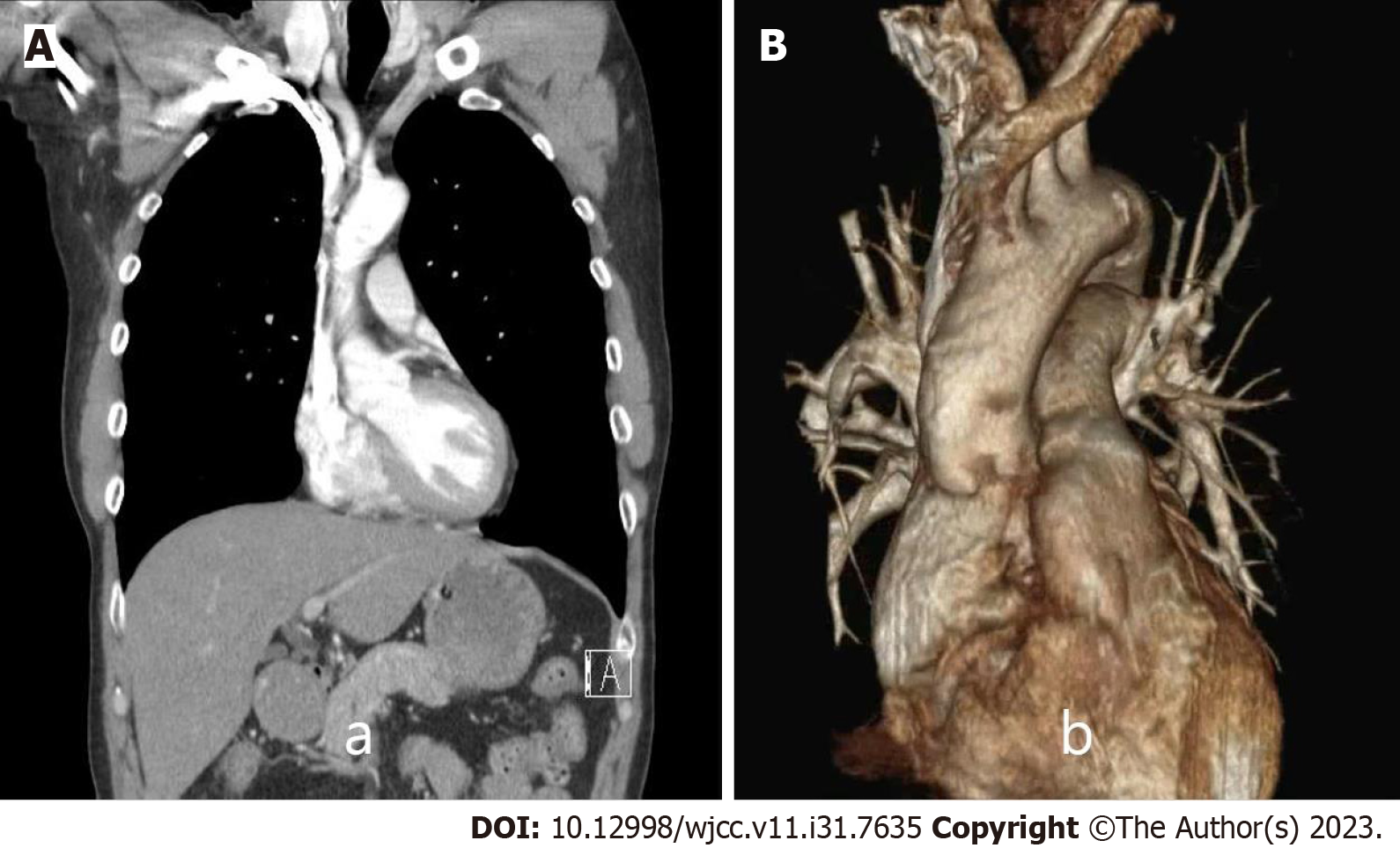
The patient was discharged on the third day after chest tube removal on the second postoperative day with no particular issues. The patient was under follow-up, and no specific findings were observed on CT 1 year after surgery (Figure 2).
Surgical approaches for treating SVC aneurysms include open thoracotomy and mid-sternotomy. In particular, a right thoracotomy has been attempted for aneurysm resection. However, exposing the left innominate vein behind the aneurysm, securing the clamping site, or encircling the vessel’s roof site can be challenging. Moreover, bleeding control is problematic in cases of injury to the opposite innominate vein during dissection. Additionally, thoracotomy increases the chance of changing positions to mid-sternotomy to control bleeding. For these reasons, thoracotomy is not a commonly used approach today.
In contrast, mid-sternotomy allows for the exposure of both jugular veins to the SVC, making it easier to create a clamping site around the aneurysm or perform vessel roof encircling. CPB can be performed at any time during surgery. Currently, mid-sternotomy is widely used in most SVC aneurysm surgeries[1,3].
Surgical visibility is essential for safe SVC aneurysm resection using video-assisted thoracic surgery (VATS). The most significant complication during surgery is the rupture of the innominate vein, which can be lethal. Compared with the right approach, the subxiphoid approach can provide a clear view of the SVC and innominate vein, making it easy to secure the vascular clamp site and promptly address innominate vein rupture. The advantages of the subxiphoid approach have already been demonstrated in VATS thymectomy[4]. Moreover, the subxiphoid approach is essential for the success of minimally invasive approaches. In the present case, since the SVC is on the right side, we believed it would be safer to approach the right side simultaneously with the subxiphoid approach, rather than using the subxiphoid approach alone. There is another consideration for VATS resection. In surgery under CPB, aneurysm resection is performed using superior and inferior SVC and innominate vein clamping, followed by resection and simple suturing. However, this procedure is not possible with minimally invasive approaches. Therefore, we modified the procedure using a vascular stapler to enable aneurysmal resection using a minimally invasive approach. In addition, the vascular stapler is relatively safe for use in the pulmonary area, which has fragile blood vessels. Therefore, the authors concluded that a vascular stapler could be used for aneurysm resection.
Aneurysms located within the mediastinum can be accessed through thoracoscopic approach without open surgery and safely resected using vascular staples.
This study was supported by a 2021 research grant from Pusan National University Yangsan Hospital.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen MCY, Taiwan S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | Morales MM, Anacleto A, Ferreira Leal JC, Greque VG, Souza AS Jr, Wolosker N. Saccular Superior Vena Cava Aneurysm: Case Report and Comprehensive Review. Ann Vasc Surg. 2021;72:666.e23-666.e32. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Kapoor H, Gulati V, Pawley B, Lee JT. Massive fusiform superior vena cava aneurysm in a 47-year-old complicated by pulmonary embolism: A case report and review of literature. Clin Imaging. 2022;81:43-45. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Honda K, Yuzaki M, Fujimoto T, Nishimura Y. Reconstruction of the superior vena cava with an autologous pericardial patch for a giant superior vena cava aneurysm. JTCVS Tech. 2020;4:183-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Abdellateef A, Ali JM, Jiang G, Aresu G, Jiang L. Tips and tricks for success in subxiphoid video-assisted thoracic surgery. J Thorac Dis. 2019;11:292-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |