Published online Oct 26, 2023. doi: 10.12998/wjcc.v11.i30.7457
Peer-review started: July 30, 2023
First decision: August 30, 2023
Revised: September 5, 2023
Accepted: September 28, 2023
Article in press: September 28, 2023
Published online: October 26, 2023
Processing time: 86 Days and 15.5 Hours
Prostatic urethral lift (PUL) therapy is an alternative to minimally invasive and other surgeries in younger patients who want to preserve their sexual and ejaculatory functions, and in elderly male patients with benign prostatic hyper
In our case, a 62-year-old prostate patient who had a PUL operation 8 years ago and had a stone on the PUL material near the bladder neck was treated. The patient’s stone was removed by endoscopic cystolithotripsy using pneumatic fragmentation. Bipolar transurethral resection of the prostate was applied to the patient in the same session. After the patient’s 7-year follow-up, the patient’s complaints relapsed, and cystoscopy was performed again. In cystoscopy, stone formation adjacent to the wall was observed at the junction of the bladder neck to the left lateral wall. The stone was fragmented with a pneumatic lithotripter.
Placing clips too close to bladder neck in the PUL procedure may result in clip migration.
Core Tip: In the prostatic urethral lift procedure, it is important to avoid placing clip materials close to the bladder neck to avoid clip migration.
- Citation: Bozkurt AS, Ekici O, Keskin E, Kocoglu F. Bladder stone due to late clip migration after prostatic urethral lift procedure: A case report. World J Clin Cases 2023; 11(30): 7457-7462
- URL: https://www.wjgnet.com/2307-8960/full/v11/i30/7457.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i30.7457
Benign prostatic hyperplasia affects millions of men worldwide. UroLift (Urolift®) device has recently been used in patients with prostatic lateral lobe hypertrophy with obstructive voiding symptoms who want to avoid sexual and ejaculatory dysfunction[1,2]. Prostatic urethral lift (PUL) is strongly recommended in patients with < 70 mL prostate and with no median lobe but who have lateral lobe hypertrophy with obstructive voiding symptoms and who want to protect from ejaculatory dysfunction[3].
Early complications of PUL include hematuria, dysuria, pelvic pain, urgency, incontinence and urinary tract infections. These complications usually resolve spontaneously within two weeks. In the literature, symptoms such as encrustation, development of stricture, and persistent dysuria and urgency due to incorrect placement of needles have been reported among the late complications[4]. Since the number of studies with long-term follow-up of patients is not sufficient, our information on late complications is limited.
In our study, we aimed to present a case that developed two bladder stones due to clip migration 1 years and 8 years later, which we followed for a long time after PUL was applied.
The patient was admitted to the outpatient clinic with dysuria and pollakiuria started 3 mo ago.
In our case, a 62-year-old prostate patient who had undergone PUL operation 8 years ago, had a stone in the PUL material near the bladder neck, and presented was treated.
In our case, a 62-year-old prostate patient who had undergone PUL operation 8 years ago, had a stone in the PUL material near the bladder neck, and presented was treated.
No feature was observed in the physical examination.
Laboratory examinations reveal nothing abnormal.
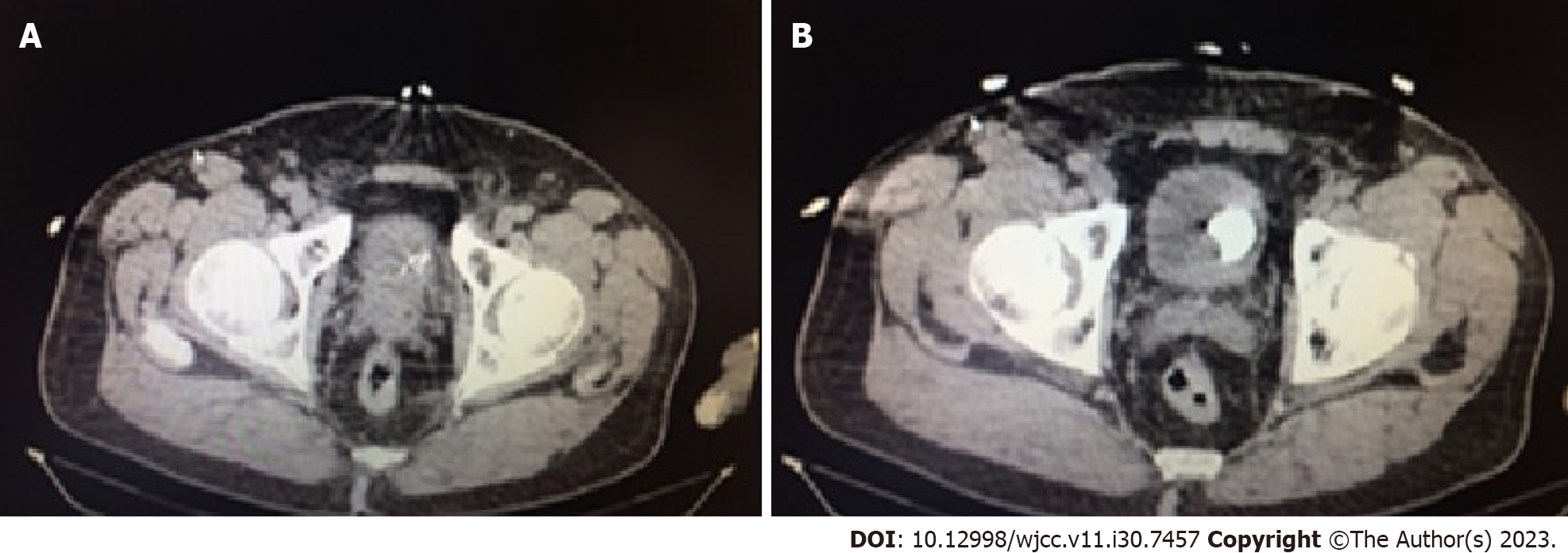
Calcification was detected in the prothatic urethra observed through ultrasound. As further investigation, computed tomography showed that stone was found to be obstructing the bladder at the bladder neck (Figure 1).
The final diagnosis was encrusted PUL clip.
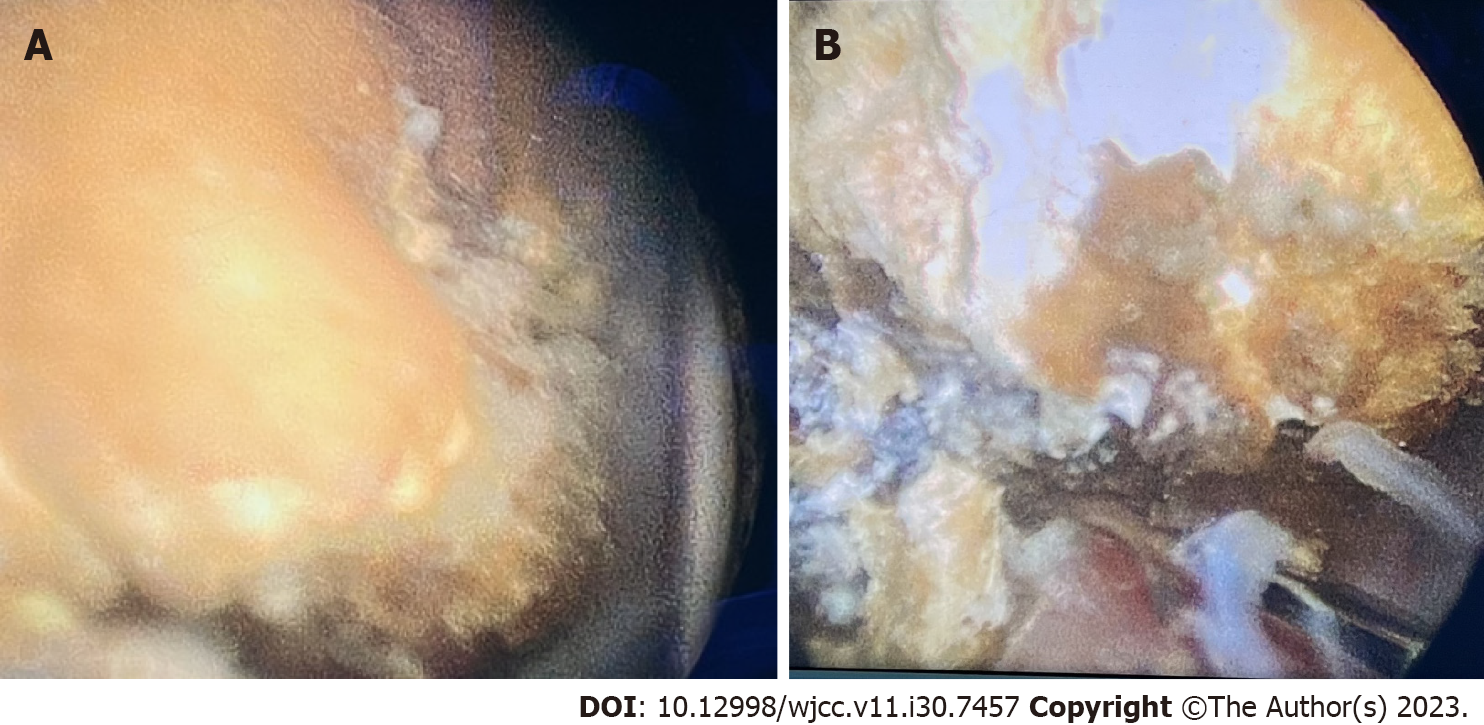
Cystoscopy was conducted. On cystoscopy, a stone was detected on the bladder neck associated with PUL material implanted on the left side prostate of the bladder neck (Figure 2). The patient’s stone was cleaned by endoscopic cystolithotripsy applying fragmentation with pneumatic. The PUL material was located very close to the bladder neck. The patient was given the same session of bipolar transurethral resection (TUR) of prostate. A urethral catheter was inserted. In postoperative day 3 catheter was removed. Maximum flow rate was measured as 21 mL/sec and International Prostate Symptome Score was 8 after TUR.
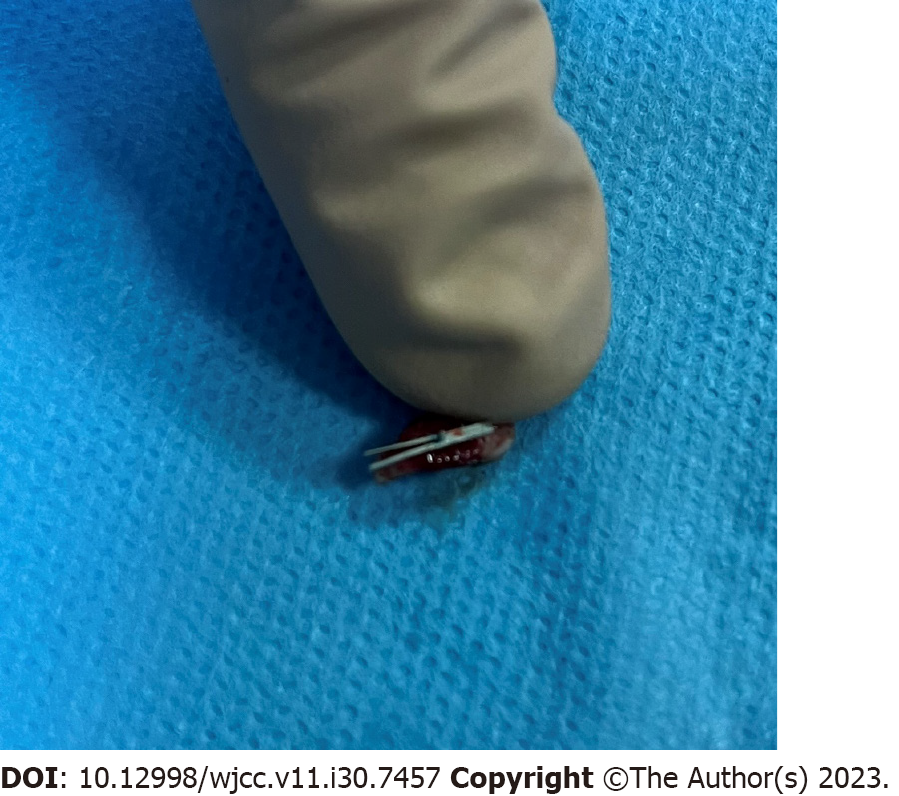
Cystoscopy was performed again when the patient’s complaints started again after 7 years of follow-up. In the cystoscopy, a stone formation adjacent to the wall was observed at the junction of the left side wall of the bladder neck (Figure 3A). The stone was fragmented with pneumatic lithotripter. During fragmentation, a clip attached to the bladder wall was observed under the stone (Figure 3B). In Figure 4, the image of the clip is seen after the stone is completely broken. This clip was removed by performing a TUR to the bladder (Figure 5).
No incrustation was observed in the controls of the patient whose complaints improved.
PUL device is used in patients with prostatic lateral lobe hypertrophy with obstructive voiding symptoms who want to avoid sexual and ejaculatory dysfunction[1,2]. It is clear that urologists need to be ready to perform secondary procedures in the case of PUL failure, as the PUL procedure has increased popularity and 14% treatment failure rate, and it can create enuresis[5]. In our case, a stone was detected on the bladder neck associated with PUL material implanted on the left side prostate of the bladder neck. Stone was fragmented with pneumatic lithotripter and endoscopic cystolithotripsy was performed. Bipolar TUR (prostate) was applied in the same session. PUL material was located near the bladder neck. PUL material was found to result in stone formation if not properly placed laterally in prostatic urethra. In the post-PUL procedure, in order to prevent stone formation, it is important that it should be placed laterally away from the bladder neck[6]. In the case we presented, we think that the reason for the formation of the first stone was the placement of the clip close to the bladder, and the second time the reason for the formation of the stone was the migration of the clip outside the prostate to the bladder.
PUL complications are rare and usually temporary. Intraoperative complications include needle placement in the wrong place, needle breakage, etc. Postoperative complications are usually temporary symptoms such as dysuria, hematuria, urgency[7]. In their study, which included 206 patients with complications recorded according to the Clavien Dindo classification, Cantwell et al[8] they wrote that no class 4 and 5 complications were seen, and 2 patients had class 3 complications. Infective complications have also been reported among postoperative complications[9,10]. The known rates of encrustation and clip migration among the late complications seen in the present case were investigated in the L.I.F.T study, which included 131 patients in whom 642 implants were placed. According to the results, 27 (4%) implants migrated to the bladder and bladder stones occurred in 14 patients[11].
PUL is more suitable for two patient groups in daily practice. The first group is young patients who want to avoid retrograde ejaculation, and the second group is comorbid elderly patients with a high risk of anesthesia. Although PUL provides quick and easy symptomatic relief, recovery is not achieved in patients between 1.4% and 19%. In these patients, retreatment is required within an average of 12-24 mo. In these patients, the TUR prostatectomy procedure can be safely performed[12]. McAdams et al[13] they wrote that the holmium laser enucleation of the prostate (HOLEP) method can also be applied reliably when retreatment is required after PUL. In the patient we presented, we relieved the obstruction in the patient with TUR prostatatectomy with the bipolar method after cystolithotripsy in our first intervention.
Pelvic hematoma cases associated with hematuria are the most common case reports about PUL in the literatüre[14]. Ewing et al[15] stated in their case report that they developed a pelvic hematoma measuring approximately 15 cm in diameter after PUL. This hematoma led to severe hemoglobin reduction (10 U erythrocyte suspension replacement) and acute renal failure requiring dialysis in the patient. This rare complication was attributed to anticoagulant use and prior radiotherapy for prostate cancer in this patient, according to the authors. Spradling et al[16] In the case report they published, they could not relieve massive bleeding after PUL with endourological interventions and stopped the bleeding with prostatic artery embolization. Similar to the case we presented, Kang[17] published the case of a 64-year-old male patient who had stone formation in the bladder neck after PUL applied 2 mo ago. They performed cystolithotripsy and HOLEP. The characteristic of the case we present is that the clip in the lumen migrates to the bladder after 1 year and the clip outside the prostate migrates to the bladder after 8 years. To avoid this complication, it is important not to place the implants close to the bladder neck.
When PUL is placed too close to the bladder neck, it can cause stone formation. Endoscopic cystolithotripsy and bipolar TUR (prostate) together with pneumatics are effective and safe procedures in the treatment of secondary stone development in PUL.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Agrawal M; Gadelkareem RA, Egypt S-Editor: Qu XL L-Editor: A P-Editor: Yuan YY
| 1. | Bardoli AD, Taylor WSJ, Mahmalji W. Can the UroLift prostatic implant device treat the symptoms of benign prostatic hypertrophy, avoid sexual dysfunction and reduce hospital TURP waiting times? A single centre, single surgeon experience and review of the literature. Aging Male. 2017;20:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Bozkurt A, Karabakan M, Keskin E, Hirik E, Balci MB, Nuhoglu B. Prostatic Urethral Lift: A New Minimally Invasive Treatment for Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia. Urol Int. 2016;96:202-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Gravas S, Cornu JN, Gacci M, Gratzke C, Herrmann TRW, Mamoulakis C, Rieken M, Speakman MJ, Tikkinen KAO. Management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). H1Connect. 2021;1-82. [DOI] [Full Text] |
| 4. | Juliebø-Jones P, Somani BK, Tzelves L, Haugland JN, Moen CA, Honoré A, Beisland C. Complications and device failures associated with urolift: Findings from the MAUDE database. Urologia. 2023;3915603231180016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Iqbal M, Jones R, Hughes S, Shergill I. Low power HOLEP after failed urolift: A case report using 50 Watt laser. Urol Case Rep. 2018;16:114-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | C Gratzke, J Barkin, C Roehrborn. 721-Predictors of response to the prostatic urethral lift (PUL) treatment. European Urology Supplements. 2018;17:e1041. [DOI] [Full Text] |
| 7. | Garcia C, Chin P, Rashid P, Woo HH. Prostatic urethral lift: A minimally invasive treatment for benign prostatic hyperplasia. Prostate Int. 2015;3:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Cantwell AL, Bogache WK, Richardson SF, Tutrone RF, Barkin J, Fagelson JE, Chin PT, Woo HH. Multicentre prospective crossover study of the ‘prostatic urethral lift’ for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. BJU Int. 2014;113:615-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Chidurala S, Bheemarasetti M. Unusual Presentation of Infective Endocarditis Following a Prostatic Urethral Lift. Cureus. 2022;14:e26919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Goodsell S, Lewis A, Domanski K. Bilateral Knee Septic Arthritis after Prostatic Urethral Lift: A Case Report. J Orthop Case Rep. 2023;13:68-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Roehrborn CG, Gange SN, Shore ND, Giddens JL, Bolton DM, Cowan BE, Brown BT, McVary KT, Te AE, Gholami SS, Rashid P, Moseley WG, Chin PT, Dowling WT, Freedman SJ, Incze PF, Coffield KS, Borges FD, Rukstalis DB. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L.I.F.T. Study. J Urol. 2013;190:2161-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 167] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 12. | Batura D, Sahibzada I. TURP in the era of UroLift. Int Urol Nephrol. 2018;50:877-878. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | McAdams S, Funk JT, Navetta AF, El Tayeb MM, Humphreys MR. Holmium Laser Enucleation of the Prostate After Prostatic Urethral Lift Surgery: Feasibility and Technical Considerations from a Multi-Institutional Case Series. J Endourol. 2017;31:774-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Pollock GR, Bergersen A, Chaus FM, Gretzer M. Pelvic Hematoma Following UroLift procedure for BPH. Urology. 2019;133:e3-e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Ewing B, Alavi-Dunn N, Hamann H, Danforth T. Large pelvic hematoma following UroLift procedure causing renal failure requiring dialysis. Urol Case Rep. 2021;34:101514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Spradling K, Deb S, Brubaker WD, Gill H, Conti S. Prostate Artery Embolization Used in the Management of Transfusion-Dependent Hematuria After Prostatic Urethral Lift Procedure in a Patient with Thrombocytopenia: A Case Report. J Endourol Case Rep. 2020;6:238-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Kang J. Bladder stone secondary to prostatic urethral lift (PUL) for benign prostatic hyperplasia (BPH). Urol Case Rep. 2021;39:101777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |