Published online Oct 26, 2023. doi: 10.12998/wjcc.v11.i30.7393
Peer-review started: June 24, 2023
First decision: August 9, 2023
Revised: September 7, 2023
Accepted: September 11, 2023
Article in press: September 11, 2023
Published online: October 26, 2023
Processing time: 122 Days and 15.7 Hours
As left bundle branch pacing (LBBP) is more like physiological pacing, LBBP has emerged as a novel pacing strategy that uses the native conduction system to improve ventricular synchronization with stable pacing parameters. LBBP has been revealed associated with a significantly reduced risk of new-onset atrial fibrillation and heart failure compared with conventional permanent pacemaker implantation.
A 64-year-old man was admitted with a 24-h history of chest distress and shortness of breath, which continued unabated. The patient had no symptoms of chest pain, dizziness, syncope, nausea nor vomiting. There were no abnormalities found in routine examinations after admission. Twelve-lead electrocardiogram presented a result of 2:1 atrioventricular block. Coronary angiography was performed the next day and no abnormality was found. Finally, the patient agreed to received LBBP and signed the informed consent. During the process of withdrawing the Medtronic Model 3830 lead into sheath, we found the lead helix was wrapped around the chordae tendineae of the septal valve of tricuspid. Attempts to rotate the 3830 lead failed to release the lead helix from the chordae tendineae, and ultimately we used radiofrequency ablation to ablate the wrapped chordae tendineae.
Radiofrequency ablation effectively solved this problem without complications. It is an effective and reliable method to resolve lead winding chordae.
Core Tip: Radiofrequency ablation can be used to separate the lead helix from a wrapped chordae tendineae. This method helped our patient avoid a surgical procedure. The innovation of this novel technique is its use of a high concentration of saline (10% NaCl) to reduce impedance.
- Citation: Liu TF, Ding CH. Lead helix winding tricuspid chordae tendineae: A case report. World J Clin Cases 2023; 11(30): 7393-7397
- URL: https://www.wjgnet.com/2307-8960/full/v11/i30/7393.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i30.7393
As left bundle branch pacing (LBBP) is more like physiological pacing, LBBP has emerged as a novel pacing strategy that uses the native conduction system to improve ventricular synchronization with stable pacing parameters. LBBP has been revealed associated with a significantly reduced risk of new-onset atrial fibrillation and heart failure compared with conventional permanent pacemaker implantation[1].
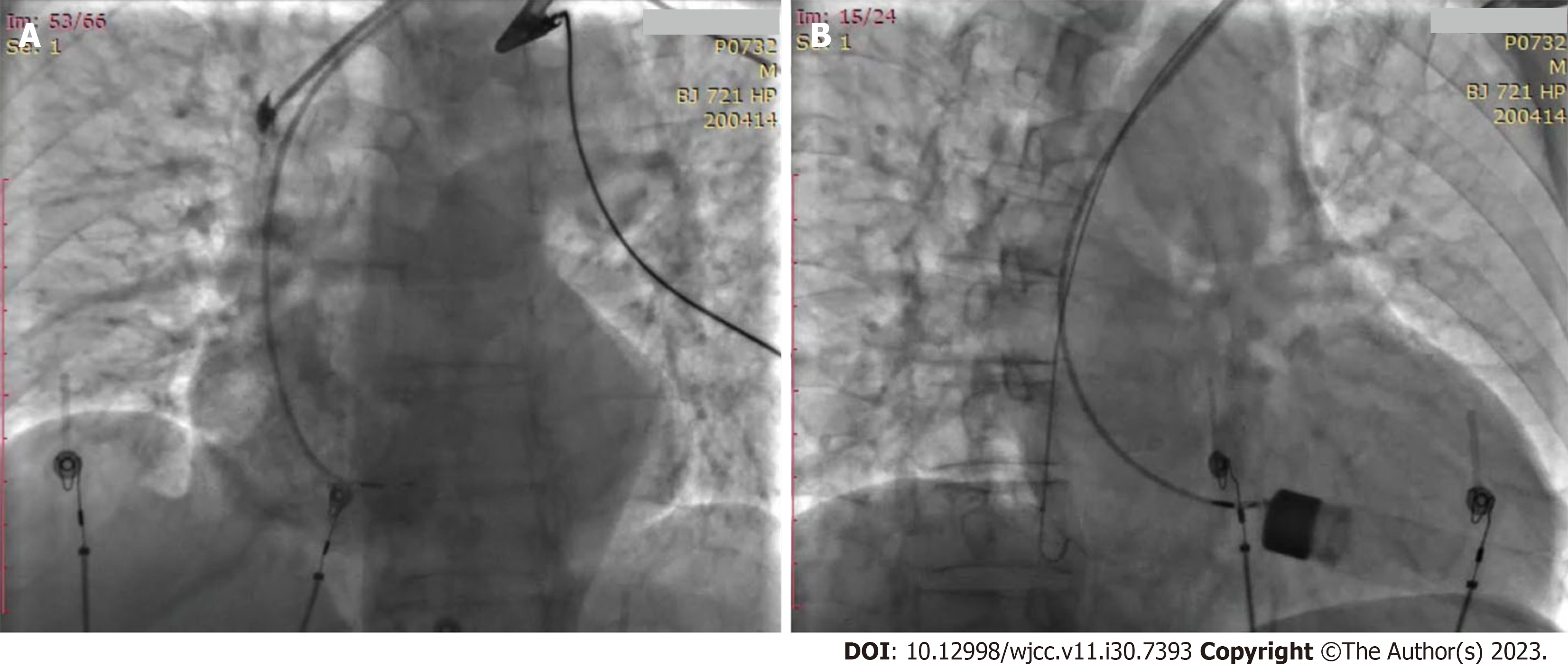
In our experience with lead implantation of the Medtronic Model 3830 (Minneapolis, MN, United States), we encountered a problem. The pacing position was not ideal, and the intracardiac electrocardiogram (ECG) indicated Q waves in the inferior wall leads (II III AVF). Our aim was to adjust the lead position to get a good parameter. During the process of withdrawing the 3830 lead to sheath, however, we found the lead helix was wrapped around the chordae tendineae of the septal valve of tricuspid. We performed a right ventricular angiography immediately (Figure 1). We rotated the lead clockwise as well as counterclockwise, and in the meantime sent the 3830 lead forward as well as backward while adjusting the sheath tube forward for sending or withdrawal at different angles. After nearly 2 h of attempts, we failed to release the lead helix from the chordae tendineae.
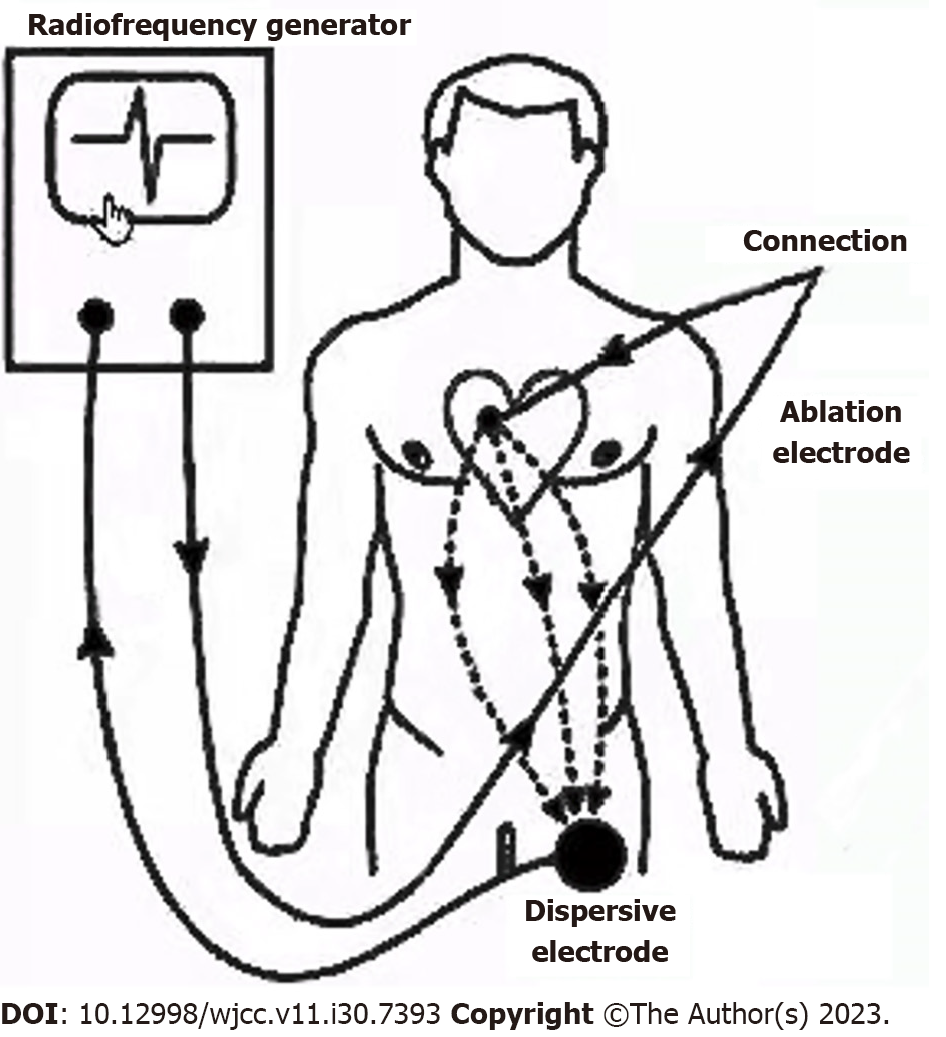
Finally, we used radiofrequency ablation to ablate the wrapped chordae tendineae. We connected the tip of the ablation catheter to the end of the 3830 lead (cathode ring). In this manner, the ablation catheter, the 3830 lead with the winding chordae tendineae, and the back electrode plate of the patient linked with the radiofrequency generator formed a closed current loop (Figure 2). Radiofrequency energy successfully transmitted to the tip of the 3830 lead. Unfortunately, the radiofrequency generator failed to work as the impedance was over the maximum (350 ohms) allowed.
We then tried to add another back electrode to reduce the impedance from 350 ohms to 300 ohms. But it failed to discharge, again because of the high impedance. Finally, a high concentration of saline (10% NaCl) was injected into the sheath of the electrode (Supplementary Figure 1) and the impedance was reduced from 300 ohms to 125 ohms. During the 3-s abatement, the lead helix successfully separated from the chordae tendineae.
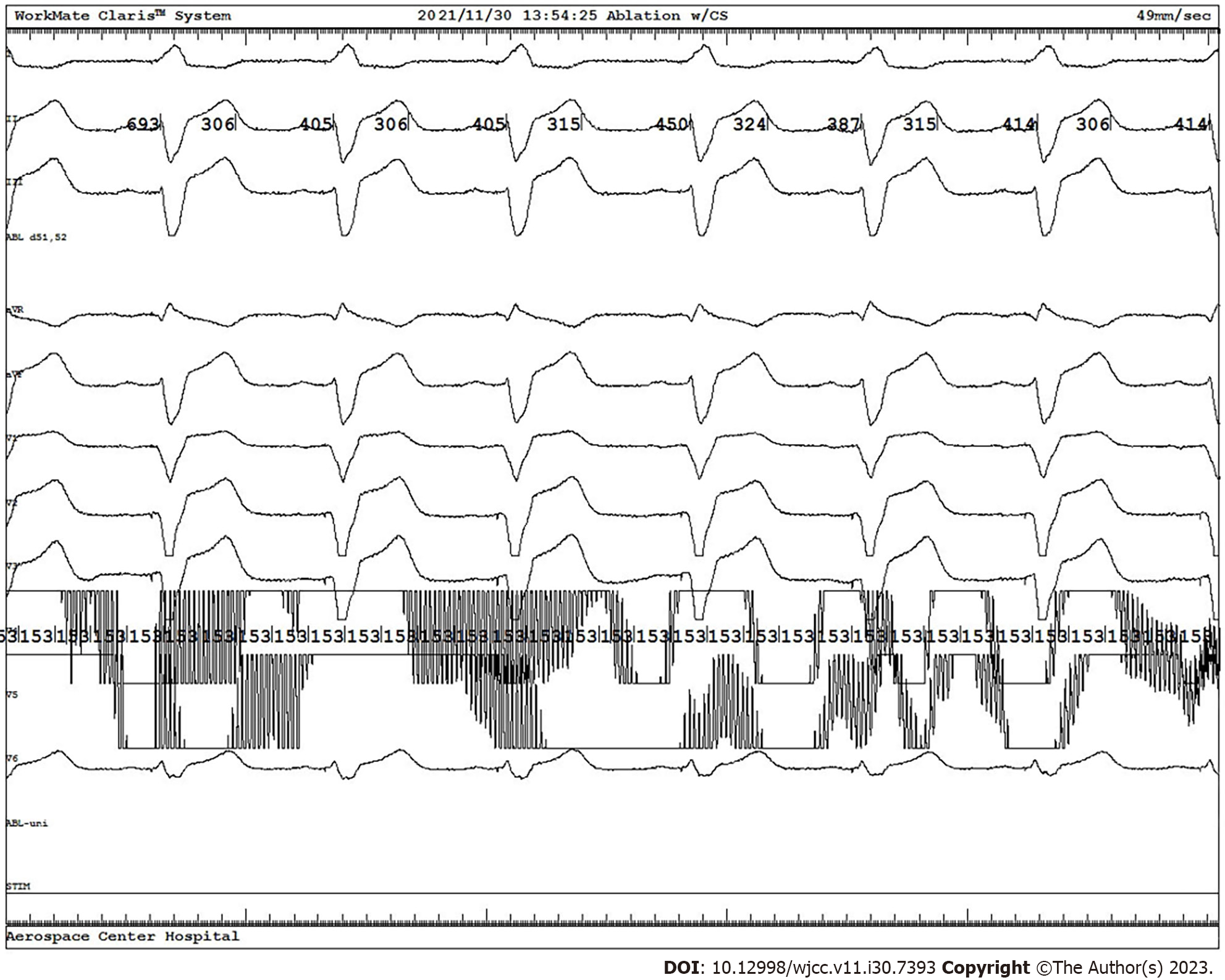
We changed to a new Model 3830 electrode and successfully implanted it into the left bundle branch area, with good capture threshold and pacing pattern (Figure 3). After that, we performed a reexamination by ECG and discovered a mild regurgitation signal of tricuspid and pericardial effusion. The patient had no complaint of discomfort.
The pacemaker was programmed before the patient was discharged, and the pacing threshold, sense, and impedance were good. The patient was regularly followed up in the clinic and the pacemaker worked normally.
A 64-year-old man was admitted with a 24-h history of chest distress and shortness of breath. The patient had no symptoms of chest pain, dizziness, syncope, nausea nor vomiting.
Symptoms started 24 h before, with no reason. The patient was consequently sent to the Emergency Room of Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine.
The patient had a 14-year history of hypertension. The highest blood pressure recorded was 150/90 mmHg. Valsartan was taken regularly and controlled the blood pressure well.
The patient denied any family history of disease.
Body temperature, 36.5 ºC; blood pressure, 108/65 mmHg; heart rate, 38 beats per min; respiratory rate, 18 breaths per min.
There was no abnormality in routine laboratory examinations made after admission.
Twelve-lead ECG presented a result of 2:1 atrioventricular block (AVB) (Supplementary Figure 2). Coronary angiography was performed the next day and no abnormality was found (Supplementary Figure 3).
Combined with the patient’s medical history and the examinations, the final diagnosis was 2:1 AVB and hypertension.
Permanent pacemaker with LBBP was implanted for the patient. During the process of withdrawing the 3830 leads to the sheath, we found the lead helix was wrapped around the chordae tendineae of the septal valve of the tricuspid. Finally, we used radiofrequency ablation from the 3830 lead helix to ablate the wrapped chordae tendineae.
The patient was regularly followed up at the clinic. The patient had no symptoms of discomfort and an ECG was added (Supplementary Figure 4). The echocardiography showed mild tricuspid regurgitation (Supplementary Figure 5).
The present case involved a rare occurrence of a pacemaker lead wrapped around the chordae tendineae. This is the first case to describe how to resolve this problem by radiofrequency ablation with high impedance. We successfully solved this problem using a high concentration of saline (10% NaCl) to reduce the impedance according to Ohm's law[2] and the principles of radiofrequency ablation[3,4]. When the radiofrequency energy was sent to 3830 lead helixes, heat was generated to dehydrate and denature the wrapped chordae tendineae.
Since intracardiac echocardiography was unavailable in the catheter lab which may have shown the wrapping situation of the electrode tip and chordae tendineae, this could have helped to guide us and allow for visualization of a way to rotate the lead.
The patient was satisfied with the result of the treatment, and for avoiding mental, financial, and physical damage by iatrogenic injuries.
This case demonstrates how to resolve a Model 3830 lead wrapped around the chordae tendineae.
Radiofrequency ablation with the injection of a high concentration of saline in the sheath effectively solves the problem of the Medtronic 3830 lead wrapped around the chordae tendineae without complications.
We thank all doctors in cardiology for supporting and coordinating with us to get the available data and materials.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sharma D, India S-Editor: Liu JH L-Editor: Filipodia P-Editor: Yu HG
| 1. | Zhu H, Li X, Wang Z, Liu Q, Chu B, Yao Y, Liu Z, Xie R, Fan X. New-onset atrial fibrillation following left bundle branch area pacing vs. right ventricular pacing: a two-centre prospective cohort study. Europace. 2023;25:121-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 2. | Anderson WP, Hendrix DL, Higinbotham N. The effect of cyanide and carbon monoxide on the electrical potential and resistance of cell membranes. Plant Physiol. 1974;54:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Lavergne T, Sebag C, Ollitrault J, Chouari S, Copie X, Le Heuzey JY, Guize L. [Radiofrequency ablation: physical bases and principles]. Arch Mal Coeur Vaiss. 1996;89 Spec No 1:57-63. [PubMed] |
| 4. | Aerts S, Calderon C, Valič B, Maslanyj M, Addison D, Mee T, Goiceanu C, Verloock L, Van den Bossche M, Gajšek P, Vermeulen R, Röösli M, Cardis E, Martens L, Joseph W. Measurements of intermediate-frequency electric and magnetic fields in households. Environ Res. 2017;154:160-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |