Published online Jan 26, 2023. doi: 10.12998/wjcc.v11.i3.655
Peer-review started: September 29, 2022
First decision: December 13, 2022
Revised: December 15, 2022
Accepted: January 5, 2023
Article in press: January 5, 2023
Published online: January 26, 2023
Processing time: 119 Days and 8.7 Hours
Diffuse idiopathic skeletal hyperostosis (DISH) is a disorder characterised by the calcification and ossification of ligaments and entheses. It is a frequent occurrence in elderly males, but rarely encountered in younger individuals.
A 24-year-old male was admitted to the hospital due to low back pain accompanied with numbness in both lower limbs for 10 d. Upon clinical examination and imaging tests, the patient was diagnosed with DISH with Scheuermann disease and thoracic spinal stenosis. Before the operation and medical treatment, the patient had hypoesthesia of the skin below the xiphoid process. Afterward, a standard laminectomy was conducted using ultrasonic bone curette and internal fixation was applied. Subsequently, the patient was given corticosteroids, neurotrophic drugs, hyperbaric oxygen and electric stimulation. As a result of the treatment, the patient’s sensory level decreased to the navel level and there was no major change in the muscle strength of the lower limbs. During follow-up, the patient’s skin sensation has returned to normal.
This case is a rare instance of DISH co-existing with Scheuermann’s disease in a young adult. This provides a valuable reference point for spine surgeons, as DISH is more commonly observed in middle-aged and elder adults.
Core Tip: This case report presents a rare instance of diffuse idiopathic skeletal hyperostosis in a 24-year-old male patient, which is a condition that is usually seen in elderly males. The patient was also diagnosed with Scheuermann disease. By providing clinical data and treatment experience of this patient, it is hoped that it will help to improve the understanding of related diseases, and reduce the chances of misdiagnosis.
- Citation: Liu WZ, Chang ZQ, Bao ZM. Young thoracic vertebra diffuse idiopathic skeletal hyperostosis with Scheuermann disease: A case report. World J Clin Cases 2023; 11(3): 655-661
- URL: https://www.wjgnet.com/2307-8960/full/v11/i3/655.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i3.655
Diffuse idiopathic skeletal hyperostosis (DISH) is an ailment caused by the calcification and ossification of the entheses that primarily affects the spine and other peripheral areas[1]. Primarily, DISH affects the thoracic spine of the axial skeleton; however, other spinal regions are often affected too. Studies demonstrate that DISH is more predominant among middle-aged and elderly individuals and the rate of occurrence increases with age. Moreover, there is a higher rate of male patients than female patients[2]. Scheuermann’s disease was initially described by Scheuermann[3], a Danish physician, in 1921. The main symptom of this condition is the formation of three adjacent vertebrae that are angled by at least 5 degrees, resulting in the spine’s kyphoscoliosis. Radiographic features of Scheuermann’s disease include wedged vertebrae, irregular vertebral endplates, and Schmorl’s nodes[4]. In this paper, we present a case of a young patient who was eventually diagnosed with DISH in combination with Scheuermann disease and thoracic spinal stenosis (TSS) in our hospital. While DISH is usually observed in middle-aged and elderly individuals, there is a lack of reports on young DISH patients. Moreover, it is even rarer for young DISH to be associated with Scheuermann disease, thus making this case worth reporting. We have reviewed the characteristics of the case, as well as the diagnosis and treatment process, in order to expand the current knowledge on the diagnosis and treatment of related diseases.
The 24-year-old male patient was hospitalized for 10 d due to lower back pain and numbness in both lower limbs.
The 24-year-old male patient was hospitalized for 10 d due to lower back pain and numbness in both lower limbs. On physical examination, thoracodorsal kyphosis was observed and the skin below xiphoid had hypoesthesia. Furthermore, the muscle strength of the right iliopsoas, quadriceps femoris and biceps femoris was graded as III, while the right tibialis anterior and extensor dorsi were graded as IV. At admission, the patient experienced radiating pain in his waist, which had a VAS score of 8.
The patient reported no other medical history such as hypertension and diabetes.
The patient denied any personal and family history of illness.
On physical examination, thoracodorsal kyphosis was observed and the skin below xiphoid had hypoesthesia. Furthermore, the muscle strength of the right iliopsoas, quadriceps femoris and biceps femoris was graded as III, while the right tibialis anterior and extensor dorsi were graded as IV. At admission, the patient experienced radiating pain in his waist, which had a VAS score of 8.
To differentiate DISH from ankylosing spondylitis, it is necessary to test for human leukocyte antigen-B27 (HLA-B27). The patient’s HLA-B27 index is within the normal range. Additionally, the patient’s erythrocyte sedimentation rate, blood routine test and other biochemical indicators are all within the normal range.
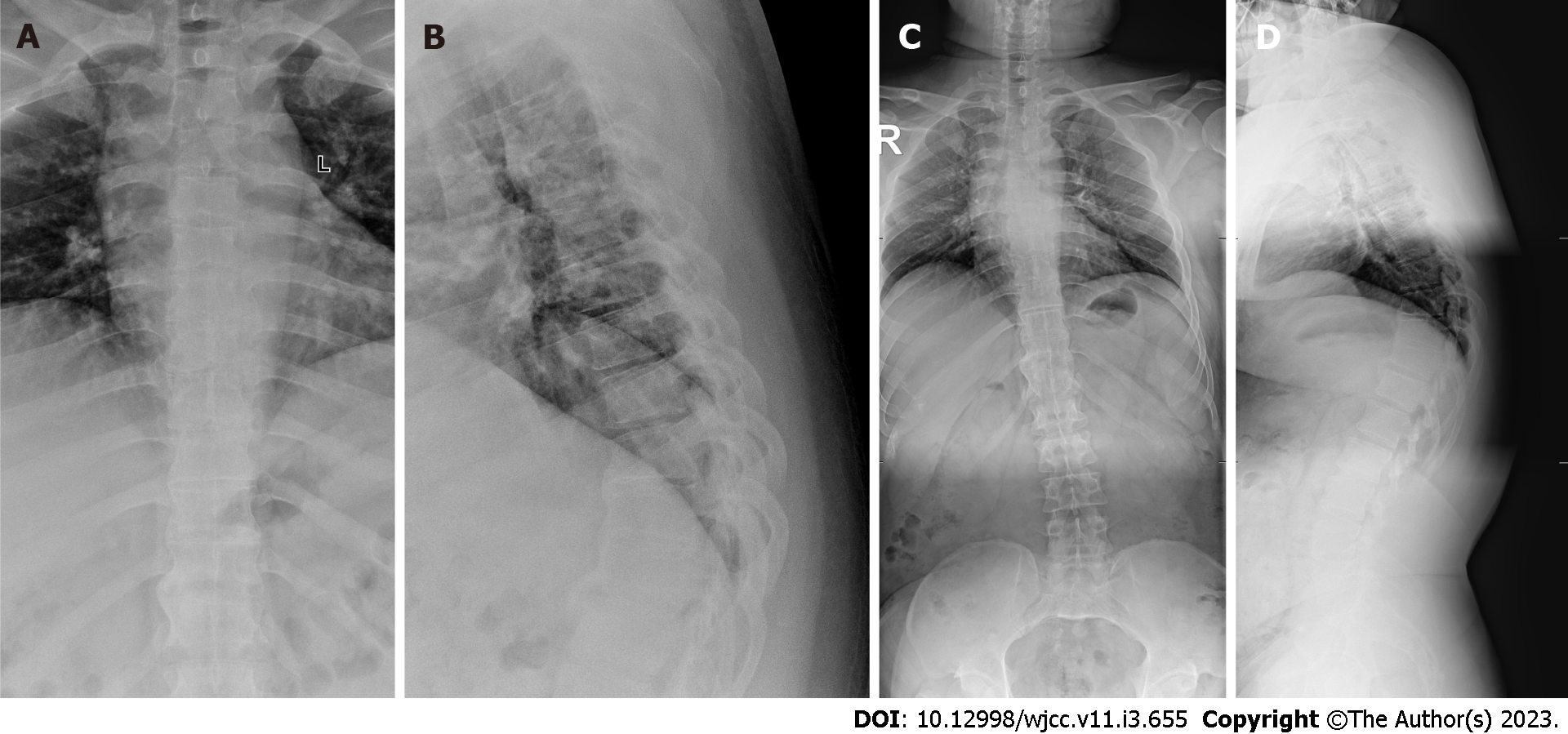
Anterior-lateral X-ray: Kyphosis of the thoracic spine is present, with calcification of the anterior longitudinal ligament and lamellar ossification/floating bone bridge on the medial-inferior and medial-superior sides of the anterior and lateral edges of vertebral plates. Additionally, there is a local wedge-shaped deformation of the lower thoracic vertebra (Figure 1).
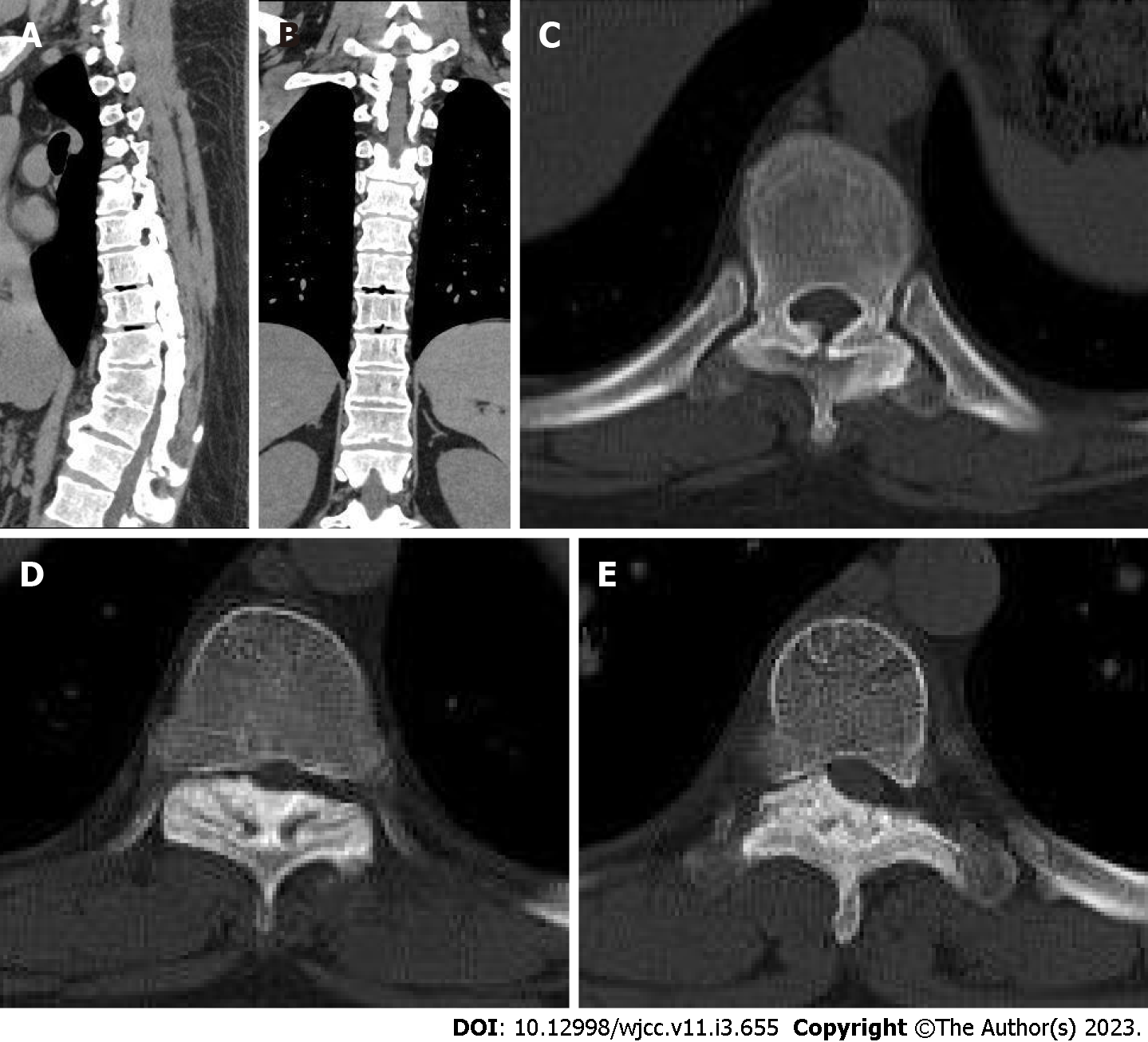
Thoracic computed tomography (CT) scan revealed a kyphosis in the thoracic spine and calcification of the anterior longitudinal ligament of multiple vertebral bodies. The T8-12 vertebral body was wedge-shaped with a narrow front and wide back. The T5/6, T7/8, and T8/9 intervertebral discs were observed to protrude backward, resulting in compression of the corresponding horizontal segment dural sac. Furthermore, the adequate space of the spinal canal was constricted, and the spinal cord was compressed due to hyperplasia and sclerosis of the bilateral facet joints of the T7-9 vertebral body (Figure 2).
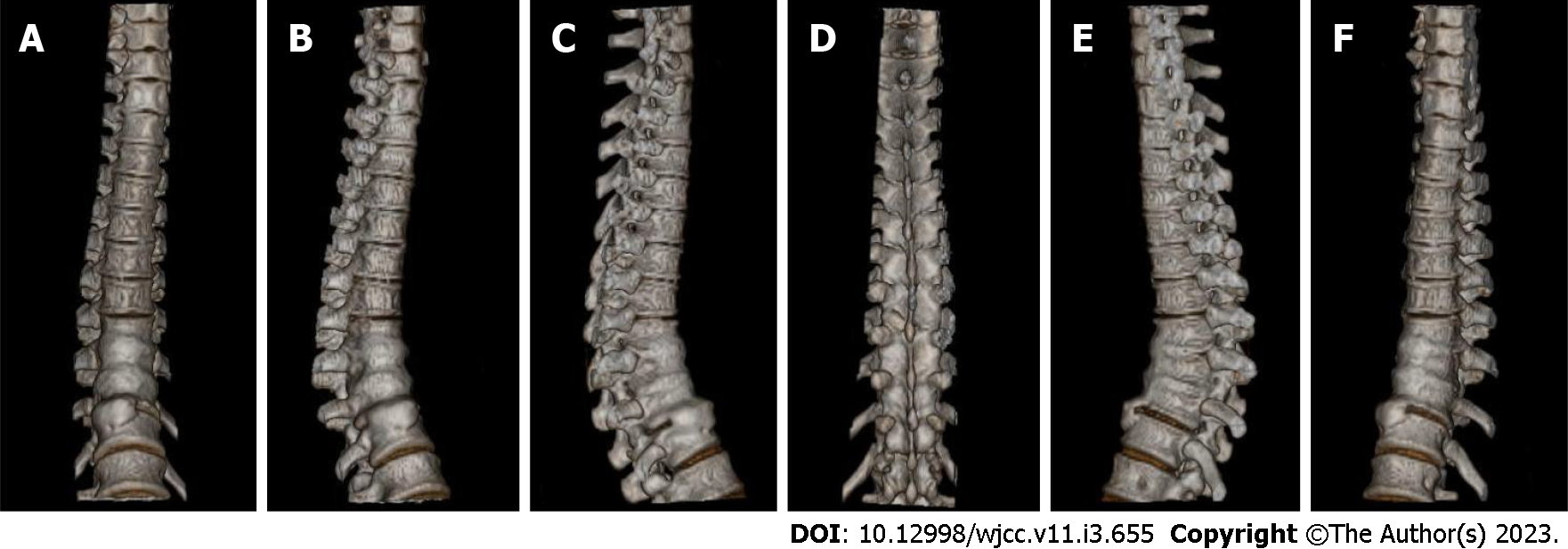
Results of a three-dimensional reconstruction revealed calcification of the anterior longitudinal ligament of numerous vertebral bodies, which has formed a bony bridge. The T8-12 vertebral body was found to be wedge-shaped, with a narrow front and wide back, as well as hyperplasia and sclerosis of both facet joints of the T7-9 vertebral body (Figure 3).
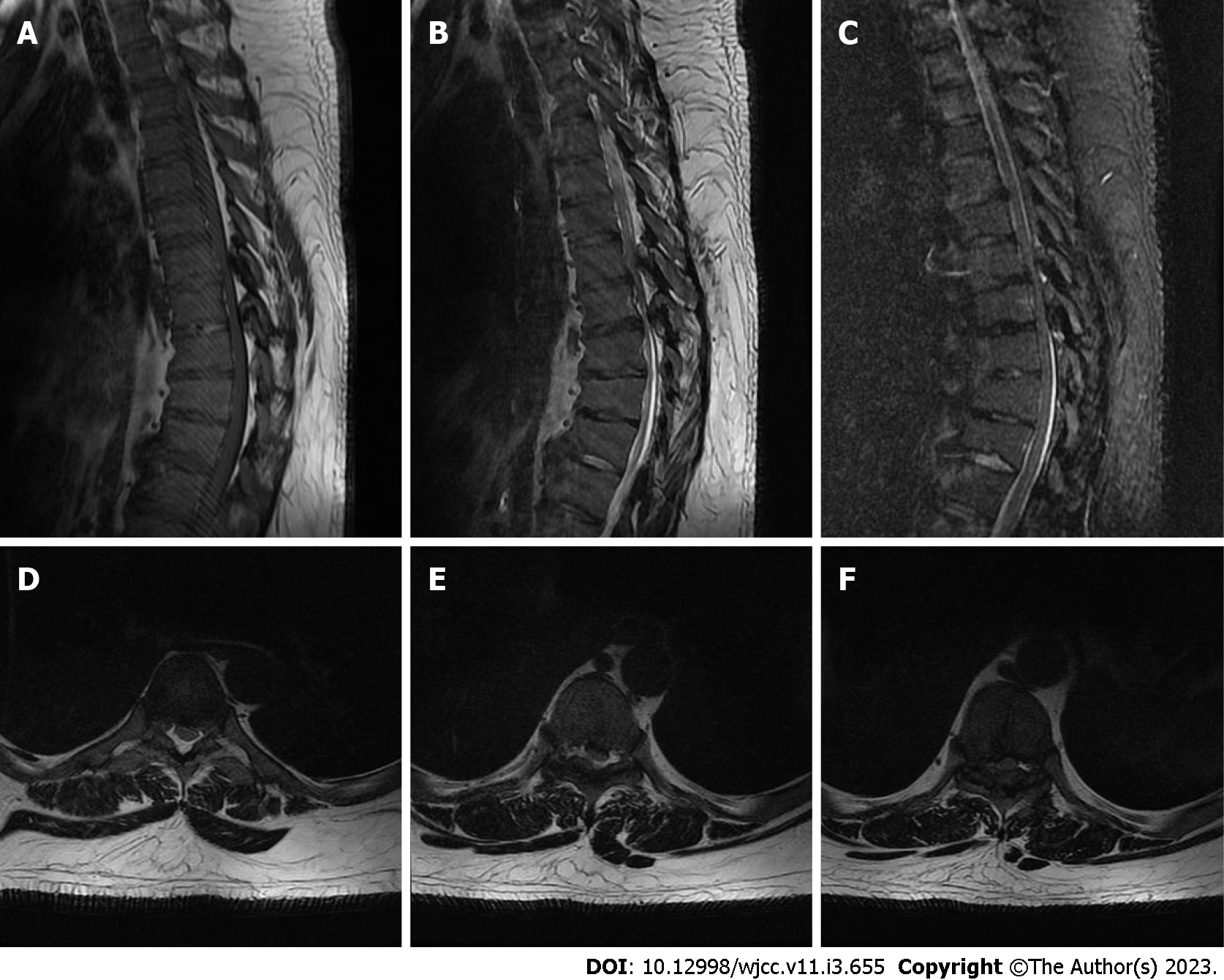
Thoracic magnetic resonance imaging showed kyphosis in the local thoracic spine. The T8-12 vertebrae have a wedge-like shape, with a thin anterior side and a wide posterior side. The intervertebral discs between T5/6, T7/8, and T8/9 protrude posteriorly and the adjacent dural sac is compressed. Additionally, no alterations in the spinal cord signal intensity were observed (Figure 4).
The patient was diagnosed with DISH with Scheuermann disease and TSS.
The patient’s TSS symptoms were serious, resulting in paraplegia of the lower limbs. To address this, we opted for a laminectomy with an ultrasonic bone curette and internal fixation. After the procedure, we administered corticosteroids, neurotrophic medications, hyperbaric oxygen, and electrical stimulation to the patient for further treatment.
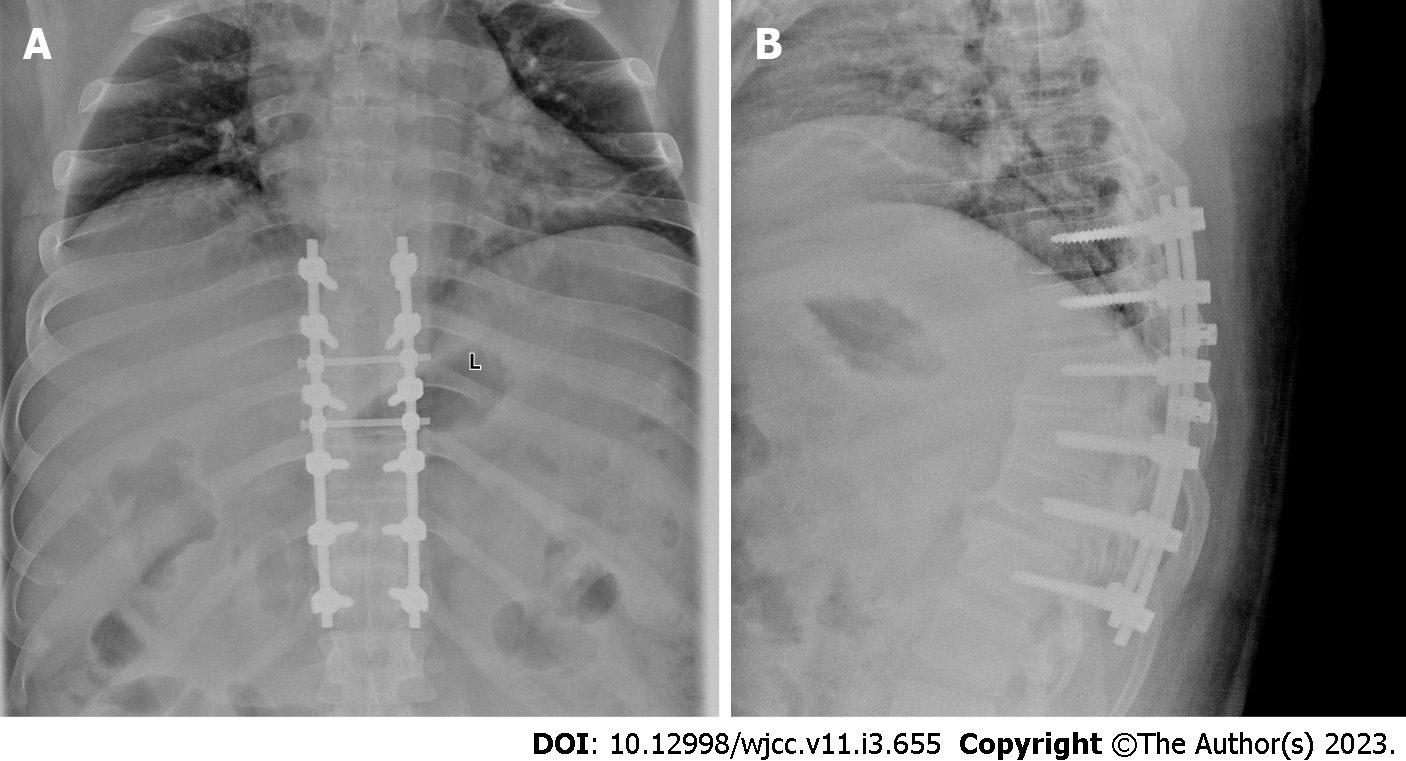
After the surgery and medication, the patient’s sensory level decreased to the navel level with no noteworthy alteration in the muscle strength of the lower limbs. The VAS score was also decreased to 2 points. During the follow-up, the lumbar pain was completely gone and the patient’s skin sensation was back to normal. The patient was also capable of walking 1.5 kilometers. The postoperative reexamination revealed that the internal fixation position was successful (Figure 5).
The diagnosis of DISH is based on radiographic criteria proposed by Resnick and Niwayama[5] in 1976, which include the presence of flowing calcification and ossification along the anterolateral aspects of at least four contiguous vertebral bodies, relative preservation of disc height in the problematic areas, and absence of apophyseal joint bony ankylosis and sacroiliac joint erosion, sclerosis or bony fusion. This patient fulfilled these criteria and was thus diagnosed with DISH. DISH is most commonly found in the thoracic spine, where it presents as wavy ossification in front of the thoracic centrum, forming bone bridges across the intervertebral spaces, and is most commonly located on the right side[6]. It may also occur in the lower cervical spine and the upper lumbar segments[7]. It is important to differentiate DISH from ankylosing spondylitis, which can be done by examining the patient’s joint space, inflammatory manifestations of the articular surface, morning stiffness, and limited joint mobility, as well as HLA-B27 values. In this case, the patient did not present with any of these features and had normal HLA-B27 values, thus excluding the possibility of ankylosing spondylitis.
Patients with DISH usually do not present with any noticeable symptoms and rarely require treatment. However, when DISH is accompanied by ossification of the ligamentum flavum and posterior longitudinal ligament, which compresses the spinal cord or nerve, surgery is necessary[8]. This condition is usually discovered incidentally during imaging tests, and the prevalence rate increases with age[6]. Studies have found that the incidence of DISH in males over 50 is more than 25%[2], and is associated with age, obesity, and diabetes[9]. In contrast, the incidence of DISH in individuals under 40 is extremely low, with only a few cases reported in the literature[10]. A Japanese study of 345 patients with spinal column diseases revealed that the youngest patient with DISH was 37 years old[11]. Additionally, a study of 1479 patients undergoing chest CT scans showed that the average age of DISH was 54.7 years old, with only one patient under the age of 40[6]. A cross-sectional study of 2000 subjects in China found that the mean age of DISH was 58.7 years old, and there were no cases of DISH in subjects under 40[10].
In 1964, Sorensen first proposed X-ray imaging diagnostic criteria for Scheuermann’s disease[12], which includes at least three adjacent vertebrae with a minimum of 5° wedging. Subsequent research has expanded the understanding of the condition and refined the diagnostic criteria, which include vertebral body wedging, vertebral endplate irregularity, Schmorl’s nodes, and narrowing of intervertebral disk spaces. Common symptoms in the early stages of the disease include chest and back pain. Our patient was a young individual with no prior history of spinal deformity, and they presented with the aforementioned symptoms. Scheuermann’s disease is a relatively common condition in adolescents, with an estimated prevalence of 1%-8%[13]. It usually presents as mild kyphosis and does not usually cause functional impairment. However, if the kyphosis worsens and is accompanied by disc herniation or spinal stenosis, prompt surgical intervention may be necessary[12]. Furthermore, a recent study reported a prevalence of syringomyelia of 5.8% in patients with Scheuermann’s disease[14], therefore, any changes in spinal cord signals should be taken seriously and prompt surgical intervention should be considered.
TSS is associated with secondary pathological factors such as ossification of ligamentum flavum and ossification of posterior longitudinal ligament secondary to ankylosing spondylitis and DISH. It is reported that the highest incidence of TSS is seen in individuals aged 50-60 years old[15]. When TSS has resulted in obvious spinal cord compression and deformation (grade IV) and the patient has developed neurologic deficits, decompression surgery should be considered[16]. Depending on the location of the lesion, TSS surgery mainly includes dorsal spinal canal decompression and ventral or annular spinal canal decompression[17]. In the present case, spinal canal decompression and pedicle screw fixation were performed taking into account the patient’s medical history and rate of disease progression. Post-operatively, the patient’s sensory level decreased without any worsening such as spinal cord ischemia-reperfusion injury. Additionally, the physiological curvature and stability of the spine were restored.
The rarity of DISH with Scheuermann disease and TSS in a 24-year-old patient poses a challenge in terms of early detection and diagnosis. Thus, medical practitioners should strive to broaden their knowledge and differential diagnosis skills regarding related diseases in order to improve the accuracy of diagnosis. By studying the clinical data and treatment experience of similar patients, doctors can gain a better understanding of DISH in young patients and reduce the chances of misdiagnosis or delayed diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Mader R, Verlaan JJ, Eshed I, Bruges-Armas J, Puttini PS, Atzeni F, Buskila D, Reinshtein E, Novofastovski I, Fawaz A, Kurt V, Baraliakos X. Diffuse idiopathic skeletal hyperostosis (DISH): where we are now and where to go next. RMD Open. 2017;3:e000472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Holton KF, Denard PJ, Yoo JU, Kado DM, Barrett-Connor E, Marshall LM; Osteoporotic Fractures in Men (MrOS) Study Group. Diffuse idiopathic skeletal hyperostosis and its relation to back pain among older men: the MrOS Study. Semin Arthritis Rheum. 2011;41:131-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine (Phila Pa 1976). 2007;32:S115-S119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Bezalel T, Carmeli E, Been E, Kalichman L. Scheuermann's disease: current diagnosis and treatment approach. J Back Musculoskelet Rehabil. 2014;27:383-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976;119:559-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 582] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 6. | Hiyama A, Katoh H, Sakai D, Sato M, Tanaka M, Watanabe M. Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) assessed with whole-spine computed tomography in 1479 subjects. BMC Musculoskelet Disord. 2018;19:178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Mader R, Baraliakos X, Eshed I, Novofastovski I, Bieber A, Verlaan JJ, Kiefer D, Pappone N, Atzeni F. Imaging of diffuse idiopathic skeletal hyperostosis (DISH). RMD Open. 2020;6:e001151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Le HV, Wick JB, Van BW, Klineberg EO. Diffuse Idiopathic Skeletal Hyperostosis of the Spine: Pathophysiology, Diagnosis, and Management. J Am Acad Orthop Surg. 2021;29:1044-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Kuperus JS, Mohamed Hoesein FAA, de Jong PA, Verlaan JJ. Diffuse idiopathic skeletal hyperostosis: Etiology and clinical relevance. Best Pract Res Clin Rheumatol. 2020;34:101527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 10. | Liang H, Liu G, Lu S, Chen S, Jiang D, Shi H, Fei Q. Epidemiology of ossification of the spinal ligaments and associated factors in the Chinese population: a cross-sectional study of 2000 consecutive individuals. BMC Musculoskelet Disord. 2019;20:253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 11. | Toyoda H, Terai H, Yamada K, Suzuki A, Dohzono S, Matsumoto T, Nakamura H. Prevalence of Diffuse Idiopathic Skeletal Hyperostosis in Patients with Spinal Disorders. Asian Spine J. 2017;11:63-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Diaremes P, Braun S, Meurer A. [Scheuermann's disease]. Orthopade. 2022;51:339-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Dziewulski M, Szymanik W. Epidemiology of Scheuermann's disease in children and adolescents. Ortop Traumatol Rehabil. 2002;4:752-757. [PubMed] |
| 14. | Demiroz S, Ketenci IE, Yanik HS, Bayram S, Ur K, Erdem S. Intraspinal Anomalies in Individuals with Scheuermann's Kyphosis: Is the Routine Use of Magnetic Resonance Imaging Necessary for Preoperative Evaluation? Asian Spine J. 2018;12:697-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Guo JJ, Luk KD, Karppinen J, Yang H, Cheung KM. Prevalence, distribution, and morphology of ossification of the ligamentum flavum: a population study of one thousand seven hundred thirty-six magnetic resonance imaging scans. Spine (Phila Pa 1976). 2010;35:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 16. | Feng FB, Sun CG, Chen ZQ. Progress on clinical characteristics and identification of location of thoracic ossification of the ligamentum flavum. Orthop Surg. 2015;7:87-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Dützmann S, Fernandez R, Rosenthal D. [Thoracic spinal stenosis: Etiology, pathogenesis, and treatment]. Orthopade. 2019;48:844-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |