Published online Jan 26, 2023. doi: 10.12998/wjcc.v11.i3.598
Peer-review started: October 30, 2022
First decision: December 13, 2022
Revised: December 22, 2022
Accepted: January 5, 2023
Article in press: January 5, 2023
Published online: January 26, 2023
Processing time: 87 Days and 23.6 Hours
The inferior vena cava filter is utilized worldwide to intercept thrombi and to reduce the risk of fatal pulmonary embolism (PE). However, filter-related thrombosis is a complication of filter implantation. Endovascular methods such as AngioJet rheolytic thrombectomy (ART) and catheter-directed thrombolysis (CDT) can treat filter-related caval thrombosis, but the clinical outcomes of both treatment modalities have not been determined.
To compare the treatment outcomes of AngioJet rheolytic thrombectomy vs catheter-directed thrombolysis in patients with filter-related caval thrombosis.
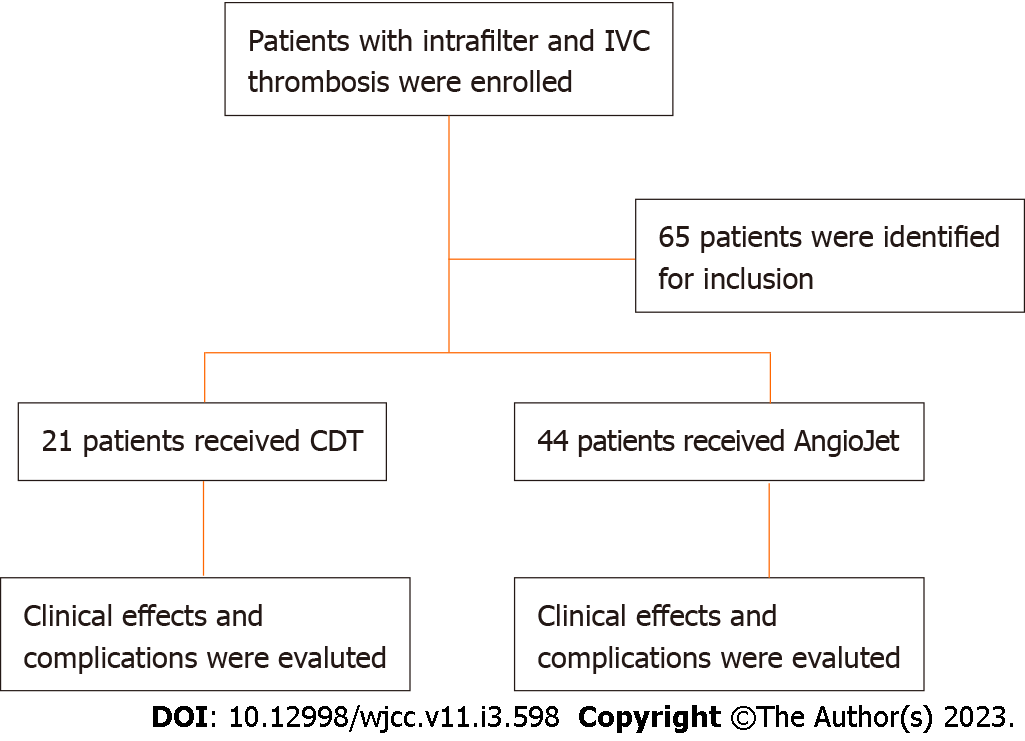
In this single-center retrospective study, 65 patients (34 males and 31 females; mean age: 59.0 ± 13.43 years) with intrafilter and inferior vena cava thrombosis were enrolled between January 2021 and August 2022. These patients were assigned to either the AngioJet group (n = 44) or the CDT group (n = 21). Clinical data and imaging information were collected. Evaluation measures included thrombus clearance rate, periprocedural complications, urokinase dosage, incidence of PE, limb circumference difference, length of stay, and filter removal rate.
Technical success rates were 100% in the AngioJet and CDT groups. In the AngioJet group, grade II and grade III thrombus clearance was achieved in 26 (59.09%) and 14 (31.82%) patients, respectively. In the CDT group, grade II and grade III thrombus clearance was accomplished in 11 (52.38%) patients and 8 (38.10%) patients, respectively (P > 0.05).The peridiameter difference of the thigh was significantly reduced in patients from both groups after treatment (P < 0.05). The median dosage of urokinase was 0.08 (0.02, 0.25) million U in the AngioJet group and 1.50 (1.17, 1.83) million U in the CDT group (P < 0.05). Minor bleeding was shown in 4 (19.05%) patients in the CDT group, and when it was compared with that in the AngioJet group, the difference was statistically significant (P < 0.05). No major bleeding occurred. Seven (15.91%) patients in the AngioJet group had hemoglobinuria and 1 (4.76%) patient in the CDT group had bacteremia. There were 8 (18.18%) patients with PE in the AngioJet group and 4 (19.05%) patients in the CDT group before the intervention (P > 0.05). Computed tomography angiopulmonography (CTA) showed that PE was resolved after the intervention. New PE occurred in 4 (9.09%) patients in the AngioJet group and in 2 (9.52%) patients in the CDT group after theintervention (P > 0.05). These cases of PE were asymptomatic. The mean length of stay was longer in the CDT group (11.67 ± 5.34 d) than in the AngioJet group (10.64 ± 3.52 d) (P < 0.05). The filter was successfully retrieved in the first phase in 10 (47.62%) patients in the CDT group and in 15 (34.09%) patients in the AngioJet group (P > 0.05).Cumulative removal was accomplished in 17 (80.95%) out of 21 patients in the CDT group and in 42 (95.45%) out of 44 patients in the ART group (P > 0.05). The median indwelling time for patients with successful retrieval was 16 (13139) d in the CDT group and 59 (12231) d in the ART group (P > 0.05).
Compared with catheter-directed thrombolysis, AngioJet rheolytic thrombectomy can achieve similar thrombus clearance effects, improve the filter retrieval rate, reduce the urokinase dosage and lower the risk of bleeding events in patients with filter-related caval thrombosis.
Core Tip: This is a retrospective study. A total of 65 patients were enrolled to evaluate the clinical outcomes of different treatment methods in patients with filter-related caval thrombosis. We compared the data of patients between the AngioJet rheolytic thrombectomy group (n = 44) and the catheter-directed thrombolysis group (n = 21). The current results showed no difference in thrombus clearance or filter retrieval rate. However, the results showed significant differences in urokinase dosage, peridiameter difference of the thigh, minor bleeding, and length of stay.
- Citation: Li JY, Liu JL, Tian X, Jia W, Jiang P, Cheng ZY, Zhang YX, Liu X, Zhou M. Clinical outcomes of AngioJet pharmacomechanical thrombectomy versus catheter-directed thrombolysis for the treatment of filter-related caval thrombosis. World J Clin Cases 2023; 11(3): 598-609
- URL: https://www.wjgnet.com/2307-8960/full/v11/i3/598.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i3.598
Patients with deep venous thrombosis (DVT) have a high risk of lethal acute pulmonary embolism (PE) if left untreated[1-3]. Anticoagulants are the mainstay of prophylaxis in DVT[4,5]. At present, inferior vena cava (IVC) filters are used to reduce the risk of fatal PE in high-risk patients[6,7]. However, permanent placement of IVC filters may lead to some complications, such as fracture or migration, organ injury, and thrombotic events[8-10]. The incidence of filter-related caval thrombosis ranges from 1% to 30%, depending on the type of filter[11-13]. Filter-related thrombosis can cause caval occlusion associated with some complications, including renal dysfunction and pelvic congestion syndrome[14].
Therefore, early thrombus clearance is essential to restore the patency of the caval outflow. It is difficult to treat filter-related thrombosis because of the large vessel lumen and the large thrombus burden. The methods of thrombus clearanceinclude open surgical thrombectomy, catheter-directed thrombolysis (CDT), and percutaneous mechanical thrombectomy (PMT)[15]. Open surgical thrombectomy ensures satisfactory long-term clinical outcomes for patients who are not eligible for endovascular measures[16]. Although CDT is an effective treatment for filter-related caval thrombosis that can restore blood flow, it increases the risk of bleeding events[13,14,17]. PMT is effective for resolving filter-related caval thrombosis, reducing the dosage of thrombolytic drugs and the risk of bleeding events[18].
A meta-analysis recently reported the treatment outcomes of AngioJet vs CDT for lower extremity deep venous thrombosis (LEDVT)[19]. Based on our clinical experience, PMT can reduce the risk of bleeding and may be a good option. What's more, it is unclear whether CDT and PMT lead to major bleeding or fatal PE in patients with filter-related caval thrombosis. However, the clinical outcomes of both treatment modalities have not been determined in these patients until now. Therefore, we aimed to compare ART with CDT in patients with filter-related thrombosis on treatment outcomes for providing a basis for clinical practice and research.
This is a single-center retrospective study. Patients with traumatic lower-limb fractures and simultaneous DVT who were admitted to Beijing Jishuitan Hospital between January 2021 and August 2022 were enrolled in the present study. The presence of DVT was confirmed with bilateral color Doppler ultrasound or venography. These patients received an IVC filter before surgical fixation. The IVC filter was deployed in all patients using the standard technique, and the femoral vein of the healthy limb was used as the access site for filter placement. Filter removal was attempted within 2 wk after fracture surgery in all patients, and venography revealed intrafilter and IVC thrombosis. Sixty-five patients (59.0 years ± 13.43 years) were identified for inclusion in the study. General patient information data, including sex, age, affected limbs, risk factors (fracture types), scope of thrombosis, filter types, and duration of symptoms (defined as the time from detection oflower extremity DVT to thrombus clearance), were collected (Table 1). This study received ethical approval from the Ethics Committee of our hospital.
| CDT group (n = 21) | AngioJet group (n = 44) | χ2/t | P values | |
| Age (yr old) | 55.24 ± 11.92 | 56.84 ± 14.19 | -0.447 | 0.656 |
| Male | 13 (61.90) | 21 (47.73) | 1.145 | 0.285 |
| Affected limbs (left) | 10 (47.62) | 20 (45.54) | 0.027 | 0.87 |
| Duration of symptoms | 11.23 ± 2.17 | 11.59 ± 2.08 | -0.63 | 0.531 |
| Risk factors (fracture types) | ||||
| Below the knee | 6 (28.57) | 8 (18.18) | 0.913 | 0.657 |
| Knee | 6 (28.57) | 14 (31.82) | ||
| Above the knee | 9 (42.86) | 22 (50.0) | ||
| Scope of thrombosis | ||||
| Femoral/popliteal/calf | 5 (23.81) | 6 (13.64) | 0.448 | 0.503 |
| Popliteal/calf | 16 (76.19) | 38 (86.36) | ||
| Filter types | ||||
| Denali | 22 (100.0) | 41 (93.18) | – | 0.545 |
The inclusion criteria were as follows: (1) Unilateral lower extremity fracture and simultaneous DVT (femoral and/or popliteal venous thrombosis) in the acute stage; (2) complete medical records; (4) life expectancy > 1 year; (5) no serious complications of vital organs; (6) no anticoagulant or thrombolysis contraindication after surgical fixation of fractures; and (7) no previous history of thrombosis.
The exclusion criteria were as follows: (1) Bilateral lower extremity DVT; (2) thrombosis throughout the iliofemoral vein; (3) history of pregnancy or any hemorrhage; (4) life expectancy < 1 year; and (5) contraindications related therapeutic drugs.
These patients were assigned to either the AngioJet group (n = 44) or the CDT group (n = 21). The study profile was shown in Figure 1. Evaluation measures included thrombus clearance rate, periprocedural complications, urokinase dosage, incidence of PE, limb circumference difference, length of stay, and filter removal rate. The procedure of intervention was as follows (Table 2).
| CDT group (n = 21) | AngioJet group (n = 44) | χ2/t | P values | |
| Scope of thrombosis | ||||
| intra-filter thrombosis | 18 (85.71) | 38 (86.36) | 0 | 1 |
| intra-filter and IVC thrombosis | 3 (14.29) | 6 (13.64) | ||
| Pulmonary embolism | 4 (19.05) | 8 (18.18) | 0 | 1 |
| Left lung | 2 (9.52) | 3 (6.82) | – | 0.655 |
| Embolism of lobar artery | 1 (4.76) | 2 (0.45) | – | 1 |
| Embolism of segmental artery | 3 (14.29) | 6 (13.64) | 0 | 1 |
| Median urokinase dosage (million U, range) | 1.50 (1.17, 1.83) | 0.08 (0.02, 0.25) | -6.495 | 0 |
| Large-lumen catheter aspiration thrombus | 11 (52.38) | 33 (75.0) | 3.326 | 0.068 |
| D-Dimer (before intervention) | 12.10 (2.29, 30.93)a | 8.87 (2.01, 18.88)b | -4.472 | 0 |
| D-Dimer (after intervention) | 8.37 (2.67, 15.98)a | 7.14 (0.43, 22.05)b | -3.407 | 0.001 |
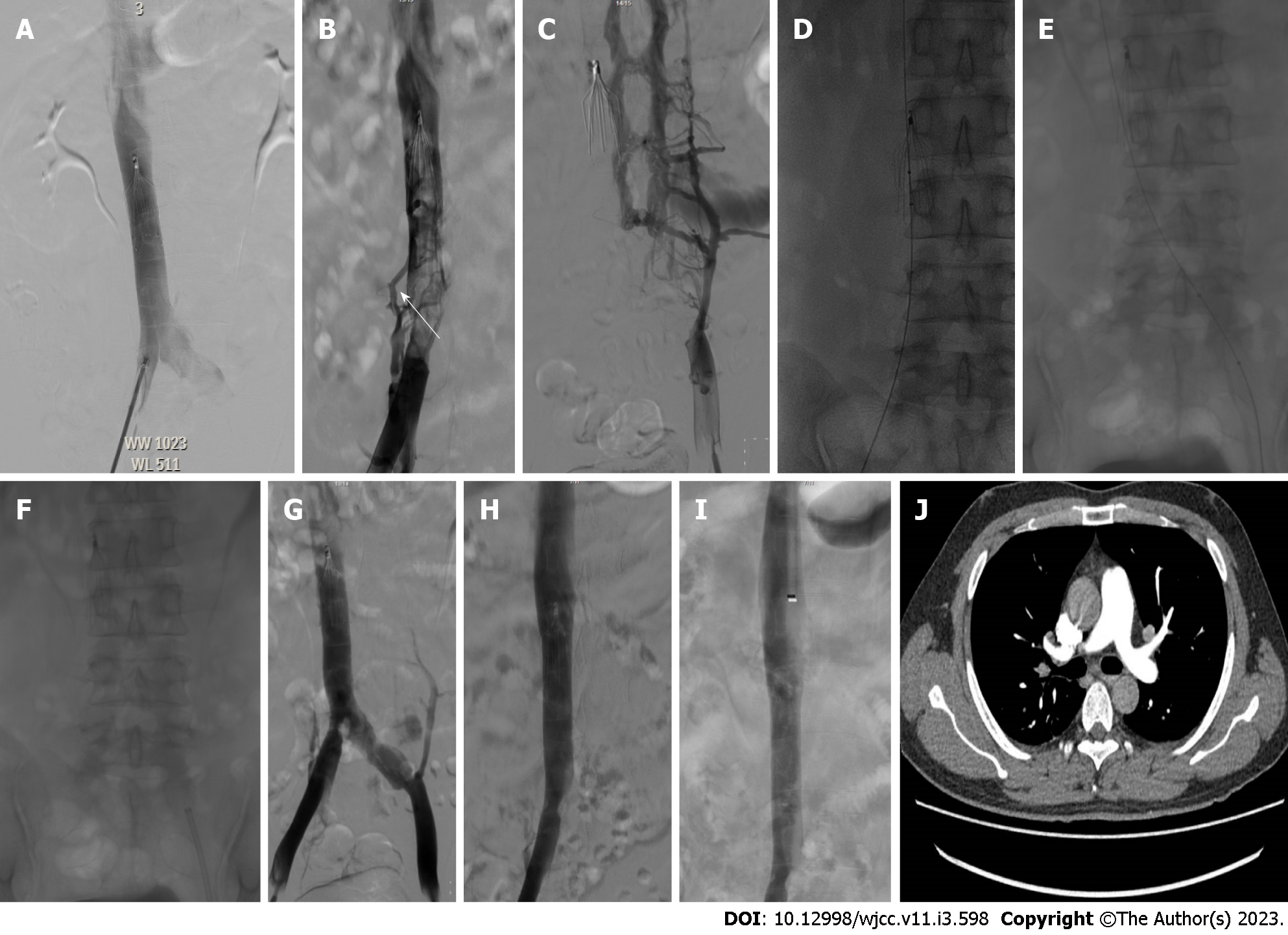
A 6-Fr AngioJet thrombectomy catheter (Boston Scientific, Natick, MA, United States) was inserted into the IVC thrombus via the femoral vein. The power-pulsed spraying thrombolytic mode was used, and saline-containing urokinase (100 mL of normal saline + 200000 U of urokinase) was injected into the IVC thrombus at a speed of 1 mm/s. The dosage of normal saline-containing urokinase depended on the extent of the thrombus. After waiting for 15-20 min, a mechanical rheolytic thrombectomy was performed for aspiration of the thrombus. If the thrombus remained, we repeated the aspiration 2-3 times. If the inferior vena cava angiography showed that the thrombus remained, a 10F guiding catheter (OptEaseTM Retrieval Catheter, Cordis Corporation, FL, United States) was used to suck the thrombus out under guidance of an exchange guidewire (Terumo, Japan) via femoral vein access. The catheter connected a 20 mL injector, and constant negative pressure of the syringe was maintained for repeated thrombus suction. Finally, inferior vena cava angiography was implemented to assess thrombus clearance (Figure 2).
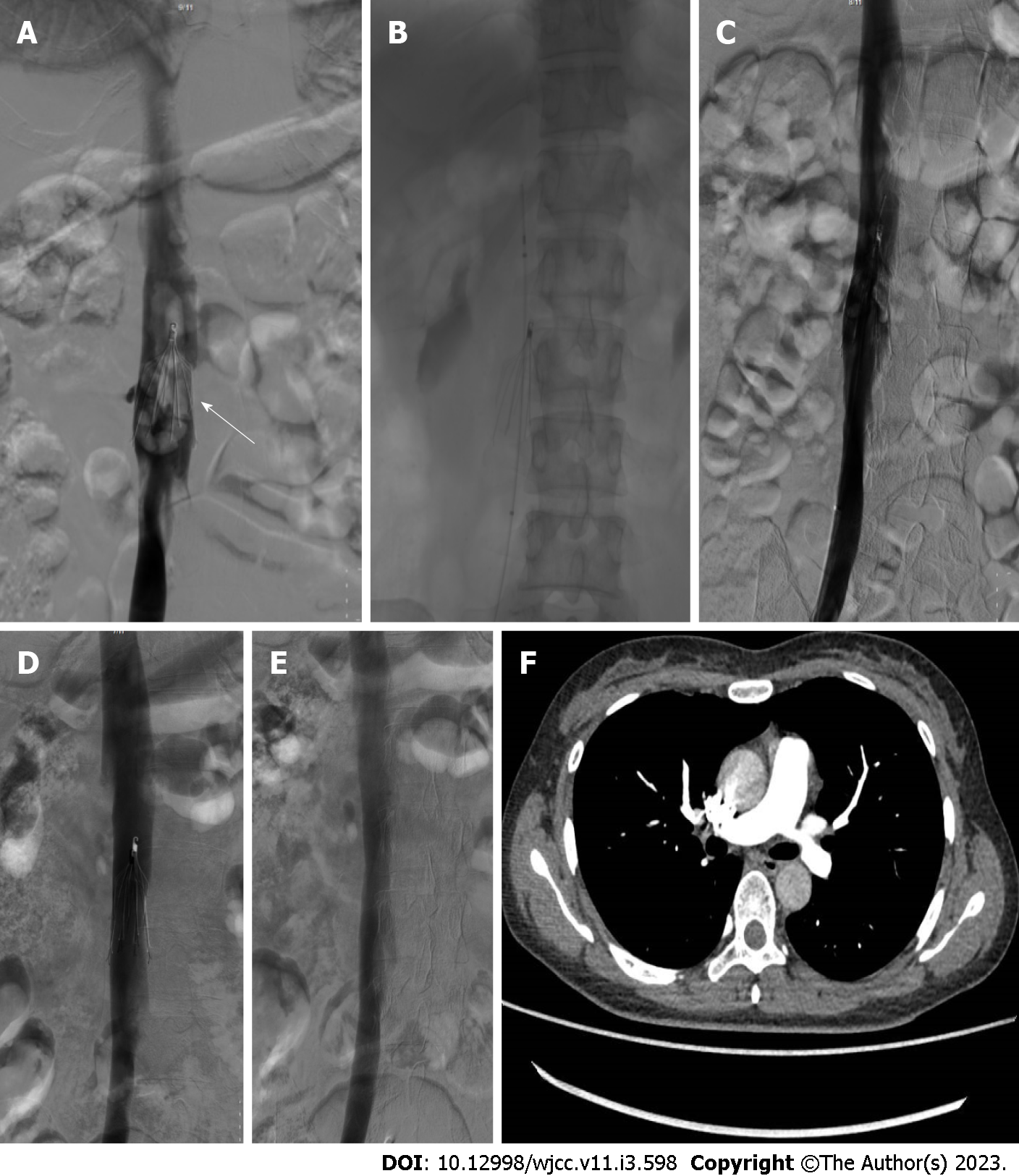
We placed a thrombolytic catheter (UniFuse, AngioDynamics, Latham, NY, United States) in the thrombus via the femoral vein. Urokinase was constantly injected through the catheter at a rate of 500000 U/d. Angiography was implemented every 24 h to evaluate the thrombolytic effect (Figure 3). Thrombolysis was terminated when the plasma fibrinogen level was less than 1 g/L, the IVC was unobstructed, or there were serious complications. If the inferior vena cava angiography showed that the thrombus remained, a 10F guiding catheter was used to suck the thrombus out under the guidance of an exchange guidewire (Terumo, Japan) via femoral vein access. The catheter connected to a 20 mL injector was maintained for repeated thrombus suction. Eventually, inferior vena cava angiography was performed to evaluate the thrombus clearance effect.
Filter retrieval was performed when the patient was considered low risk for PE. The criteria were as follows: (1) Decreasing trend or normal serum D-dimer levels; (2) IVC thrombus clearance of more than 95% after ART or CDT; and (3) disappearance or organization of the previously visualized lower-limb thrombus. The same placement technique as before was applied for venous access for the filter retrieval procedures. All procedures were performed through the femoral vein. Briefly, after venous access and the introduction of the angiography catheter, initial venography was performed to evaluate the patency of the IVC. The filter was retrieved using the Günther Tulip Retrieval System (William Cook Europe, Denmark). If the above conditions were not met, anticoagulation therapy was continued, ultrasound or venography was further assessed for the associated risks, and filter removal was performed at an optional stage.
During hospitalization, low molecular weight heparin was routinely given after fracture surgery, and anticoagulation therapy with 20 mg rivaroxaban was initiated daily after thrombus clearance. Oral anticoagulant was taken for at least 3 mo after filter removal.
Technical success is defined as uncomplicated implementation of the AngioJet device or CDT for thrombectomy through femoral vein access. CTA and D-dimer tests were performed before and after the operation within 3 d. D-dimer was analyzed with a Sysmex CS-5100 System. The laboratory reference range was 0 to 0.55 mg/mL. The difference in circumference between the affected and unaffected thighs at 15 cm above the patella was measured before and after treatment. The thrombus clearance effect was assessed according to the outcomes of the first and last venography. The degree of thrombus clearance was divided into three types: Grade I (partial clearance (< 50%), grade II (most clearance (50%-99%), and grade III (complete clearance (100%)[20]. The occurrence of complications was evaluated, including minor bleeding (epistaxis, gum bleeding, and hematoma), major bleeding (retroperitoneal or intracranial bleeding), hemoglobinuria, bacteremia, allergic reaction, serious cardiovascular or respiratory complications, and death. Filter removal of the first phase was defined as immediate retrieval within 3 d after thrombus removal. After anticoagulation and thrombus clearance, all filters were removed, and the cumulative removal rate was calculated by the proportion of successful filter retrieval. The indwelling time of the filter was the time from placement to retrieval. The follow-up time was more than one month, and patients also underwent routine D-dimer tests every month after discharge.
Continuous variables are presented as medians, minimums, and maximums for nonparametric distributions and were compared by using the Mann-Whitney test. Continuous variables are presented as the means and standard deviations for parametric distributions, and comparisons were made using the independent t test. Categorical variables are evaluated as frequencies and percentages and compared by using the chi-square test or Fisher’s exact test. Statistical significance was defined as P < 0.05. All statistical analyses were processed with SPSS 23.0 software (SPSS Inc., Chicago, IL, United States).
Sixty-five (65) patients diagnosed with traumatic lower-limb fracture and simultaneous DVT between January 2021 and August 2022 were enrolled in the study. Forty-four patients (56.84 ± 14.19 years) were included in the AngioJet group, and 21 patients (55.24 ± 11.92 years) were included in the CDT group. The left lower extremity was affected in 10 patients (47.76%) in the CDT group and in 20 patients (45.54%) in the ART group (P > 0.05). Risk factors associated with acute DVT in the two groups were fractures below the knee (28.57% vs 18.18%, P > 0.05), fractures of the knee (28.57% vs 31.82%, P > 0.05), and fractures above the knee (42.86% vs 50.0%, P > 0.05). The scope of thrombosis in both groups included the femoral/popliteal/calf vein (23.81% vs 13.64%, P > 0.05) and popliteal/calf vein (76.19% vs 86.36%, P > 0.05). Filters of Denali were implanted in 22 patients in the CDT group and 44 in the ART group (100% vs 93.18%, P > 0.05). The general information is shown in Table 1.
The scope of thrombosis in both groups included intrafilter thrombosis (85.71% vs 86.36%, P > 0.05) and intrafilter and IVC thrombosis (14.29% vs 13.64%, P > 0.05). There were 8 (18.18%) patients with PE in the AngioJet group and 4 (19.05%) patients in the CDT group before the intervention (P > 0.05). CTA showed that these cases of PE were resolved after the intervention. The PE was located at the level of segmental or lobar arteries in these patients (P > 0.05). The median dosage of urokinase was 0.08 (0.02, 0.25) million U in the AngioJet group and 1.50 (1.17, 1.83) million U in the CDT group (P < 0.05). Compared to 33 (75.0%) patients in the AngioJet group, 11 (52.38%) patients in the CDT group were treated with large-lumen catheter suction after thrombus clearance (P > 0.05). In the CDT group, the median D-dimer levels were 12.10 (2.29, 30.93) and 8.37 (2.67, 15.98) mg/mL before and after treatment, respectively (P < 0.05). In the AngioJet group, the median D-dimer levels were 8.87 (2.01, 18.88) and 7.14 (0.43, 22.05) mg/mL before and after treatment, respectively (P < 0.05) (Table 2).
The technical success rates were 100% in the AngioJet and CDT groups. Thrombus clearance of patients in the CDT and AngioJet groups reached grade I (9.52% vs 9.09%), grade II (52.38% vs 59.09%), and grade III (38.10% vs 31.82%), respectively (P > 0.05). In the AngioJet group, the differences in thigh circumference were 4.76 ± 0.77 cm and 1.58 ± 0.51 cm before and after treatment, respectively (P < 0.05). In the CDT group, the peridiameter differences of the thigh were 4.51 ± 0.65 cm and 1.44 ± 0.36 cm, respectively (P < 0.05).
In the AngioJet group, 7 patients (15.91) developed hemoglobinuria after the procedure, which was relieved after rehydration and hydration, and no hemoglobinuria was found in the CDT group. Bacteremia was found in one patient (4.76%) in the CDT group, which was relieved by anti-infection after catheter removal. In the CDT group, minor bleeding was observed in 4 (19.05%) patients, including epistaxis in 2 patients, gum bleeding in one patient, and hematoma at the puncture site in one patient, and the difference was significant compared with the AngioJet group (P < 0.05). New PE occurred in 4 patients (9.09) in the AngioJet group and in 2 patients (9.52) in the CDT group and was asymptomatic in each case. These PEs were located at the level of segmental arteries in these patients (P > 0.05). The mean length of stay was longer in the CDT group (11.67 ± 5.34 d) than in the AngioJet group (10.64 ± 3.52 d) (P < 0.05).
Immediate filter retrieval was successful in 10 out of 21 patients (47.62% success rate) after the procedure in the CDT group and 15 out of 44 patients (34.09% success rate) in the ART group (P > 0.05). Cumulative removal was achieved in 17 (80.95% success rate) out of 21 patients in the CDT group and 42 (95.45% success rate) out of 44 patients in the AngioJet group (P > 0.05). Filter retrieval was unsuccessful in one patient due to superior vena cava malformation and was not conducted in 3 CDT patients due to organized thrombus, which prevented the capture of the retrieval hook, and in 2 AngioJet patients because of an organized thrombus on the hook. The median indwelling time for patients in whom retrieval was successful was 16 d (range 13-139 d) in the CDT group and 59 d (range 12-231 d) in the ART group (P > 0.05). The therapeutic effects and complications are shown in Table 3.
| CDT group (n = 21) | AngioJet group (n = 44) | χ2/t | P values | |
| Thrombus clearance grade | ||||
| Grade I (< 50%) | 2 (9.52) | 4 (9.09) | 0.281 | 0.922 |
| Grade II (50%-99%) | 11 (52.38) | 26 (59.09) | ||
| Grade III (100%) | 8 (38.10) | 14 (31.82) | ||
| Complications | ||||
| Haemoglobinuria | 0 | 7 (15.91) | – | 0.086 |
| Any bleed | 4 (19.05) | 0 | – | 0.009 |
| Bacteraemia | 1 (4.76) | 0 | – | 0.323 |
| PE after treatment | 2 (9.52) | 4 (9.09) | – | 1 |
| Left lung | 2 (9.52) | 0 | – | 0.101 |
| Embolism of segmental artery | 2 (9.52) | 4 (9.09) | – | 1 |
| Difference of circumference between affected and unaffected thigh (cm) | ||||
| Before treatment | 4.51 ± 0.65c | 4.76 ± 0.77d | -1.267 | 0.21 |
| After treatment | 1.44 ± 0.36d | 1.58 ± 0.51d | -1.089 | 0.28 |
| Length of stay (d) | 11.67 ± 5.34 | 10.64 ± 3.52 | 2.215 | 0.03 |
| Filter removal | ||||
| the first phase | 10 (47.62) | 15 (34.09) | 1.099 | 0.294 |
| the cumulative removal | 17 (80.95) | 42 (95.45) | – | 0.08 |
| IVCF retention time (d) | 16 (13, 139) | 59 (12, 231) | -0.991 | 0.322 |
| D-dimer after 1 mo (mg/L) | 0.24 (0.09, 2.15) | 0.26 (0.09, 2.62) | -4.346 | 0 |
The median follow-up time was 4(1,10) months. At the 1-mo follow-up, no major bleeding, symptomatic PE, recurrent thrombosis or other serious complications was observed after the procedure in either group. Two (4.5%) patients in the AngioJet group developed recurrent swelling of the affected limb 1 mo after the intervention. The ultrasound showed venous reflux of the lower extremities. There was no skin ulceration or pigmentation in the calf after treatment in either group.
A high incidence of DVT has been reported in trauma patients, especially those with lower-limb fractures. With transient trauma contraindicating anticoagulant use, temporary perioperative IVC filter placement is the best prophylactic option for these patients[12,21]. IVC filter placement, however, may lead to numerous complications[22]. Filter-related thrombosis is one of the complications after implantation, with an incidence of approximately 10% in these patients[12]. Moreover, filter-related thrombosis also causes serious complications, such as caval occlusion or shock[14,23]. Prompt treatment of thrombi and retrieval of IVC filters can reduce the risk of filter-related thrombosis. The more effective methods for treating acute IVC filter-related thrombosis are CDT or ART[18,24]. No relevant literature evaluating the clinical efficacy of the two methods has been found thus far.
In our study, endovascular intervention resulted in good clinical outcomes, with a high incidence of thrombus clearance in patients in both groups. Studies have shown that grade II/III thrombus clearance was achieved in 80%-91% of acute LEDVT patients who underwent ART and in 83%-97% of acute LEDVT patients who underwent CDT[20,25]. The results of this study show that the extent of thrombus clearance in patients with IVC thrombosis is similar to that of patients with LEDVT. However, there have also been studies reporting 100% clearance of grade II/III IVC thrombosis[18,26]. This is somewhat different from our study and may be related to the selection of patients, the time of thrombosis, and the choice of thrombolytic drugs. In our study, manual aspiration thrombectomy (MAT) was performed according to the effect of thrombus removal after the operation. MAT through a large vascular sheath and guiding catheter is an adjunctive procedure for thrombus removal. It is also a necessary and effective means of thrombus clearance because of the large lumen and thrombus burden of the IVC in the treatment of filter-related thrombosis. In one study, the researchers repeated that MAT could achieve more than 95% thrombus clearance, which was shown in venography in patients with acute iliofemoral DVT[27]. However, in another study, the researchers mentioned that MAT had a good thrombusclearance rate but was less effective than ART for the treatment of IVC filter-related thrombosis (74.13 ± 19.74% vs 84.58 ± 11.90%, P < 0.05)[18]. ART or CDT combined with MAT can achieve good clinical outcomes, but further studies are needed to confirm this hypothesis in the future.
CDT can rapidly achieve complete thrombolysis without pure anticoagulation but increases the potential risk of bleeding, which may be life-threatening[28]. It has been reported that the incidence of bleeding events in CDT ranges from 9.7% to 21.1% in patients with LEDVT[20,25-26]. Our study showed that the bleeding complication rate was 19.05%, which was similar to that of LEDVT, and no major bleeding events occurred. In addition to bleeding complications, the management of CDT is also a tricky problem, mainly reflected in the restriction of patient movement because of indwelling catheters, bleeding or hematoma, and catheter-related bacteremia. In this study, one patient (4.76%) in the CDT group developed postoperative catheter-related bacteremia, which was cured by antibiotic treatment. When catheter-related infection occurs, it is necessary to remove the catheter, which may affect thrombolytic treatment. Therefore, catheter-related bacteremia should be avoided. ART can quickly reduce the volume of thrombi, which can achieve better clinical outcomes for inferior vena cava-iliac vein thrombosis[29]. Transient hemoglobinuria is one of the common complications of ART, and studies have reported an incidence of 9.1%-19%[18,20]. ART lowers urokinase dosage but causes discomfort, such as chest tightness, during the procedure in patients with IVC thrombosis. If these conditions occur, the procedure should be stopped, and thrombus removal can be resumed when the symptoms are relieved.
Winters et al[30] found that the retrieval rate improved from 23% to 45% over the past five years. It was reported in another study that the retrieval rate of the filter increased from 6.9% to 22.1% in the past 5 years[31]. This indicates that the retrievable rate is still low. Because it is difficult to complete DVT treatment within a short retrieval window, one might lose the best chance of filter retrieval. Meanwhile, a large number of retrievable filters were converted to permanent filters due to capturing thrombi or displaced or tilted filters[32]. Therefore, it is very important to perform thrombus clearance for filter-related thrombosis, which can improve the removal rate of the filter. In our study, the cumulative filter removal rate was 80.95% in the CDT group and 95.45% in the ART group. In addition, it is necessary to choose a filter such as Denali with a long indwelling time and a high removal rate as much as possible[33].
Lindsey et al[34] reported that the incidence of trapped IVC filter thrombus was 38% in patients with symptomatic lower extremity DVT who underwent endovascular interventions. At present, the occurrence of PE due to thrombus clearance in patients with intrafilter and IVC thrombosis has not been clinically reported. In our study, the incidence of PE was approximately 9% after ART or CDT in these patients. These PEs were asymptomatic, located in the pulmonary segmental or lobar arteries and relieved with conservative anticoagulation. After oral rivaroxaban anticoagulation, the patient's D-dimer level nearly dropped to normal within one month. This suggests that adequate anticoagulation after thrombus clearance is essential.
There are still several limitations in this study. First, it is a single-center retrospective analysis, which makes it prone to patient selection bias and artificial judgment bias for thrombus removal. LEDVT is different from intrafilter and IVC thrombosis. Thrombus clearance assessment for LEDVT may not be appropriate for IVC thrombosis. In the future, it is necessary to explore objective methods for evaluating thrombus clearance. Second, the sample size of the study was limited. Third, due to the short follow-up period, PTS and venous insufficiency were not evaluated. At present, there is a lack of large-scale studies and long-term follow-up on the venous patency rate and incidence of PTS after IVC thrombosis removal.
In summary, we reported the advantages and disadvantages of the two surgical methods in the treatment of patients with filter-related thrombosis. Compared with catheter-directed thrombolysis, ART can attain similar thrombus clearance effects, improve the filter retrieval rate, reduce the dosage of thrombolytic drugs and lower the risk of bleeding. ART and CDT did not cause fatal symptomatic PE in these patients. Because CDT has a greater risk of bleeding, ART may be an alternative treatment for these patients. However, ART, CDT, MAT and conservative treatment with anticoagulants are effective treatments for patients with IVC thrombosis. Which method is more advantageous? Large-sample prospective trials are needed to further confirm the clinical outcome of these treatment modalities.
Filter-related thrombosis is a complication of filter implantation. Early thrombus removal is implemented to restore the patency of the caval outflow. AngioJet rheolytic thrombectomy (ART) and catheter-directed thrombolysis (CDT) are endovascular treatment methods for filter-related caval thrombosis, but the clinical outcomes of both treatment modalities have not been determined.
We have performed both CDT and ART for filter-related thrombosis at our center. To date, there are few studies comparing the clinical outcomes of the two surgical methods, and the results are expected to be reported.
The aim of this study is to compare the clinical outcomes of AngioJet rheolytic thrombectomy with those of catheter-directed thrombolysis in patients with filter-related caval thrombosis.
Sixty-five patients (34 males and 31 females; mean age: 59.0 ± 13.43 years) with intrafilter and inferior vena cava thrombosis were enrolled between January 2021 and August 2022. Of these, patients were divided into the AngioJet group (n = 44) and the CDT group (n = 21). Clinical data and imaging information were collected. Evaluation measures included thrombus clearance rate, periprocedural complications, urokinase dosage, incidence of PE, limb circumference difference, length of stay, and filter removal rate.
There was no significant difference in thrombus clearance between the two groups (P > 0.05). The peridiameter difference of the thigh was significantly reduced in the patients of both groups after treatment (P < 0.05). The median dosage of urokinase was significantly lower in the ART group (0.08 (0.02, 0.25) million U) than in the CDT group (1.50 (1.17, 1.83) million U) (P < 0.05). Minor bleeding was shown in 4 (19.05%) patients in the CDT group, and when it was compared with that in the AngioJet group, the difference was statistically significant (P < 0.05). There was no case of symptomatic PE after the procedure in either group. The mean length of stay was 11.67 ± 5.34 d in the CDT group and 10.64 ± 3.52 d in the AngioJet group (P < 0.05). Cumulative removal was accomplished in 17 (80.95%) out of 21 patients in the CDT group and in 42 (95.45%) out of 44 patients in the AngioJet group (P > 0.05).
Compared with catheter-directed thrombolysis, AngioJet rheolytic thrombectomy can achieve similar thrombus clearance effects, improve the filter retrieval rate, reduce the urokinase dosage and lower the risk of bleeding events in patients with filter-related caval thrombosis.
Further large, prospective clinical studies of the clinical outcomes of CDT and ART are needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Kharlamov AN, Netherlands; Shariati MBH, Iran S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Patel K, Fasanya A, Yadam S, Joshi AA, Singh AC, DuMont T. Pathogenesis and Epidemiology of Venous Thromboembolic Disease. Crit Care Nurs Q. 2017;40:191-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Melman WP, Ettema HB, Verheyen CC. Symptomatic venous thromboembolism after trauma surgery: a study on 56.884 procedures. Acta Orthop Belg. 2020;86:363-368. [PubMed] |
| 3. | Barrera LM, Perel P, Ker K, Cirocchi R, Farinella E, Morales Uribe CH. Thromboprophylaxis for trauma patients. Cochrane Database Syst Rev. 2013;CD008303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Madan S, Shah S, Dale P, Partovi S, Parikh SA. Use of novel oral anticoagulant agents in venous thromboembolism. Cardiovasc Diagn Ther. 2016;6:570-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S-e496S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2565] [Cited by in RCA: 2569] [Article Influence: 197.6] [Reference Citation Analysis (0)] |
| 6. | Charalel RA, Durack JC, Mao J, Ross JS, Meltzer AJ, Sedrakyan A. Statewide Inferior Vena Cava Filter Placement, Complications, and Retrievals: Epidemiology and Recent Trends. Med Care. 2018;56:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral FG, Huet Y, Simonneau G. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338:409-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1265] [Cited by in RCA: 1100] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 8. | Abudayyeh I, Takruri Y, Weiner JB. Heart block and cardiac embolization of fractured inferior vena cava filter. SAGE Open Med Case Rep. 2016;4:2050313X16686017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Shimizu T, Kubota K, Suzuki T, Matsumoto T, Shiraki T, Sakuraoka Y, Mori S, Iso Y, Kato M, Ishizuka M, Aoki T. A technique for taping inferior vena cava caudal to the duodenum: duodenal penetration by IVC filter strut after retroperitoneal lymph node dissection-usefulness of the mesenteric approach. Surg Case Rep. 2019;5:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Knavel EM, Woods MA, Kleedehn MG, Ozkan OS, Laeseke PF. Complex Inferior Vena Cava Filter Retrieval Complicated by Migration of Filter Fragment into the Aorta and Subsequent Distal Embolization. J Vasc Interv Radiol. 2016;27:1865-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | King RW, Wooster MD, Veeraswamy RK, Genovese EA. Contemporary rates of inferior vena cava filter thrombosis and risk factors. J Vasc Surg Venous Lymphat Disord. 2022;10:313-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Huang J, Kong J, Zhang X, Liu C, Zhao Z, Liu L, Xiao L, Han X. Risk factors for inferior vena cava filter thrombosis in traumatic fracture patients with deep venous thrombosis of lower extremity: A single-center experience. Vascular. 2022;17085381221128056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Patel SH, Patel R. Inferior vena cava filters for recurrent thrombosis: current evidence. Tex Heart Inst J. 2007;34:187-194. [PubMed] |
| 14. | Xiao L, Shen J, Tong JJ, Zhang Z, Mu XL, Yi ZJ, Bai S, Xu K. Transcatheter thrombolytic therapy for symptomatic thrombo-occlusion of inferior vena cava filter. Exp Ther Med. 2013;5:533-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Kakkos SK, Gohel M, Baekgaard N, Bauersachs R, Bellmunt-Montoya S, Black SA, Ten Cate-Hoek AJ, Elalamy I, Enzmann FK, Geroulakos G, Gottsäter A, Hunt BJ, Mansilha A, Nicolaides AN, Sandset PM, Stansby G; Esvs Guidelines Committee; de Borst GJ, Bastos Gonçalves F, Chakfé N, Hinchliffe R, Kolh P, Koncar I, Lindholt JS, Tulamo R, Twine CP, Vermassen F, Wanhainen A, Document Reviewers, De Maeseneer MG, Comerota AJ, Gloviczki P, Kruip MJHA, Monreal M, Prandoni P, Vega de Ceniga M. Editor's Choice - European Society for Vascular Surgery (ESVS) 2021 Clinical Practice Guidelines on the Management of Venous Thrombosis. Eur J Vasc Endovasc Surg. 2021;61:9-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 393] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 16. | Wagenhäuser MU, Dimopoulos C, Antakyali K, Meyer-Janiszewski YK, Mulorz J, Ibing W, Ertas N, Spin JM, Schelzig H, Duran M. Clinical outcomes after direct and indirect surgical venous thrombectomy for inferior vena cava thrombosis. J Vasc Surg Venous Lymphat Disord. 2019;7:333-343.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Baekgaard N, Broholm R, Just S, Jørgensen M, Jensen LP. Long-term results using catheter-directed thrombolysis in 103 Lower limbs with acute iliofemoral venous thrombosis. Eur J Vasc Endovasc Surg. 2010;39:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Liu Z, Fu G, Gong M, Zhao B, Gu J, Wang T, Zhou Y, He X, Kong J. AngioJet Rheolytic Thrombectomy to Treat Inferior Vena Cava Filter-Related Thrombosis: Efficacy and Safety Compared With Large-Lumen Catheter Suction. Front Cardiovasc Med. 2022;9:837455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Li GQ, Wang L, Zhang XC. AngioJet Thrombectomy Versus Catheter-Directed Thrombolysis for Lower Extremity Deep Vein Thrombosis: A Meta-Analysis of Clinical Trials. Clin Appl Thromb Hemost. 2021;27:10760296211005548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 20. | Zhu J, Ni CF, Dai ZY, Yao LZ, Li WH. A case-controlled study on AngioJet rheolytic thrombectomy and catheter-directed thrombolysis in the treatment of acute lower extremity deep venous thrombosis. Vascular. 2020;28:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Jia W, Liu J, Tian X, Jiang P. Tempofilter II implantation in patients with lower extremity fractures and proximal deep vein thrombosis. Diagn Interv Radiol. 2014;20:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Grewal S, Chamarthy MR, Kalva SP. Complications of inferior vena cava filters. Cardiovasc Diagn Ther. 2016;6:632-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 23. | Higashi H, Yoshii T, Inaba S, Morofuji T, Morioka H, Saito M, Sumimoto T. Life-threatening shock due to inferior vena cava filter thrombosis. Heart Lung Vessel. 2015;7:263-265. [PubMed] |
| 24. | Li WD, Li CL, Qian AM, Zhang YQ, Li XQ. Catheter-directed thrombolysis combined with manual aspiration thrombectomy for acute inferior vena cava filter thrombosis. Int Angiol. 2016;35:605-612. [PubMed] |
| 25. | Xu Y, Wang X, Shang D, Liu J, Chen W, Han X. Outcome of AngioJet mechanical thrombus aspiration in the treatment of acute lower extremities deep venous thrombosis. Vascular. 2021;29:415-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Shi W, Lou W, He X, Liu C, Gu J. The management of filter-related caval thrombosis complicated by heparin-induced thrombocytopenia and thrombosis. Int J Clin Exp Med. 2015;8:13078-13088. [PubMed] |
| 27. | Zhu QH, Zhou CY, Chen Y, Wang J, Mo HY, Luo MH, Huang W, Yu XF. Percutaneous manual aspiration thrombectomy followed by stenting for iliac vein compression syndrome with secondary acute isolated iliofemoral deep vein thrombosis: a prospective study of single-session endovascular protocol. Eur J Vasc Endovasc Surg. 2014;47:68-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Amin VB, Lookstein RA. Catheter-directed interventions for acute iliocaval deep vein thrombosis. Tech Vasc Interv Radiol. 2014;17:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Huang CY, Hsu HL, Kuo TT, Lee CY, Hsu CP. Percutaneous pharmacomechanical thrombectomy offers lower risk of post-thrombotic syndrome than catheter-directed thrombolysis in patients with acute deep vein thrombosis of the lower limb. Ann Vasc Surg. 2015;29:995-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Winters JP, Morris CS, Holmes CE, Lewis P, Bhave AD, Najarian KE, Shields JT, Charash W, Cushman M. A multidisciplinary quality improvement program increases the inferior vena cava filter retrieval rate. Vasc Med. 2017;22:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Ahmed O, Wadhwa V, Patel K, Patel MV, Turba UC, Arslan B. Rising Retrieval Rates of Inferior Vena Cava Filters in the United States: Insights From the 2012 to 2016 Summary Medicare Claims Data. J Am Coll Radiol. 2018;15:1553-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 32. | Ho KM, Tan JA, Burrell M, Rao S, Misur P. Venous thrombotic, thromboembolic, and mechanical complications after retrievable inferior vena cava filters for major trauma. Br J Anaesth. 2015;114:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | Stavropoulos SW, Chen JX, Sing RF, Elmasri F, Silver MJ, Powell A, Lynch FC, Abdel Aal AK, Lansky A, Muhs BE; DENALI Trial Investigators. Analysis of the Final DENALI Trial Data: A Prospective, Multicenter Study of the Denali Inferior Vena Cava Filter. J Vasc Interv Radiol. 2016;27:1531-1538.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Lindsey P, Echeverria A, Poi MJ, Matos J, Bechara CF, Cheung M, Lin PH. Thromboembolic Risk of Endovascular Intervention for Lower Extremity Deep Venous Thrombosis. Ann Vasc Surg. 2018;49:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |