Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7221
Peer-review started: August 8, 2023
First decision: August 30, 2023
Revised: September 11, 2023
Accepted: September 18, 2023
Article in press: September 18, 2023
Published online: October 16, 2023
Processing time: 66 Days and 8.7 Hours
Ectopic pancreas may be unfamiliar to many people because it is rare and difficult to diagnose. However, this disease is highly susceptible to misdiagnosis and missed diagnosis. In this article, we report two cases of pancreatic heterotopia in the gastric sinus and small intestine, respectively, both of which were confirmed by histopathological examination.
The first patient was a 43-year-old female which reported abdominal distension for 2 mo. The second was a 67-year-old female who experienced intermittent epigastric discomfort for 15 d. In both cases, there was no confirmed preoperative examination, and the postoperative pathology indicated the presence of ectopic pancreas.
The diagnosis of ectopic pancreas is difficult, and is often prone to misdiagnosis and the possibility of being overlooked. Various laboratory tests and imaging tests should be carefully evaluated before surgery to achieve early detection, early diagnosis and early treatment.
Core Tip: Ectopic pancreas is rare, is usually clinically asymptomatic, and lacks a specific clinical presentation. Therefore, ectopic pancreas is often missed and misdiagnosed in clinical practice. This article reports the diagnosis and treatment process of two cases of ectopic pancreas in our hospital, to increase awareness regarding the occurrence of ectopic pancreas and provide guidance for making the correct diagnosis in a timely manner.
- Citation: Zhang H, Zhao HY, Zhang FH, Liang W. Gastric and intestinal ectopic pancreas: Two case reports. World J Clin Cases 2023; 11(29): 7221-7226
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7221.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7221
Ectopic pancreas is a relatively rare congenital condition in which pancreatic tissue is detected outside its normal location that has no anatomical or vascular relationship to the normal pancreas[1]. Ectopic pancreas often lacks specific clinical symptoms and signs, and because there are no specific clinical manifestations or imaging signs, the correct diagnosis can only be determined, in most cases, by histopathological examination of a resected specimen[2-3]. Ectopic pancreas can occur at any part of the gastrointestinal tract, but it is mostly detected in the upper gastrointestinal tract, especially in the stomach, duodenum and jejunum[4]. It is most commonly found in the stomach (25%-38% of cases), followed by the duodenum (17%-36%) and jejunum (15%-22%)[4]. This condition is highly susceptible to misdiagnosis in clinical practice. In the present report, case 1 with gastric ectopic pancreas was misdiagnosed as gastrointestinal mesenchymal tumor. This case highlights the importance of thorough and meticulous assessment of digestive swellings by clinicians, and attention to their differential diagnosis. The main differential diagnoses of ectopic pancreas include gastrointestinal mesenchymal tumors, gastrointestinal autonomic tumors, gastric carcinoid tumors, lymphomas, and gastric cancer[5].
Case 1: A 43-year-old female who reported abdominal distension for 2 mo.
Case 2: A 67-year-old female who experienced intermittent epigastric discomfort for 15 d.
Case 1: The patient presented to our hospital 2 mo ago with abdominal distension of unknown cause, which worsened after eating, without abdominal pain or diarrhea.
Case 2: Fifteen days ago, the patient presented with epigastric dull pain of no apparent cause, intermittent in nature, not radiating to the back, unrelated to breathing or position change, and relieved by eating. Occasional black stools, no mucopurulent stools, dizziness and weakness were observed.
Case 1: Five years after previous endometrial cancer surgery, regular check-ups have shown no signs of recurrence.
Case 2: This patient was previously fit, with no special medical history.
The patients had no relevant personal or family history.
Physical examination of the patients’ heart and lungs was unremarkable. Abdominal examination showed no positive signs for general conditions.
Blood analysis, stool analysis, and serum tumor markers showed no significant abnormalities.
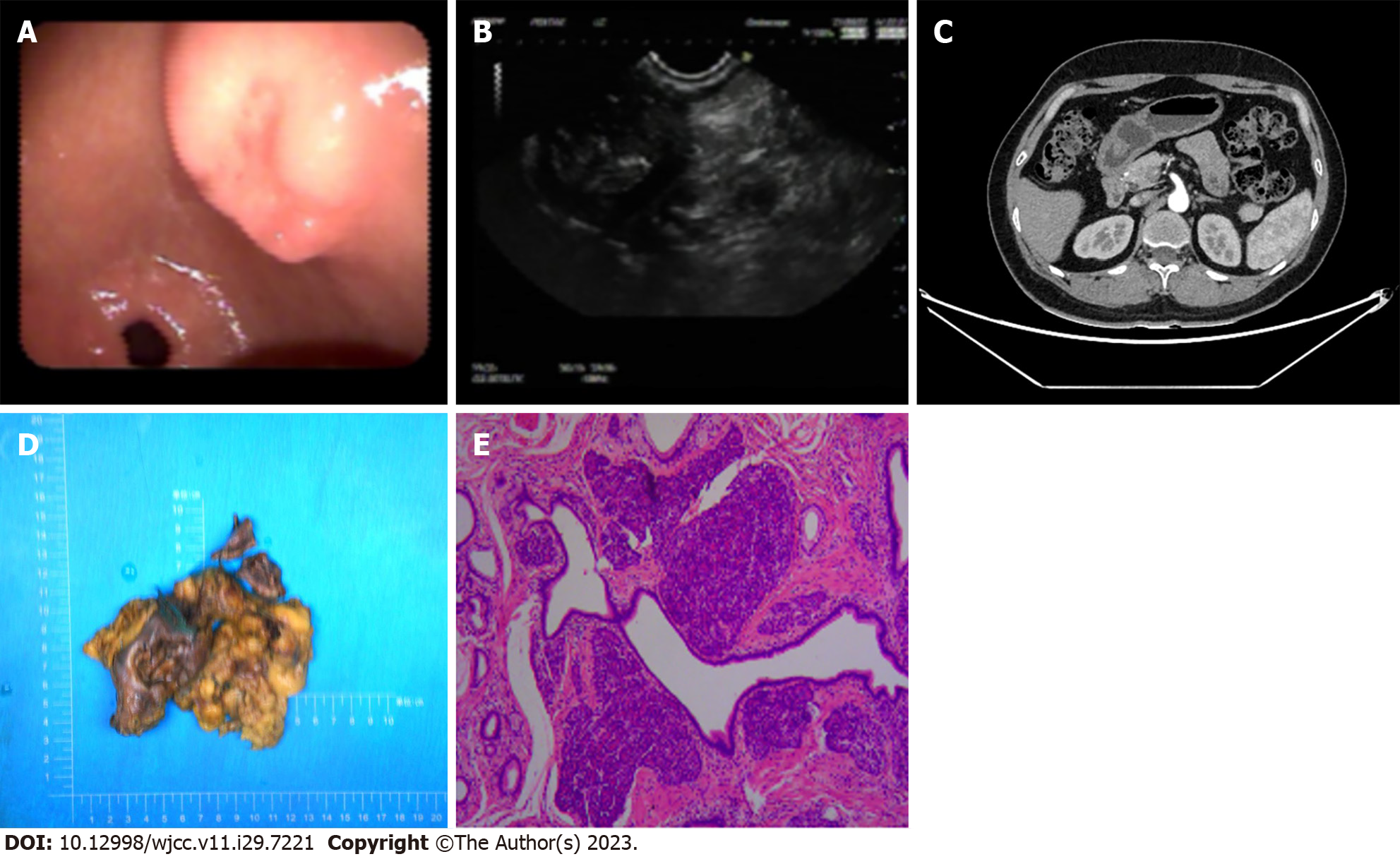
Case 1: Gastroscopic observation: A submucosal mass measuring approximately 3.0 cm × 2.2 cm was seen in the posterior wall of the gastric sinus, with smooth surface mucosa, central depression and rupture, and visible bridge-shaped folds (Figure 1A). Ultrasound gastroscopy observation: The lesion was located in the intrinsic muscular layer, and the internal echogenicity was heterogeneous and hypoechoic, approximately 3.0 cm × 2.4 cm in size, showing intra- and extra-cavernous growth with clear borders (Figure 1B). Microscopic diagnosis: A submucosal mass was detected in the gastric sinus, suggesting mesenchymal tumor. Computed tomography (CT) enhancement of the abdomen: The pancreas exhibited normal morphology and positioning, with a distinct contour. There were no signs of abnormal enhancement in the pancreatic tissue, and the pancreatic duct showed no dilation. Additionally, the peripancreatic fat gap was clearly visible (Figure 1C).
Case 2: Gastroscopy and pathology suggested: Gastric sinus cancer (type IIb).
During surgery: The mass was located on the lateral side of the greater curvature of the gastric sinus, with no invasion into the plasma layer, a diameter of approximately 3 cm, slightly tough, movable, and poorly defined. A laparoscopic wedge resection of the stomach was performed (Figure 1D). Postoperative pathological findings: (Distal stomach) dilated ducts and pancreatic vesicles were seen in the myxomucosa, submucosa, and superficial muscular layer, which was consistent with pancreatic ectopia (Figure 1E).
Case 1: The patient was diagnosed with (gastric sinus region) ectopic pancreas in the stomach.
Case 2: (1) Distal stomach: Gastric cancer; and (2) small intestinal mass (ectopic pancreas).
Case 1: Postoperatively, the patient recovered well.
Case 2: Postoperatively, the patient recovered well. Adjuvant XELOX chemotherapy regimen (oxaliplatin 240 mg as continuous intravenous infusion over 24 h on 1 d combined with capecitabine 1.5 g on 1-14 d) was administered as one cycle per 3 wk after surgery.
Case 1: The patient was discharged 8 d after surgery and has been followed up since.
Case 2: She was discharged from the hospital 11 d after surgery. As of the latest follow-up, her overall condition is satisfactory.
Currently, the pathogenesis of ectopic pancreas is unclear, and three main theories have been proposed to explain its occurrence, namely the mislocation theory, the chemotaxis theory, and the totipotent cell theory. The widely accepted mislocation theory suggests that during embryonic rotation, dorsal and ventral deposits of pancreatic tissue migrate and detach from the main body of the pancreas to different ectopic sites[6-8]. The chemotaxis theory suggests that during embryonic development, endodermal tissue migrates to the submucosa and then transforms into pancreatic tissue. The totipotent cell theory postulates that endodermal cells in the intestine differentiate into pancreatic tissue. Most patients with ectopic pancreas are asymptomatic[9], and preoperative diagnosis is often difficult, typically arising as an incidental discovery during surgery or autopsy[2-3]. It was reported that 0.2% of the cases were diagnosed during abdominal surgery and 0.55%-13.7% were diagnosed during autopsy and were mostly seen in men aged 30-50 years[10], with a male to female incidence ratio of approximately 3:1. However, the two patients in this report were women. Depending on the site of the lesion, some patients may present with nonspecific symptoms and complications such as abdominal pain, nausea, dysphagia, dyspepsia, bleeding and pancreatitis, gastric outlet obstruction or even malignant transformation[11,12]. Neither of the two patients in this report developed these complications. All pancreatic related diseases can also occur in ectopic pancreatic tissue[13]. A small percentage of patients may present with other symptoms, such as jaundice and biliary obstruction, perforation, fever, diarrhea, abscess, and carcinoid syndrome caused by jugular lesions[9].
Understanding and mastering the characteristic imaging manifestations of ectopic pancreas is the key to making a confirmatory diagnosis preoperatively. On imaging, ectopic pancreas is identified by a submucosal mass, presenting as an ill-defined lesion with an intraluminal growth pattern. A CT scan typically reveals enhancement similar to that of the normal pancreas, with surface depression and low attenuation within the lesion[14]. Additionally, a duct-like weakly enhancing shadow, known as the central duct sign, may be observed[15]. The typical endoscopic presentation is a well-defined submucosal lesion[16], and a depression formed at the edge of the lesion, known as the umbilical recess sign[15].
The reasons for the misdiagnosis and omission of the two cases in this report were analyzed. Firstly, the incidence of ectopic pancreas is low and relatively rare in clinical practice. Secondly, the small size of the ectopic pancreatic lesion makes the disease extremely easy to overlook. Both cases lacked specific clinical manifestations.
Most patients undergo surgical or endoscopic resection to relieve symptoms[9]. Therefore, patients with symptoms or complications are treated aggressively; however, the need for resection in those patients who are asymptomatic or whose symptoms have resolved remains controversial[17]. Studies have shown that local surgical resection can satisfactorily treat symptomatic patients who have failed to respond to pharmacological treatment, unless malignant transformation is present[10].
Benign neoplastic lesions caused by ectopic gastric pancreas are less common clinically, and carcinogenesis of ectopic glandular epithelium is even rarer[18]. In 1999, Makhlouf et al[19] reported that in 109 cases of gastrointestinal ectopic pancreas, the probability of malignancy was only 1.8%, and tumors were more common in the upper digestive tract.
Similar to the challenging diagnostic assessment of ectopic pancreas, evaluating the transplant donor poses a similar level of difficulty. In recent years, organ scarcity has led to the utilization of organs from individuals with a cancer history or newly discovered cancer during evaluation for transplantation. However, using organs from donors with a cancer history does come with a risk of cancer transmission. While this risk is extremely low, with reported incidences ranging from approximately 0.03% to 0.06%, the potential consequences can be severe. Although this risk can be reduced by careful assessment, it cannot be eliminated. The survival rate and prognosis of different types of tumors varies, with the prognosis of melanoma and neuroendocrine tumors reported to be the worst[20]. Thus, proper donor risk assessment is critical. The selection of donors should be carefully evaluated, with caution in the use of donor organs with a potentially high metastatic malignancy, while weighing up the risk factors for individual patients. Autopsy and timely pathology allows early detection of cancer and rapid transplantation, but it has a low pickup rate and not always accepted by families. Therefore, radiography should also be considered as a method for donor assessment[21]. At present, experts have suggested some effective methods, such as that of the Second Opinion in Italy. The timing of transplantation is equally important because organs must be transplanted as soon as possible to ensure the best possible results and the success of transplantation, enabling remote pathology systems and promoting the application of artificial intelligence[22].
In summary, clinicians and imaging experts aim to increase our understanding of ectopic pancreas, familiarize us with the typical imaging manifestations of ectopic pancreas, and identify a gastrointestinal space during endoscopy or biopsy, consider the possibility of ectopic pancreas, promote early detection and early diagnosis, and make a correct decision on whether to perform surgical intervention.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eccher A, Italy S-Editor: Qu XL L-Editor: Webster JR P-Editor: Yu HG
| 1. | Rezvani M, Menias C, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications. Radiographics. 2017;37:484-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 2. | Chen HL, Chang WH, Shih SC, Bair MJ, Lin SC. Changing pattern of ectopic pancreas: 22 years of experience in a medical center. J Formos Med Assoc. 2008;107:932-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Seneviratne SA, Ramanayaka IT, Samarasekera DN. Heterotopic pancreas in the body of the stomach. Ceylon Med J. 2009;54:57-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Christodoulidis G, Zacharoulis D, Barbanis S, Katsogridakis E, Hatzitheofilou K. Heterotopic pancreas in the stomach: a case report and literature review. World J Gastroenterol. 2007;13:6098-6100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in CrossRef: 107] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Liu X, Wu X, Tuo B, Wu H. Ectopic pancreas appearing as a giant gastric cyst mimicking gastric lymphangioma: a case report and a brief review. BMC Gastroenterol. 2021;21:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Chen HL, Lin SC, Chang WH, Yang TL, Chen YJ. Identification of ectopic pancreas in the ileum by capsule endoscopy. J Formos Med Assoc. 2007;106:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Monier A, Awad A, Szmigielski W, Muneer M, Alrashid A, Darweesh A, Hassan H. Heterotopic pancreas: a rare cause of ileo-ileal intussusception. Pol J Radiol. 2014;79:349-351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Trifan A, Târcoveanu E, Danciu M, Huţanaşu C, Cojocariu C, Stanciu C. Gastric heterotopic pancreas: an unusual case and review of the literature. J Gastrointestin Liver Dis. 2012;21:209-212. [PubMed] |
| 9. | LeCompte MT, Mason B, Robbins KJ, Yano M, Chatterjee D, Fields RC, Strasberg SM, Hawkins WG. Clinical classification of symptomatic heterotopic pancreas of the stomach and duodenum: A case series and systematic literature review. World J Gastroenterol. 2022;28:1455-1478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (2)] |
| 10. | Sheshe AA, Yusuf I. Ectopic Pancreas Causing Partial Gastric Outlet Obstruction: A Case Report and Review of Literature. Niger J Surg. 2018;24:56-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Bejiga G. Gastric outlet obstruction secondary to heterotopic pancreas being mistaken for gastric cancer: "Case report". Int J Surg Case Rep. 2022;93:106974. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Manhal K, Gaetan M, Thierry D, Baudouin M. A rare case of adenocarcinoma of an ectopic pancreas: A case report. Int J Surg Case Rep. 2022;94:107061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Betzler A, Mees ST, Pump J, Schölch S, Zimmermann C, Aust DE, Weitz J, Welsch T, Distler M. Clinical impact of duodenal pancreatic heterotopia - Is there a need for surgical treatment? BMC Surg. 2017;17:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Wei R, Wang QB, Chen QH, Liu JS, Zhang B. Upper gastrointestinal tract heterotopic pancreas: findings from CT and endoscopic imaging with histopathologic correlation. Clin Imaging. 2011;35:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Sun J, Yin LL. CT and MRI manifestations of ectopic pancreas in the gastrointestinal tract . Zhongguo Puwai Jichu Yu Linchuang Zazhi. 2019;26:1346-1349. |
| 16. | Jung HS, Lee J, Nam KH, Jeong SJ, Oh EH, Park YE, Park J, Kim TO. Gastric Adenocarcinoma Arising from Heterotopic Pancreas Presenting as Gastric Outlet Obstruction 10 Years after the First Diagnosis. Korean J Gastroenterol. 2020;76:37-41. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Rubel AR, Chong VH. Gastric Hematoma Secondary to Heterotopic Pancreas of the Stomach: Unexpected Cause of Upper Gastrointestinal Bleeding. Cureus. 2022;14:e26175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Noda E, Kuroda K, Sera T, Mori T, Kinoshita H, Hasegawa T, Teraoka H, Chikugo T. Intraductal papillary mucinous neoplasm originating from a heterotopic pancreas within the jejunum: a case report. J Surg Case Rep. 2018;2018:rjy181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Makhlouf HR, Almeida JL, Sobin LH. Carcinoma in jejunal pancreatic heterotopia. Arch Pathol Lab Med. 1999;123:707-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Eccher A, Girolami I, Marletta S, Brunelli M, Carraro A, Montin U, Boggi U, Mescoli C, Novelli L, Malvi D, Lombardini L, Cardillo M, Neil D, D'Errico A. Donor-Transmitted Cancers in Transplanted Livers: Analysis of Clinical Outcomes. Liver Transpl. 2021;27:55-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Ortiz JA, Manzarbeitia C, Noto KA, Rothstein KD, Araya VA, Munoz SJ, Reich DJ. Extended survival by urgent liver retransplantation after using a first graft with metastasis from initially unrecognized donor sarcoma. Am J Transplant. 2005;5:1559-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Eccher A, Malvi D, Novelli L, Mescoli C, D'Errico A. Second Opinion in the Italian Organ Procurement Transplantation: The Pathologist Is In. Clin Pract. 2023;13:610-615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |