Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7179
Peer-review started: July 28, 2023
First decision: August 30, 2023
Revised: September 14, 2023
Accepted: September 25, 2023
Article in press: September 25, 2023
Published online: October 16, 2023
Processing time: 76 Days and 23.6 Hours
Ankylosing spondylitis (AS) is a chronic rheumatic disease that primarily affects the spine and the sacroiliac and peripheral joints. Juvenile-onset AS (JoAS) pati
This report presents a case study of a 31-year-old male patient with a squatting gait due to severe bilateral KFC and HFC. The patient had a normal walking pat
The incidence of squatting gait due to KFC in individuals diagnosed with JoAS was low. Utilizing the Ilizarov technique has proven to be a secure and effective method for managing KFC in JoAS patients. Although the Ilizarov technique can
Core Tip: In Juvenile-onset ankylosing spondylitis (JoAS) patients, knee flexion contracture (KFC) is uncommon, with sparse literature on arthroplasty for ankylosed knees. We share a case where a JoAS patient’s severe bilateral KFC was effec
- Citation: Xia LW, Xu C, Huang JH. Use of Ilizarov technique for bilateral knees flexion contracture in Juvenile-onset ankylosing spondylitis: A case report. World J Clin Cases 2023; 11(29): 7179-7186
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7179.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7179
Juvenile-onset ankylosing spondylitis (JoAS) can cause deformities and disabilities of the hip and knee joints. The American College of Rheumatology recommends arthroplasty for AS patients with end-stage hip arthritis[1,2]. Total knee arthroplasty (TKA) is the most commonly performed surgical intervention for AS patients, aimed at reducing pain and improving knee mobility[3,4]. The incidences of total hip arthroplasty and TKA have recently increased in older AS patients[5]. Young and middle-aged AS patients also have an elevated risk of undergoing TKA[6]. However, performing TKA on patients with AS presents orthopedic surgeons with challenges, including surgical field exposure, soft tissue ba
Furthermore, AS patients have higher rates of infection, systemic complications, revision, and readmission following TKA than osteoarthritis patients[8]. Therefore, explore alternative options for delaying primary TKA in young and middle-aged individuals, especially those with partial hip and knee function and no joint rigidity. The Ilizarov technique is a skeletal traction method that has been widely used for fracture management, limb salvage, and deformity correction, including knee flexion contracture (KFC)[9-11]. However, there are few reports on managing severe KFC of JoAS with Ilizarov technique. The present study hypothesizes that the Ilizarov technique can safely and effectively correct KFC in JoAS.
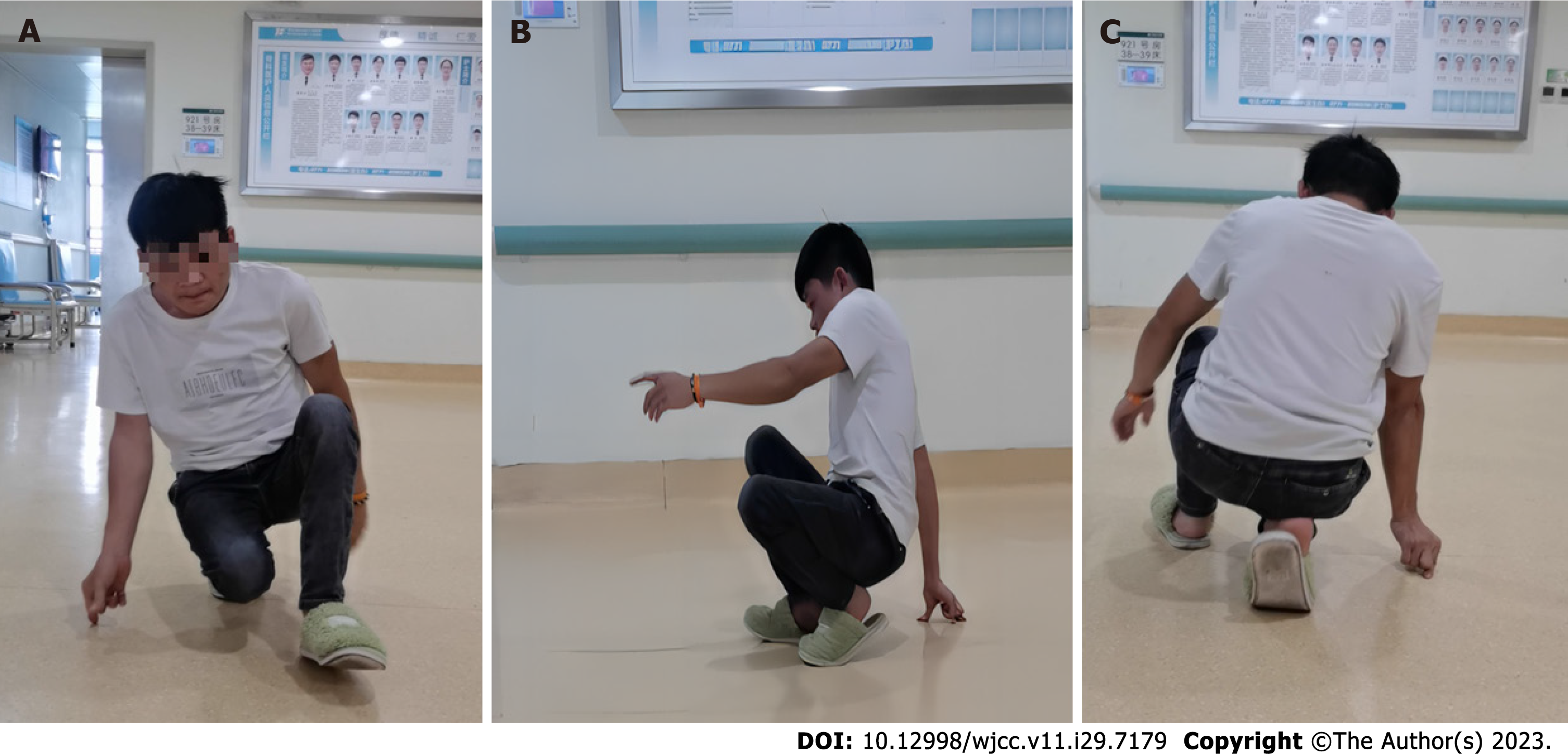
A 31-year-old male patient presented to our orthopedic clinic with a squatting gait and the desire to walk upright (Figures 1A-C).
The patient could walk normally until the age of eight.
The patient, at the age of 8, experienced pain in various peripheral joints, including the knees and hips. Regrettably, the family failed to acknowledge these symptoms, resulting in a delayed diagnosis and subsequent treatment.
The patient had no significant medical history and denied any family history of AS.
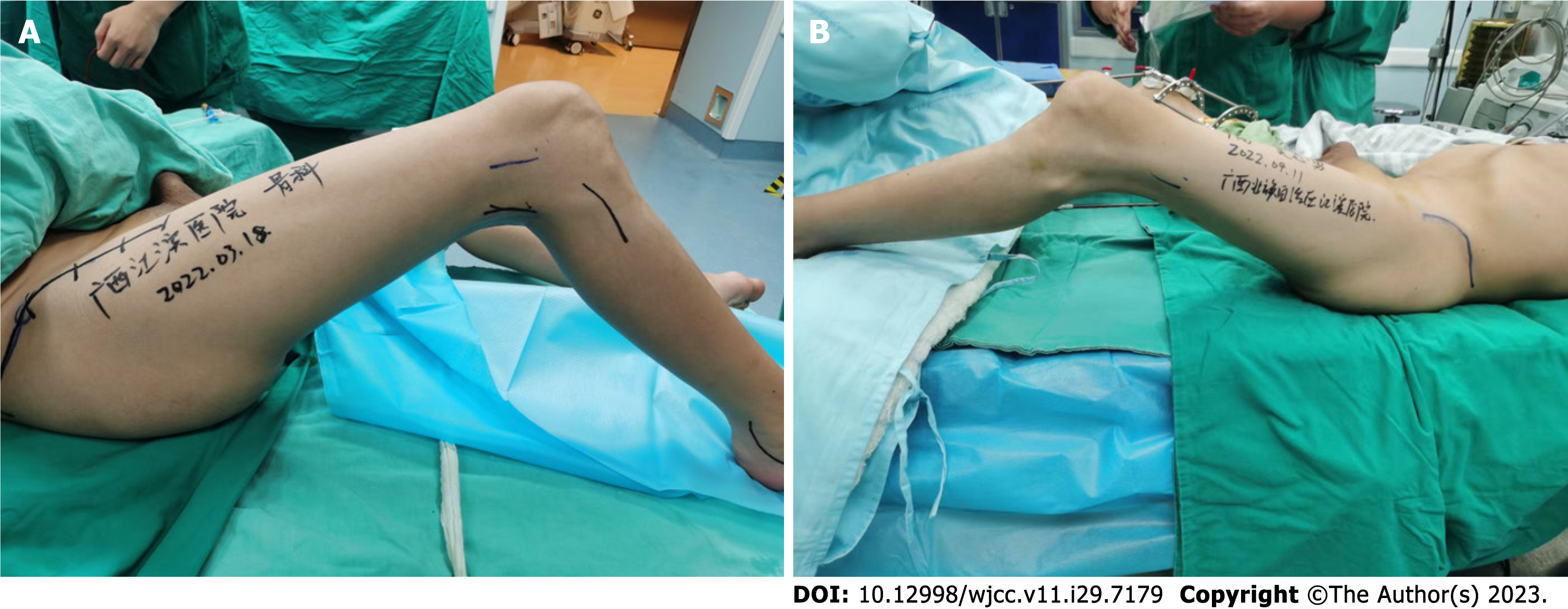
Upon examination, the right and left knees had a limited range of motion (ROM) of 75°-135° and 55°-135°, respectively (Figures 2A and B). The ROM of the right hip was limited to 50°-135°, while the left hip had a range of 45°-135°. Posterior extension of both the hips was limited.
The patient tested positive for HLA-B27, whereas negative for rheumatoid factor.
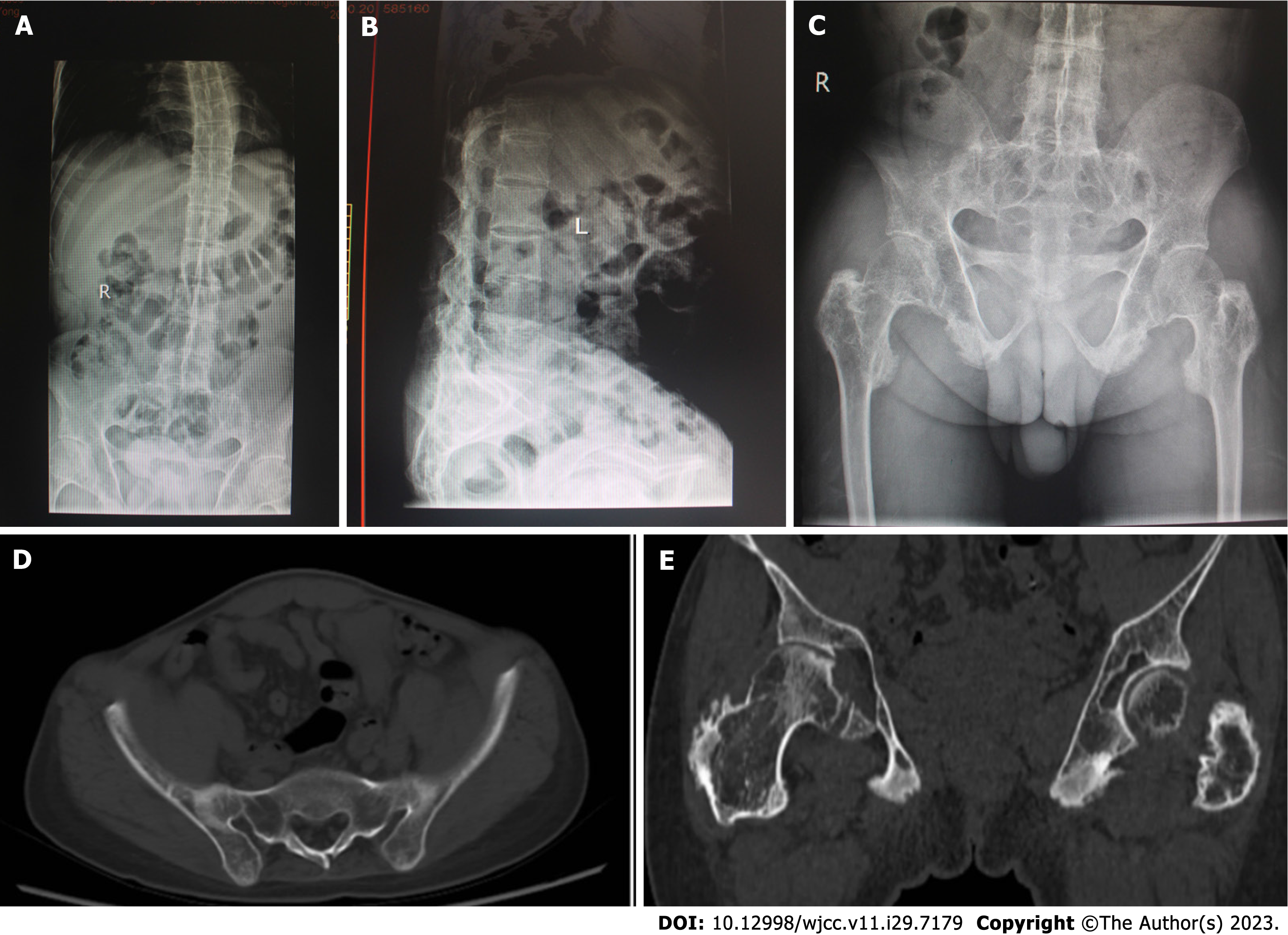
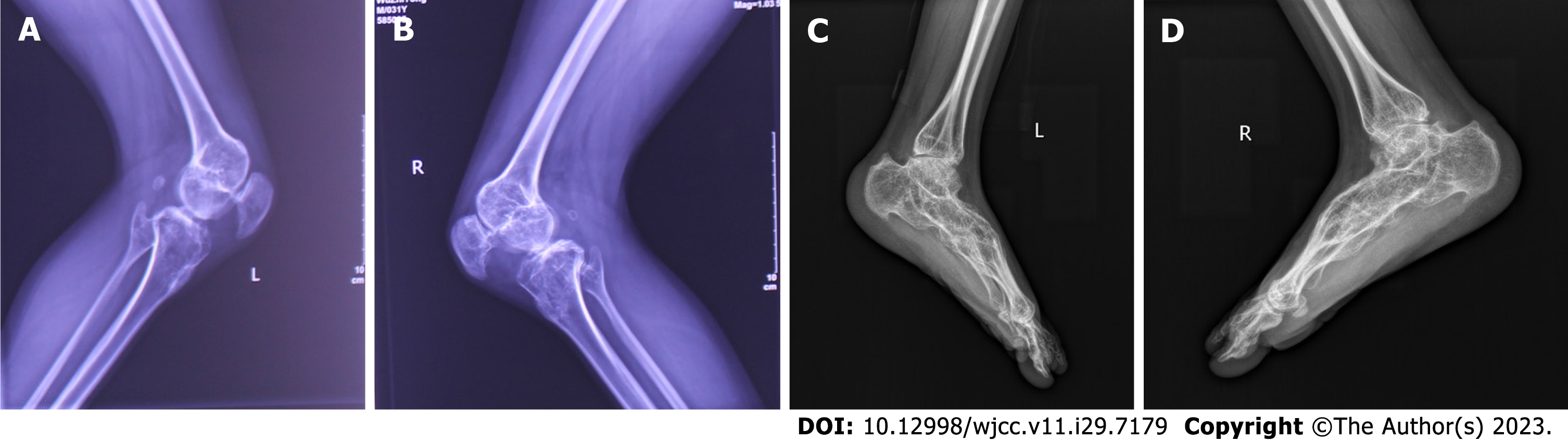
Plain radiographs of the spine exhibited characteristic bamboo-like alterations (Figures 3A and B). Plain radiography of Pelvis (Figure 3C) and computed tomography (CT) of Pelvis (Figure 3D) revealed sacroiliac joint fusion. Pelvis CT plain scans showed osteoarthritic changes in both hips, such as narrowing of the hip gaps, cystic changes beneath the articular cartilage, and significant bone hyperplasia around the greater and lesser trochanters (Figure 3E). Plain radiography of bilateral knees revealed a narrowing of the knee gaps and bilateral KFC (Figures 4A and B). Plain radiography of feet dis
The patient was diagnosed with neglected JoAS with bilateral KFC and hip flexion contracture (HFC).
In the present study, the patient did not exhibit knee or hip joint ankylosis. Although X-rays displayed knee and hip joints destruction, the patient did not complain of significant pain in these areas. Considering the relatively young age of the patient, performing primary TKA early increases the likelihood of future knee revisions. Therefore, the patient underwent hip dissection and release, as well as limited soft tissue release of the hamstring, along with gradual traction using the Ilizarov method.
The patient’s spinal vertebral fusion rendered epidural anesthesia impossible, necessitating general anesthesia despite the challenges associated with tracheal intubation. After administering anesthesia, the patient was positioned supine and a lateral incision measuring approximately 10 cm in length was made on the right hip to release the adherent hip joint. After the hamstring lengthening procedure, an Ilizarov ring external fixator was attached to the right thigh and proximal tibiofibular region. Neurolysis of the peroneal nerve was performed to prevent paralysis of the common peroneal nerve during knee distraction.
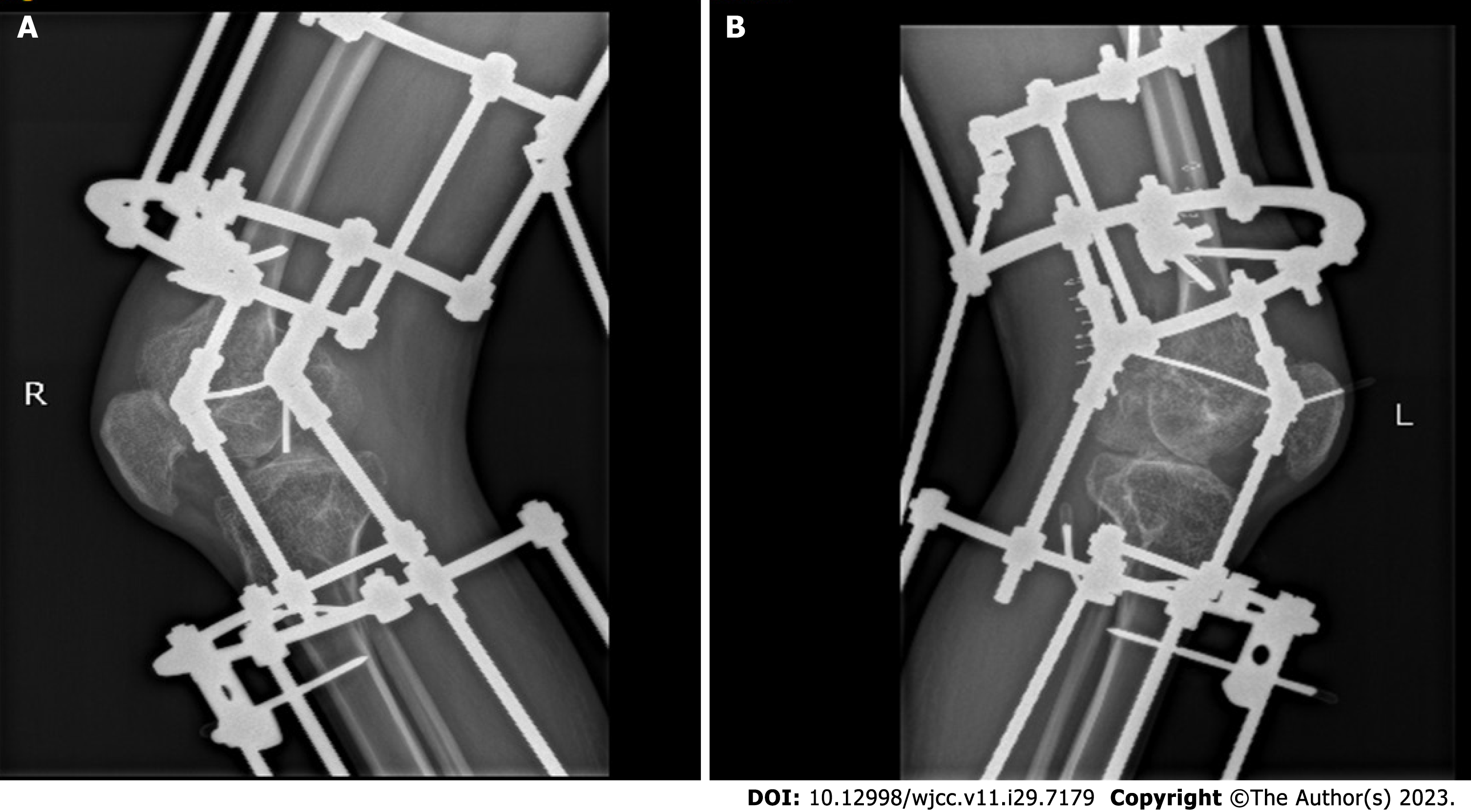
The threaded rod could be rotated posteriorly to initiate distraction once local pain and swelling had diminished significantly, typically five to seven days after surgery. The knee joint gap can be increased by approximately 5 mm to prevent compression of the articular cartilage during distraction. Subsequently, the nut on the posterior popliteal distraction rod was rotated to gradually distract the posterior knee soft tissue, thereby correcting the residual knee flexion deformity (Figures 5A and B). During treatment, a sandbag was used to compress the patient’s hip joint, and a physiotherapist was involved in providing bedside physiotherapy to address the residual hip flexion deformity.
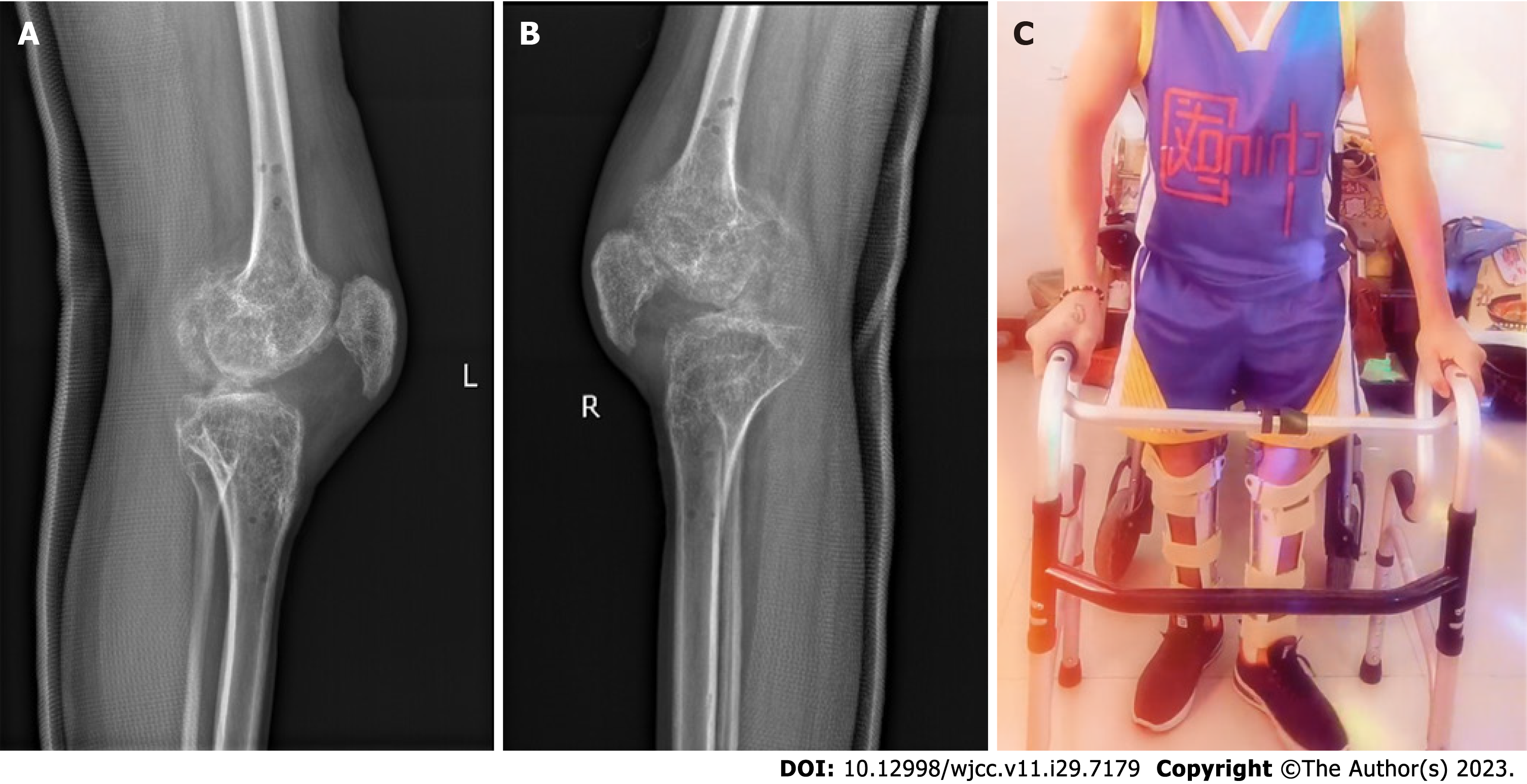
Three weeks after the surgery, the same procedure was performed on the left lower extremity. Once the bilateral HFC and KFC were fully corrected, the patient was encouraged to stand and walk with the assistance of a walker. After 10 wk, the patient was readmitted to the hospital to remove the Ilizarov external fixation device (Figures 6A and B). During the procedure, a plaster model of the patient’s lower extremities was obtained to facilitate the customization of a long-leg brace for both limbs. Subsequently, the patient was encouraged to walk on the ground wearing a bilateral lower limb long-leg brace. Radiographs of both knee joints showed the patient had full extension of both knees (Figures 7A and B). Following discharge from the hospital, the patient independently engaged in standing and upright walking exercises at home (Figure 7C).
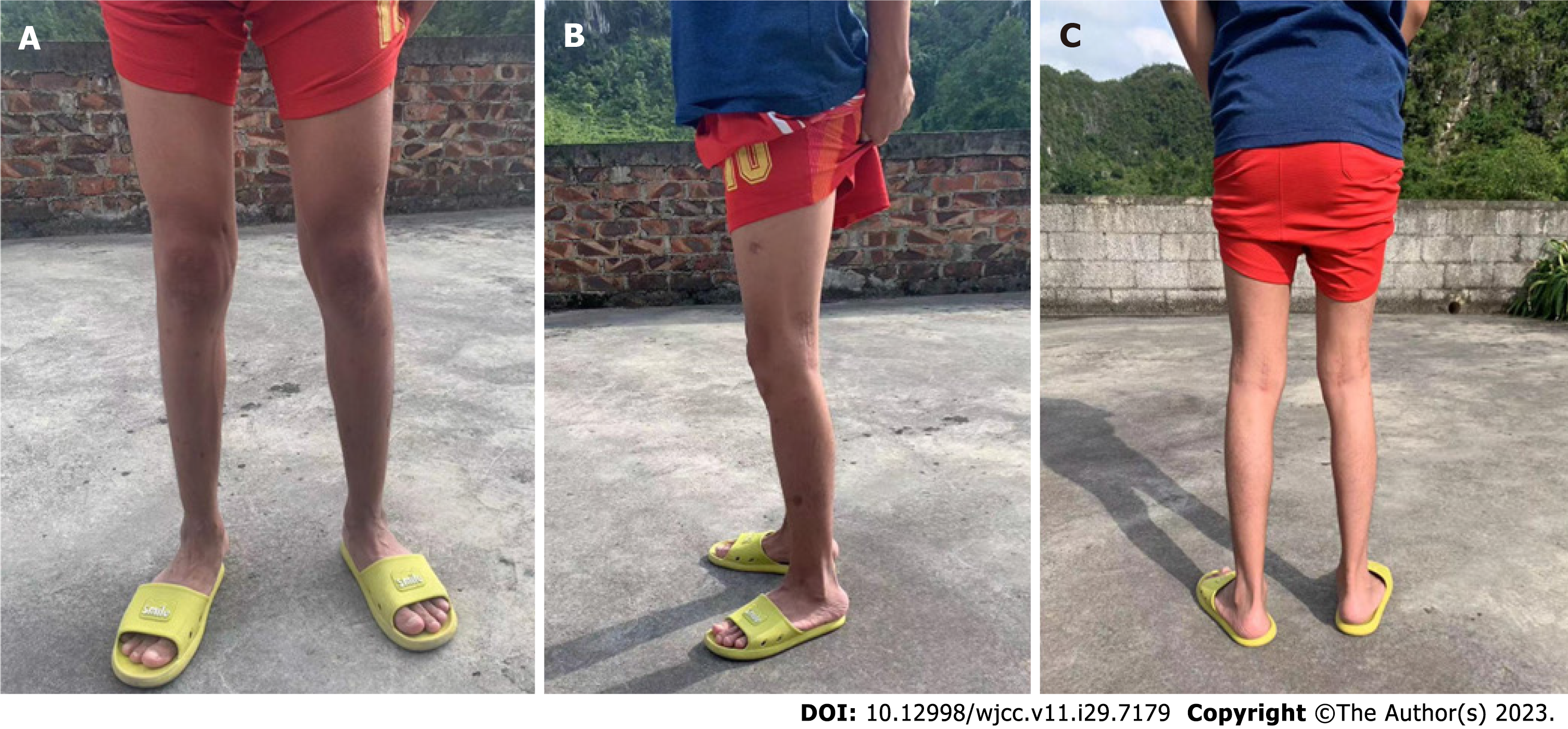
Approximately three months later, the patient presented to the outpatient clinic with bilateral knee extension stiffness. After receiving physiotherapy, manipulation, and sodium hyaluronate injection into the knee joint by a rehabilitation therapist, the patient could actively flex both knees to 110°. Twelve months postoperatively, the patient achieved inde
KFC can arise from various etiologies, such as congenital diseases, inflammatory conditions, and miscellaneous reasons[12]. The Ilizarov technique is a safe and effective method that can be used to treat KFC caused by various pathologies. However, the purpose of using the Ilizarov technique differs depending on the etiology of the KFC.
Common causes of KFC are cerebral palsy, poliomyelitis, congenital spina bifida, trauma, and burns. Limb length discrepancy affects patient aesthetics and ambulation. The knee is gradually straightened by the continuous and slow distraction of the Ilizarov ring external fixator, restoring symmetrical lower limb lengths.
KFC has also been observed in patients with brain injuries and stroke[13]. The Ilizarov technique can increase a patient’s walking ability if they has the potential to walk. The Ilizarov technique has the potential to improve comfort and hygiene and facilitate care for patients who are expected not to walk even after surgery[14].
Septic knee arthritis can also result in KFC[15]. The Ilizarov technique is a viable option to achieve knee arthrodesis in cases of septic failure following TKA, post-traumatic knee infection, and end-stage tuberculosis of the knee[16-18]. Junior rheumatoid arthritis (JRA) can destroy the knee cartilage and develop KFC. TKA is the most commonly reported surgical procedure, whereas the Ilizarov technique is rarely reported. Guo et al[19] reported nine patients diagnosed with severe KFC due to JRA. All the patients underwent gradual distraction using an Ilizarov ring external fixator. At the last follow-up, all patients completed knee extension without severe complications. The authors believe that Ilizarov technique corrected the knee flexion deformity, providing a foundation for subsequent TKA. Vecham et al[20] described a 22-year-old female patient with JRA and severe bilateral KFC who underwent a two-stage procedure. The initial stage involved using Ilizarov ring external fixators to completely correct the KFC. The patient underwent bilateral TKA during the second stage. Since the patient’s KFC was completely corrected in the first stage, second-stage TKA was relatively easy to perform, as it did not require excessive osteotomy and soft tissue balancing.
JoAS, like RA, is an inflammatory rheumatic disease that affects the joints, including the knee. However, clinically reported cases of KFC are less common due to JoAS. To our knowledge, there have been no reports of Ilizarov treatment of severe bilateral KFC caused by JoAS. This study presents a novel therapeutic approach for patients diagnosed with JoAS who exhibit severe KFC. In this case report, the patient realized his desire to walk upright and was satisfied with the results despite some complications, such as high-lever pain and sleep disturbances. However, It remains necessary to follow up for a longer period to determine potential long-term efficacy differences.
The presence of hip and knee arthritis in individuals diagnosed with JoAS can result in HFC and KFC, potentially inducing gait abnormalities in affected patients. A combination of limited soft tissue release from the knee joint and Ilizarov distraction therapy is a safe and effective procedure. Although this procedure is not a substitute for TKA, it can help avoid the need for early or delayed primary joint replacement, consequently mitigating the likelihood of future knee revision.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dauyey K, Kazakhstan; Malkova TA, Russia; Oommen AT, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Ward MM, Deodhar A, Akl EA, Lui A, Ermann J, Gensler LS, Smith JA, Borenstein D, Hiratzka J, Weiss PF, Inman RD, Majithia V, Haroon N, Maksymowych WP, Joyce J, Clark BM, Colbert RA, Figgie MP, Hallegua DS, Prete PE, Rosenbaum JT, Stebulis JA, van den Bosch F, Yu DT, Miller AS, Reveille JD, Caplan L. American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network 2015 Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2016;68:282-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 320] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 2. | Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, Haroon N, Borenstein D, Wang R, Biehl A, Fang MA, Louie G, Majithia V, Ng B, Bigham R, Pianin M, Shah AA, Sullivan N, Turgunbaev M, Oristaglio J, Turner A, Maksymowych WP, Caplan L. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019;71:1599-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 426] [Article Influence: 71.0] [Reference Citation Analysis (0)] |
| 3. | Rajgopal A, Ahuja N, Dolai B. Total knee arthroplasty in stiff and ankylosed knees. J Arthroplasty. 2005;20:585-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Owen AR, Markos JR, Mabry TM, Taunton MJ, Berry DJ, Abdel MP. Contemporary Primary Total Knee Arthroplasty is Durable in Patients Diagnosed With Ankylosing Spondylitis. J Arthroplasty. 2020;35:3161-3165. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Ward MM. Increased Rates of Both Knee and Hip Arthroplasties in Older Patients with Ankylosing Spondylitis. J Rheumatol. 2019;46:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Ward MM. Risk of total knee arthroplasty in young and middle-aged adults with ankylosing spondylitis. Clin Rheumatol. 2018;37:3431-3433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Sharma M, Sharma S, Upadhyaya AR. Classification-Based Management of Stiff/Ankylosed Knees. Indian J Orthop. 2021;55:1158-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Cancienne JM, Werner BC, Browne JA. Complications of Primary Total Knee Arthroplasty Among Patients With Rheumatoid Arthritis, Psoriatic Arthritis, Ankylosing Spondylitis, and Osteoarthritis. J Am Acad Orthop Surg. 2016;24:567-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Gubin AV, Borzunov DY, Malkova TA. The Ilizarov paradigm: thirty years with the Ilizarov method, current concerns and future research. Int Orthop. 2013;37:1533-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Devalia KL, Fernandes JA, Moras P, Pagdin J, Jones S, Bell MJ. Joint distraction and reconstruction in complex knee contractures. J Pediatr Orthop. 2007;27:402-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Hosny GA, Fadel M. Managing flexion knee deformity using a circular frame. Clin Orthop Relat Res. 2008;466:2995-3002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Herzenberg JE, Davis JR, Paley D, Bhave A. Mechanical distraction for treatment of severe knee flexion contractures. Clin Orthop Relat Res. 1994;80-88. [PubMed] [DOI] [Full Text] |
| 13. | Keenan MA, Ure K, Smith CW, Jordan C. Hamstring release for knee flexion contracture in spastic adults. Clin Orthop Relat Res. 1988;221-226. [PubMed] [DOI] [Full Text] |
| 14. | Martin JN, Vialle R, Denormandie P, Sorriaux G, Gad H, Harding I, Dizien O, Judet T. Treatment of knee flexion contracture due to central nervous system disorders in adults. J Bone Joint Surg Am. 2006;88:840-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Athanasiou V, Panagopoulos A, Gliatis J, Papathanasiou N, Tyllianakis M, Megas P. Neglected Posterior Dislocation Septic Loosening and Prolonged Flexion Contracture of Total Knee Arthroplasty: A Case Report. Am J Case Rep. 2021;22:e931857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Bruno AA, Kirienko A, Peccati A, Dupplicato P, De Donato M, Arnaldi E, Portinaro N. Knee arthrodesis by the Ilizarov method in the treatment of total knee arthroplasty failure. Knee. 2017;24:91-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 17. | Sun J, Li Q, Gao F, Xiang Z, Huang Q, Li L. Application of the Ilizarov technique for knee joint arthrodesis as a treatment for end-stage tuberculosis of the knee. BMC Musculoskelet Disord. 2020;21:579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Vaish A, Rabari Y, Vaish R, Vaishya R. Correction of a Severe Flexion Knee Deformity Using 3D Printing. Indian J Orthop. 2020;54:228-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 19. | Guo B, Qin S, Zheng X, Zang J, Zhao W, Wu H. Ilizarov technique for severe knee flexion contracture in juvenile rheumatoid arthritis. J Orthop Translat. 2020;25. [DOI] [Full Text] |
| 20. | Vecham R, Annapareddy A, Hippalgaonkar K, Bhushan C, Pawar S, Reddy AVG. Two-Staged Total Knee Arthroplasty in Juvenile Rheumatoid Arthritis with Severe Flexion Deformity: A Case Report. JBJS Case Connect. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |