Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7113
Peer-review started: June 7, 2023
First decision: August 4, 2023
Revised: August 21, 2023
Accepted: September 18, 2023
Article in press: September 18, 2023
Published online: October 16, 2023
Processing time: 128 Days and 12.2 Hours
Primary renal lymphoma (PRL) is extremely rare with an incidence of 0.7% among extranodal lymphomas. Occult renal lymphoma, which mimics medical renal disease and bilateral renal involvement, presents a diagnostic challenge to nephrologists and radiologists as the clinical and radiological findings are mostly non-specific or inconclusive. Acute kidney injury (AKI) is not an uncommon finding in renal infiltration due to malignant lymphoma. However, only 14% of cases are detected before death, and the low diagnostic rate may be due to the non-specific clinical manifestations of renal involvement, with only 0.5% of these cases presenting with AKI. Moreover, PRL is difficult to diagnose based on clinical, biochemical, and radiologic features, especially, in the case of bilateral diffuse involvement.
Herein, we report a 74-year-old woman with primary diffuse large B-cell lymphoma who presented with AKI diagnosed by ultrasound-guided needle biopsy. We also report the clinicopathologic findings of 121 PRL cases reported since 1989, by conducting a literature review of published cases.
A timely renal biopsy provides the most expedient means of establishing the diagnosis. Thus, early identification of the disease by the clinician facilitates early diagnosis toward effective treatment.
Core Tip: We report a patient with bilateral primary renal lymphoma (B-PRL) presenting with acute kidney injury (AKI), and conducted a literature review of 121 cases of PRL since 1989. Among the 121 cases, 29.8% were bilateral. AKI occurred in all bilateral cases, and 71.4% of patients who died were diagnosed with B-PRL. There is a need to discuss more active treatment for B-PRL. In particular, differentiating diffuse involvement of lymphoma from other kidney diseases causing AKI is difficult clinically or radiologically; therefore, a kidney biopsy is essential for the diagnosis. Clinicians should endeavor to make a preoperative diagnosis, to avoid unnecessary surgery.
- Citation: Lee SB, Yoon YM, Hong R. Primary renal lymphoma presenting as renal failure: A case report and review of literature from 1989. World J Clin Cases 2023; 11(29): 7113-7126
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7113.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7113
Primary renal lymphoma (PRL), defined as a lymphoma involving the kidneys in the absence of extrarenal lymphoma, is a rare disease. Additionally, PRL accounts for approximately 0.7% of extranodal lymphomas[1], as the kidney is an extranodal organ and the renal parenchyma does not contain lymphatic tissue[2]. Occasionally, patients present with nonspecific signs and symptoms including flank pain, weight loss, hematuria, a palpable mass, or symptoms of acute kidney injury (AKI). Evaluation of renal lymphoma is important and includes differentiating PRL from other renal neoplasms, making pathologic diagnoses, and preserving renal parenchyma and function[3]. Radiologically, the typical computed tomography (CT) pattern in renal lymphoma can be grouped approximately as multiple renal masses (approximately 60%, most common), solitary masses (< 6%, rarest), renal invasion from retroperitoneal disease, or diffuse renal infiltration[1,3-6]. The diffuse infiltration pattern is always bilateral, observed in approximately 25%-30% of renal lymphomas[6]. Moreover, the pattern is difficult to diagnose by imaging alone due to the non-specific manifestations. In particular, PRL with a diffuse growth pattern in the bilateral kidney may clinically mimic medical renal disease and even escape detection during the routine radiological work-up, including ultrasonography (US) and CT, preceding biopsy. Percutaneous renal biopsy is generally used in the diagnosis of medical renal diseases, although the indications for biopsy vary. Renal neoplasms, which are typical urological disorders, are not generally recommended for percutaneous biopsy[7], but the tumor may be detected incidentally during a biopsy. For a rapid and confirmative diagnosis, kidney biopsy remains the gold standard. Therefore, although rare, clinicians should consider lymphoma as a differential diagnosis during percutaneous renal biopsy for diagnosing the aforementioned lesions. According to a population-based analysis using the Surveillance, Epidemiology, and End Results Program, factors such as old age, primary diffuse large B-cell lymphoma (DLBCL) histologic type, and male patients are associated with short overall survival (OS)[8].
To the best of our knowledge, to date, 121 cases of PRL have been reported in the literatures[1,2,4,9-97]. Herein, we report the case of primary renal DLBCL of 74-year-old woman presenting with AKI, diagnosed by US-guided needle biopsy. We also conducted a literature review of the 121 cases reported since 1989 and described their clinicopathologic findings. This study was approved by the Institutional Review Board (IRB) of Chosun University Hospital, Gwangju, Korea, which waived the requirement for written informed consent due to the nature of the study (IRB No. 2023-02-020).
A 74-year-old woman who was treated outside our hospital due to complaints of general weakness, hematuria, dysuria, and decreased renal function was transferred to Chosun University Hospital, Gwangju, Korea, as her renal function did not improve despite treatment.
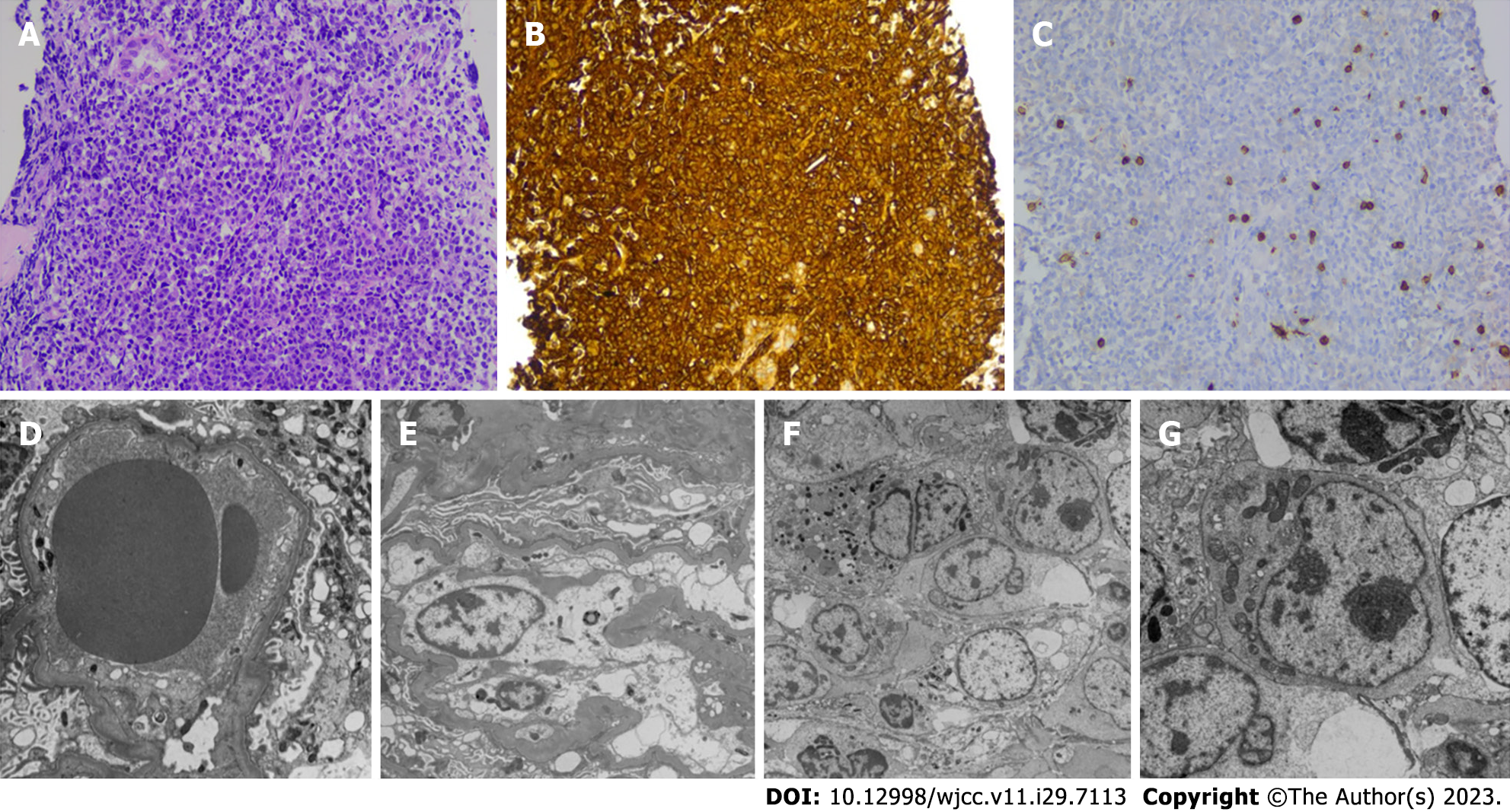
Clinically, rapid progressive glomerulonephritis (RPGN) was suspected. Two days after admission, US-guided percutaneous renal biopsy was performed to confirm the pathologic diagnosis, before initiating steroid treatment. Contrary to expectations, the light microscopic examination identified diffuse infiltration of pleomorphic cells throughout the specimen. The pleomorphic cells were immunoreactive for CD20, bcl-2, bcl-6, and MUM-1, but negative for CD3, CD10, and Epstein-Barr encoding region in situ hybridization (Figure 1). No fluorescence deposit was identified during immunofluorescence examination. In electro-microscopic examination, no electron-dense deposit was observed, and the glomerular basement membrane appeared normal in thickness, contour, and texture. However, strikingly, diffuse prominent infiltration of atypical lymphocytes was observed in the interstitium. The cells displayed round to oval cleaved and non-cleaved nuclei with variable clumping of chromatin, and large prominent, marginated nucleoli (Figure 1). We diagnosed the condition as DLBCL, not medical renal disease. After pathologic diagnosis, radiologic re-evaluation was performed. Abdominal CT examination (with contrast) revealed diffuse homogeneous enhancement in both kidneys without definite visible cortico-medullary differentiation, and lymphomatous involvement was diagnosed. A few mild enlargements of lymph nodes in the pericardial and periaortic chains were identified, and such nodes were considered to indicate secondary lymphomatous involvement. On fluorodeoxyglucose-positron emission tomography CT, intense hypermetabolism (19.6) was identified in both kidneys, and some lymph nodes exhibited mild hypermetabolism (Figure 2). In the laboratory tests, serum lactate dehydrogenase (LDH) level was elevated to 376 U/L (125-220 U/L). The international prognostic index (IPI) was reported as 3 when the following laboratory data and clinicopathologic factors were considered [old age, 1; Eastern Cooperative Oncology Group (ECOG) performance status (PS), 1; Ann Arbor stages III–IV, 0; serum level > 1 × normal, 1; and > 1 extranodal site, 0].
The patient had no previous renal problems.
There was no specific personal or family history.
The patient looked ill.
After admission, the blood urea nitrogen (normal range, 7.0-20.1 mg/dL)/creatinine (0.57-1.11 mg/dL) levels on June 30, July 9, and July 11, 2022 were as follows: 27.7/4.09; 41.0/6.61; and 48/7.62 mg/dL, respectively.
Radiologically, renal US exhibited heterogeneously increased parenchymal echogenicity and a 1.43 cm-sized hypoechoic cystic lesion in the right kidney. Thus, the radiologist suggested probable medical renal disease with a right cystic lesion. During abdominal CT (contrast-free CT while admitted to the emergency room), no neoplastic lesion was suspected.
The patient was diagnosed with DLBCL.
She was immediately started on chemotherapy (CTx), which was composed of rituximab-cyclophosphamide, vincristine, adriamycin, and prednisolone.
The patient succumbed to her illness 3 mo after diagnosis during her third round of CTx.
As demonstrated during the literature search, according to Stallone et al[5] who reported 29 cases in a literature review in 2000[66,76,98,99], PRL is very rare with an incidence of 0.7% in extranodal lymphomas[1]. Since 1989 when Paganelli et al[2] presented the first patient with PRL diagnosed by open kidney biopsy, to our knowledge, 121 cases have been reported in the medical literature, including our case (Table 1). The present study reviewed all 121 cases of PRL reported in the literature since 1989.
| Factor | Factor | ||
| Gender | Age (yr) | ||
| Male | 72 (58.5) | ≤ 20 | 16 (13.2) |
| Female | 45 (36.6) | 21-40 | 7 (5.8) |
| Unknown | 4 (3.3) | 41-60 | 41 (33.8) |
| 61-80 | 48 (39.7) | ||
| ≥ 80 | 9 (7.4) | ||
| Site | Prognosis | ||
| Unilateral | 81 (66.9) | Died due to lymphoma | 21 (17.4) |
| Bilateral | 36 (29.8) | Free of disease | 68 (56.2) |
| Unknown | 4 (3.3) | Recurrence | 5 (4.1) |
| Unknown | 27 (22.3) | ||
| Histologic diagnosis | Treatment | ||
| DLBCL | 62 (51.2) | CTx | 67 (55.4) |
| BCL, other | 22 (18.2) | CTx + surg | 24 (19.8) |
| MZL | 23 (19.0) | CTx + RTx | 5 (4.1) |
| FL | 3 (2.5) | CTx + stem cell | 1 (0.8) |
| TCL | 2 (1.7) | TPL | 2 (1.7) |
| T-LBL | 3 (2.5) | CTx + Surg + RTx | 2 (1.7) |
| NHL | 2 (1.7) | RTx Surg | 9 (7.4) |
| Unknown | 4 (3.2) | Steroid therapy | 3 (2.5) |
| Antibiotics | 1 (0.8) | ||
| No | 3 (2.5) | ||
| Unknown | 4 (3.3) | ||
Of these 121 cases, the male-to-female ratio was 1.6:1 (72:45; unknown, 4 patients). The average age of the patients was 55 years, and the distribution is displayed in Table 2. A total of 36 (29.8%), 81 (66.9%), and 4 (3.3%) cases of bilateral renal involvement, unilateral lesion, and unknown, respectively, were observed. The bilateral involvement in PRL may be age-related. Patients aged < 40 years have higher bilateral renal involvement (17/23, 73.9%) compared with those aged ≥ 40 years (19/98, 19.4%) (Table 2).
| Age (yr) | Bilateral | AKI | Prognosis-dead | |
| ≤ 10 | 11 (9.1) | 9 (81.8) | 0 | 5 (45.5) |
| 11-20 | 5 (4.1) | 3 (60.0) | 0 | 0 |
| 21-30 | 3 (2.5) | 3 (100) | 1 (33.3) | 0 |
| 31-40 | 4 (3.3) | 2 (50.0) | 0 | 2 (50.0) |
| 41-50 | 17 (14.0) | 3 (17.6) | 3 (17.6) | 2 (11.8) |
| 51-60 | 24 (19.8) | 6 (25.0) | 2 (8.3) | 2 (8.3) |
| 61-70 | 22 (18.2) | 6 (27.3) | 1 (4.5) | 5 (22.7) |
| 71-80 | 26 (21.5) | 4 (15.4) | 4 (15.4) | 5 (19.2) |
| ≥ 80 | 9 (7.4) | 0 | 0 | 0 |
| 123 | 36 (29.3) | 11 (8.9) | 21 (17.4) |
Histologically, DLBCL is the most common (62/121, 51.2%) lymphoma, followed by marginal zone lymphoma (23/121, 19.0%). Symptoms and signs include abdominal distension, fever, flank pain, nausea and vomiting, hematuria, frequency, urinary retention, hydronephrosis, and AKI. Some cases were identified incidentally without any symptoms. According to Coggins[100], AKI in renal lymphoma may occurs by several causes such as infections and obstructive urinary disease with leukemic infiltration contributing to the progression of renal failure. Bridoux et al[101] suggested that invasion of lymphoma to the renal interstitium induces compression of tubules and peritubular capillaries, which leads to tubular obstruction and increase of post-glomerular vascular resistance.
In the current review, AKI with symptoms was found in 11 cases (8.9% of all the cases and 30.6% of cases with bilateral lesions), and all exhibited bilateral diffuse renal involvement. However, the incidence of AKI did not correlate with age but occurred more consistently in those over 40 years old (< 40 years old, 1/23, 4.3%) (Table 3).
| No | Age (yr) | Sex | Side | Presentation | Diagnosis | Tx | Prognosis | Year | Ref. |
| 1 | 53 | F | B | Poor appetite, wt loss | NHL | CTx | Died at 3 d | 1989 | Paganelli et al[2] |
| 2 | 58 | M | B | Anorexia, wt loss, night sweat, malaise | B-cell NHL | CTx | NR | 1992 | Taneja et al[8] |
| 3 | 51 | F | U | Pain | SNCL | CTx | NR | 1993 | Van Gelder et al[9] |
| 4 | 4 | M | B | Fever, N/V | NR | CTx | Died after 16 mo | 1994 | Salem et al[10] |
| 5 | 5 | F | B | Fever, wt loss sweat | B-LBL | CTx | Died after 20 mo | 1994 | Salem et al[10] |
| 6 | 49 | F | B | Renal impairment, fever, wt loss, LBP | Centroblastic lymphoma | CTx | Died after 10 wk | 1994 | Salem et al[10] |
| 7 | 52 | F | U | Pain | DLBCL | CTx | Remission-relapse | 1995 | Arranz et al[11] |
| 8 | 59 | M | U | Pain | SNCL | CTx | Remission | 1995 | Arranz et al[11] |
| 9 | 60 | F | U | Pain | DLBCL | CTx | Remission | 1995 | Arranz et al[11] |
| 10 | 60 | M | U | Pain | DLBCL | CTx | Remission-relapse | 1995 | Arranz et al[11] |
| 11 | 63 | F | B | Pain | DLBCL | CTx | Died after 4.5 mo | 1995 | Arranz et al[11] |
| 12 | 73 | F | B | N/V, AKI | DLBCL | PDS | Died after 3 mo | 1999 | Okuno et al[12] |
| 13 | 50 | M | U | NR | MZL | No | Remission | 1999 | Chin et al[13] |
| 14 | 76 | F | U | Flank pain | MALT | Surg | NR | 2000 | Stallone et a[5] |
| 15 | 45 | M | U | Pain, fever | MZL | CTx | Remission-relapse | 2001 | Mhawech et al[15] |
| 16 | 51 | M | B | Flank pain | TCL | CTx | Died after 15 mo | 2001 | Jindal et al[16] |
| 17 | 45 | M | U | Incidental | BCL, Burkitt | Surg CTx | Remission | 2002 | O'Riordan et al[17] |
| 18 | 62 | M | B | Hematuria, acute urinary retention, | BCL, follicular | CTx | Died after 2 mo | 2002 | O'Riordan et al[17] |
| 19 | 14 | M | B | Headache, HTN, flank pain, Wt loss, | DLBCL | CTx | Alive at 2 wk | 2002 | Gellrich et al[18] |
| 20 | 78 | M | U | Hematuria | DLBCL | Surg, CTx | Alive at 2 yr | 2002 | Levendoglu et al[19] |
| 21 | 77 | M | U | Not determined | MZL | No | Remission | 2002 | Mansouri et al[20] |
| 22 | 68 | F | NR | NR | MALT | PDS | NR | 2002 | Mita et al[21] |
| 23 | 72 | F | NR | NR | MALT | PDS | NR | 2002 | Mita et al[21] |
| 24 | 57 | F | ND | Pain, fever | BCL | CTx | NR | 2003 | Stokes et al[22] |
| 25 | 79 | M | U | Pain, weakness, U/O↓ | MZL | Surg, CTx | Alive at 2 mo | 2003 | O'Sullivan et al[23] |
| 26 | 82 | M | U | Pain | DLBCL | CTx | D's free after 1 yr | 2003 | Olusanya et al[24] |
| 27 | 43 | M | U | Lt. flank pain | MALT | Surg, CTx | Alive at 28 mo | 2003 | Pervez et al[25] |
| 28 | 46 | M | B | RF | DLBCL | Surg, CTx | Alive at 67 mo | 2004 | Tuzel et al[26] |
| 29 | 17 | M | U | Flank pain | DLBCL | CTx | Remission | 2004 | Cupisti et al[27] |
| 30 | 70 | F | U | Anorexia, malaise, fever | DLBCL | Surg, CTx | Alive at 8 mo | 2004 | Ozaltin et al[28] |
| 31 | 65 | F | U | Unknown | DLBCL | Surg, CTx, RTx | Alive at 18 mo | 2005 | Zomas et al[29] |
| 32 | 68 | M | B | Pain | DLBCL | No | Died after 10 d | 2006 | Ahmad et al[30] |
| 33 | 70 | M | U | LBP | DLBCL | CTx | D's free after 1 yr | 2006 | Kaya et al[31] |
| 34 | 62 | M | B | Oliguria, ARF | DLBCL | CTx | Died after 3rd CTx | 2006 | Bozas et al[32] |
| 35 | 68 | F | B | Flank pain, dysuria | LCL | Unknown | Died after 10 d | 2006 | Ahmad et al[30] |
| 36 | 53 | M | U | Not determined | MZL | CTx | Remission | 2006 | Guilpain et al[33] |
| 37 | 72 | M | U | Fever, chill | MZL | Surg | NR | 2006 | Guilpain et al[33] |
| 38 | 83 | F | U | Flank pain | MZL | CTx | D's free after 8 mo | 2006 | Guilpain et al[33] |
| 39 | 83 | F | U | Pain, fever | MZL | CTx, RTx | Remission | 2006 | Guilpain et al[33] |
| 40 | 2 | M | B | Abd. Distension, U/O↓ | TCL | CTx | F/U loss | 2006 | Qiu et al[34] |
| 41 | 71 | F | U | wt loss, fever | BCL | Surg, CTx | Died after 4 mo | 2006 | Tefekli et al[1] |
| 42 | 78 | M | U | Pain | DLBCL | CTx | Remission | 2006 | Sharma et al[35] |
| 43 | 5 | M | B | HTN | TCL | CTx | Died after 2 mo | 2007 | Valarmathi et al[36] |
| 44 | 77 | ND | B | ARF | DLBCL | CTx, RTx | Remission | 2007 | Becker et al[37] |
| 45 | 50 | M | U | Abd pain | DLBCL | Surg, CTx | Alive at 1 mo | 2007 | Diskin et al[38] |
| 46 | 62 | M | U | Hematuria | DLBCL | Surg, CTx, IFN | Alive at 5 yr | 2007 | Diskin et al[38] |
| 47 | 84 | M | U | Unknown | BCL | Surg, CTx, IFN | Alive at 5 yr | 2007 | Diskin et al[38] |
| 48 | 54 | M | U | ND | MZL (MALT) | CTx | Remission | 2007 | Fang et al[39] |
| 49 | 65 | ND | U | ND | MZL (MALT) | Antibiotics | Remission | 2007 | Fang et al[39] |
| 50 | 66 | F | U | ND | MZL | Surg | Remission | 2007 | Fang et al[39] |
| 51 | 75 | M | U | ND | MZL (MALT) | CTx | Remission | 2007 | Fang et al[39] |
| 52 | 77 | F | ND | ND | MZL (MALT) | NR | Remission | 2007 | Fang et al[39] |
| 53 | 83 | M | U | ND | MZL (MALT) | CTx | Remission | 2007 | Fang et al[39] |
| 54 | 49 | M | U | Abd pain, fever | DLBCL | CTx | NR | 2007 | Bokhari et al[102] |
| 55 | 21 | M | B | Fever, wt loss, pain, | DLBCL | CTx | NR | 2007 | Garcia et al[40] |
| 56 | 58 | M | U | Headache, memory loss | DLBCL | Surg, CTx | Well on CTx | 2007 | Omer et al[41] |
| 57 | 57 | M | B | Dyspnea, RF, anemia | NR | CTx, Stem, cell TPL | NR (regression) | 2008 | Rajappa et al[42] |
| 58 | 55 | F | U | Fever | DLBCL | CTx | D's free after 1 mo | 2008 | James et al[43] |
| 59 | 62 | F | U | Fever, flank pain | DLBCL | Surg, CTx | Alive at 1 yr | 2008 | Ladha et al[4] |
| 60 | 62 | M | U | Pain | DLBCL | CTx, RTx | Remission-relapse | 2008 | Ladha et al[4] |
| 61 | 3 | M | B | Abd. distension, abd. pain, fever | BCL | CTx | Died after 5th CTx | 2009 | Kuo et al[44] |
| 62 | 71 | M | U | Unknown | DLBCL | CTx | Alive 2 yr | 2009 | Jindal et al[45] |
| 63 | 74 | M | U | Unknown | DLBCL | Surg, CTx | D's after 2nd CTx | 2009 | Jindal et al[45] |
| 64 | 75 | F | U | Unknown | DLBCL | Surg, CTx | Alive at 1 yr | 2009 | Jindal et al[45] |
| 65 | 81 | M | U | Hematuria | SBL | Surg, CTx | NR | 2009 | Jindal et al[45] |
| 66 | 60 | M | U | Dyspnea, fatigue | FL | Surg, CTx | NR | 2009 | Kose et al[46] |
| 67 | 82 | M | U | Mass | NR | RTx | NR | 2009 | Pinggera et al[47] |
| 68 | 52 | F | B | BP, headache, dysuria, hematuria, ARF, HTN | DLBCL | CTx | Alive 2 yr NR s | 2009 | Renaud et al[48] |
| 69 | 46 | M | U | Wt loss, fever, pain | DLBCL | CTx | Alive 7 mo | 2009 | Reuter et al[49] |
| 70 | 47 | M | U | Chronic graft dysfunction | BCL | Surg | Alive at 6.5 yr | 2009 | Reuter et al[49] |
| 71 | 77 | F | U | Anorexia, asthenia, malaise | DLBCL | Surg, CTx | Alive at 15 mo | 2009 | Reuter et al[49] |
| 72 | 70 | M | U | Hematuria | DLBCL | Surg | NR | 2010 | Vázquez et al[50] |
| 73 | 66 | F | U | Incidental | MALT | CTx | D's free after 3 yr | 2010 | Chatzipantelis et al[51] |
| 74 | 52 | F | U | Flank pain, hematuria | DLBCL | CTx | D's free after Tx | 2010 | Contreras-Ibáñez et al[52] |
| 75 | 32 | M | U | Heaviness, wt loss, | BCL | Surg, CTx | Died after 2 mo | 2010 | Cyriac et al[53] |
| 76 | 12 | M | U | Lumbar mass | DLBCL | CTx | D's free after 3 mo | 2010 | Gupta et al[54] |
| 77 | 48 | M | U | Abd. distension | DLBCL | CTx | D's free after Tx | 2010 | Kumar et al[55] |
| 78 | 2.5 | F | B | Abd. distension | T-LBL | CTx | D's free after Tx | 2010 | Moslemi et al[56] |
| 79 | 75 | F | B | ARF | DLBCL | CTx | NR | 2010 | Paladugu et al[57] |
| 80 | 67 | F | B | Epigastric pain, N/V | Large BCL | CTx | Alive at 4 wk | 2011 | Weng et al[58] |
| 81 | 72 | M | U | Flank pain, wt loss, | DLBCL | CTx | Alive at 15 mo | 2011 | Al-salam et al[59] |
| 82 | 7 | F | B | Fever, joint pain, anemia | NR | CTx | NR | 2011 | Al-salam et al[59] |
| 83 | 23 | M | B | ARF | TLBL | CTx | NR | 2011 | Dash et al[61] |
| 84 | 73 | M | U | Unknown | Large BCL | Surg | Unknown | 2012 | Kwakernaak et al[62] |
| 85 | 82 | F | U | Dizziness, palpitation, loss of consciousness | BCL | CTx | Unknown | 2012 | Brancato et al[63] |
| 86 | 46 | M | U | Wt loss, flank pain | DLBCL | Surg, CTx, RTx | Alive at 5 yr | 2012 | Hart et al[64] |
| 87 | 77 | F | U | Anorexia, malaise | DLBCL | Surg, CTx | Alive at 5.5 yr | 2012 | Hart et al[64] |
| 88 | 61 | M | U | ND | DLBCL | CTx | NR | 2013 | Vázquez-Alonso et al[65] |
| 89 | 77 | M | U | Hematuria | MZL | RTx | Alive at 3 yr | 2013 | Chen et al[66] |
| 90 | 12 | F | U | Hematuria | DLBCL | Surg, CTx | Alive at 3.2 yr | 2013 | Dedekam et al[67] |
| 91 | 27 | F | B | N/V, fever | DLBCL | CTx | Recurrence | 2013 | Hayakawa et al[68] |
| 92 | 39 | M | U | Pain | NHL | CTx | Remission | 2013 | Hu et al[69] |
| 93 | 64 | F | U | Wt loss | DLBCL | Surg, CTx | D's free | 2013 | Pahwa et al[3] |
| 94 | 42 | M | U | Abd pain, abd. mass | DLBCL | CTx | Alive at 28 mo | 2014 | Patel et al[70] |
| 95 | 49 | M | U | Pain, abd. mass | BCL | Surg | Alive at 1 yr | 2014 | Geetha et al[71] |
| 96 | 82 | F | U | HTN | MALT | Surg, CTx | D's free after 10 mo | 2014 | Naveen et al[72] |
| 97 | 44 | F | B | ARF | DLBCL | CTx | NR | 2015 | Vedovo et al[73] |
| 98 | 8 | ND | B | Fever, joint pain, anemia, | BCL | CTx | Alive at 1 yr | 2015 | Bahure et al[74] |
| 99 | 56 | M | U | Flank pain, fever | DLBCL | CTx, RTx | Remission | 2015 | Dhull et al[75] |
| 100 | 8 | M | U | Wt loss | DLBCL | CTx | Recurrence | 2015 | Hagihara et al[76] |
| 101 | 70 | F | U | Anorexia, malaise, fever | DLBCL | CTx | Alive at 8 mo | 2016 | Wang et al[77] |
| 102 | 19 | M | B | Hematuria | DLBCL | CTx | Alive after Tx | 2016 | Chen et al[78] |
| 103 | 72 | M | U | Incidental | FL | Surg, CTx | NR | 2016 | Erdoğmuş et al[79] |
| 104 | 50 | M | U | Dull aching pain | DLBCL | CTx | Died before 3rd CTx | 2016 | Jipp et al[80] |
| 105 | 12 | M | B | Fatigue | DLBCL | CTx | D's free after 5 yr | 2017 | Shetty et al[81] |
| 106 | 10 | M | U | Flank mass | DLBCL | CTx | Died at 14 mo | 2017 | Butani et al[82] |
| 107 | 54 | F | U | Headache | DLBCL | CTx | NR | 2017 | Coca et al[83] |
| 108 | 38 | M | B | Flank pain | DLBCL | NR | NR | 2017 | Rissman et al[84] |
| 109 | 64 | F | U | Abd. pain | DLBCL | CTx | NR | 2017 | Saddadi et al[85] |
| 110 | 51 | M | U | Flank pain | DLBCL | Surg | D's free after Tx | 2018 | Thawani et al[86] |
| 111 | 37 | M | B | Hematuria | DLBCL | CTx | Died prior to CTx | 2018 | Agochukwu et al[87] |
| 112 | 4 | M | B | Fatigue | DLBCL | CTx | D's free after 4 yr | 2018 | Mustafar et al[88] |
| 113 | 64 | F | U | Frequency | DLBCL | Surg, CTx | NR | 2019 | South et al[89] |
| 114 | 78 | M | U | Abd. pain | DLBCL | Surg | Died during Tx | 2019 | Cheng et al[90] |
| 115 | 79 | M | U | Myalgia | DLBCL | NR | NR | 2019 | Li et al[91] |
| 116 | 50 | M | U | Flank pain | DLBCL | CTx, RTx | CR | 2022 | Silverman et al[92] |
| 117 | 56 | F | U | Back pain, hematuria | DLBCL | CTx | D's free after 1 yr | 2022 | Nasrollahi et al[93] |
| 118 | 59 | M | U | Back pain | BCL | CTx | CR | 2022 | He et al[94] |
| 119 | 53 | ND | B | Back pain, ARF | MZL | CTx | Under Tx | 2023 | Abdi et al[95] |
| 120 | 56 | F | U | Incidental | HG BCL | CTx | D's free | 2023 | Benmoussa et al[96] |
| 121 | 74 | F | B | ARF | DLBCL | CTx | Died at 3rd CTx | Present case | |
Renal lymphoma can present as a solitary mass (10%-25% of cases) or multiple parenchymal nodular masses of variable sizes, typically 1.0 to 4.5 cm in diameter, which is the most common pattern in approximately 50%-60% of cases. The second most common pattern is a retroperitoneal nodular lesion with continuous extension into the kidneys or perinephric space (observed in 25%-30% of cases). Diffuse renal enlargement without distortion of kidney shape or formation of any discrete masses was found in 6%-19%[102]. The unilateral masses and grossly nodular forms are relatively easily detected by US or CT; therefore, when necessary, the patients undergo open renal biopsy or nephrectomy. On the contrary, bilateral diffuse infiltrative lesions are difficult to detect by radiologic examination. Furthermore, due to various symptoms of lymphomatous infiltration, they are often mistaken for medical renal disease, and frequently percutaneous needle biopsy is performed for confirmative diagnosis. In our case, no definite mass-like lesion was identified on abdominal CT due to bilateral diffuse involvement of PRL, and a sono-guided percutaneous needle biopsy was performed to diagnose RPGN, clinically. In this case, based on the clinical and radiological background, renal involvement of malignant lymphoma could not be suspected.
Of all 121 patients, 96 had the following prognostic data: 68 (56.2%) patients survived, 21 (17.4%) died during/before/shortly after treatment, and 5 (4.1%) had relapsed disease. The mortality rate was especially high in patients younger than 10 years of age at 45.5%, and was 30.4% and 14.3% for those aged < 40 and ≥ 40 years, respectively. In addition, when the mortality rate was stratified by the location of the tumor, 41.7% (15/36) of patients demonstrated bilateral involvement whereas 7.2% (6/83) had unilateral lesions. Younger patients and those with bilateral PRL had a shorter survival time and more rapid disease progression compared to older individuals. Therefore, special procedures should be considered for the patients mentioned above, including a combination of surgery, CTx, or radiotherapy (RTx).
To date, CTx remains the main treatment for PRL. Among these 121 cases, 99 (81.8%) were treated with CTx (CTx alone or in combination), 67 (55.4%) with single CTx, and the remainder received various combination therapies including RTx, surgery, stem cell transplantation, and surgery. Regardless of the treatment, the overall mortality rate was 17.1%. When classified according to the treatment, the mortality rate of patients on single CTx was 21.2% (14/66), whereas, with combined therapy, a much lower mortality rate was observed [surgery with CTx, 12.5% (3/24); no treatment, 1 case; steroid treatment, 1 case; surgery, 1 case; surgery n with concurrent chemoradiation therapy and CTx with stem cell transplantation, no death]. Apart from single CTx, the number of patients on other therapies was small; therefore, this result should be interpreted with caution. To date, CTx remains the most-preferred treatment; however, a combination of CTx with RTx, surgery, and other methods should be considered in young patients or those with bilateral PRL.
Using the IPI, 4 independent patient risk groups with any combination of the following five clinical variables were identified, including age, LDH level, tumor stage, ECOG-PS, and extranodal sites of disease[103]. Moreover, the IPI has been widely used in clinical applications and is the standard practical prognostic tool for patients with DLBCL. In our case, the IPI was 3 (old age, 1; ECOG-PS, 1; Ann Arbor stages III–IV, 0; LDH > 1 × normal, 1; and > 1 extranodal site, 0). In addition to the IPI, because the correlation between cancer and inflammation has received attention in recent years, the prognostic significance of platelet/lymphocyte ratio (PLR) and neutrophil/lymphocyte ratio (NLR) in DLBCL has been reported in several studies[104]. For nearly all oncology records, PLR and NLR are calculated and routinely investigated from platelets, lymphocytes, and neutrophil counts. They are easily available measures in daily clinical practice, are inexpensive, and can provide useful prognostic information for the management of DLBCL[104]. Wang et al[104] reported markedly short OS and progression-free survival in patients with higher NLR and PLR compared with those with low NLR and PLR. Patients with a high NLR exhibit significantly low ECOG-PS, a high disease stage, and B symptoms, more extranodal sites of disease, and high IPI and LDH levels at diagnosis. Patients with a high PLR more frequently displayed significantly low ECOG-PS and B symptoms and a high LDH level at diagnosis. This revealed that patients with a PLR < 150 or NLR < 2.32 at diagnosis experienced better relapse-free survival and OS than those with a PLR ≥ 150 or NLR ≥ 2.32. In their study, NLR displayed no significant difference in multivariate analysis; however, univariate and multivariate analysis confirmed the predictive ability of PLR, indicating that PLR may be superior to NLR as a prognostic factor for DLBCL. In the present case, the pretreatment PLR was 186 (≥ 150) and NLR was 8.23 (≥ 2.32), implying a poor prognosis [platelets, 279000/µL; lymphocytes, 1500/µL; lymphocytes (%), 18.2%; and neutrophils (%), 67.2%].
This literature review had several limitations. Most importantly, all follow-up data were obtained from different article references and therefore have different follow-up periods. Thus, further studies are required regarding the prognosis of the disease.
Pathological diagnosis is important for the early diagnosis of PRL. When PRL shows bilateral and diffuse patterns, as in our case, predicting the diagnosis based on clinical and biochemical characteristics may be difficult, as PRL may clinically mimic refractory medical renal disease. Thus, a kidney biopsy would be required for confirmation of a radiologic or clinically suspected lymphoma. A biopsy is essential following a diagnosis of renal lymphoma, especially PRL, to institute early treatment, to achieve a cure in patients. Additionally, kidney biopsy helps confirm the exact subtype of lymphoma to apply appropriate treatment.
In conclusion, we report a 74-year-old patient with PRL presenting with AKI, and we conducted a literature review of 121 cases of PRL since 1989, to report their clinicopathologic findings. The literature search demonstrated that bilateral PRL is rare and has a poor prognosis. Among the 121 cases, only 36 were bilateral PRL, similar to our case. Additionally, AKI occurred in all bilateral PRL cases, and 71.4% of patients who died were diagnosed with bilateral PRL. Therefore, a need to discuss more active treatment for bilateral PRL is necessary. Moreover, bilateral renal involvement in malignant lymphoma can cause AKI. In particular, differentiating diffuse involvement (rather than the nodular form) clinically or radiologically from other kidney diseases that causes AKI is difficult; therefore, a kidney biopsy is essential for the diagnosis of renal lymphoma. Thus, clinicians should endeavor to make a preoperative diagnosis, to avoid unnecessary surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Long X, China; Ohashi N, Japan; Tang H, China S-Editor: Qu XL L-Editor: Webster JR P-Editor: Yu HG
| 1. | Tefekli A, Baykal M, Binbay M, Barut M, Muslumanoglu AY. Lymphoma of the kidney: primary or initial manifestation of rapidly progressive systemic disease? Int Urol Nephrol. 2006;38:775-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Paganelli E, Arisi L, Ferrari ME, Olivetti G, Tedeschi F. Primary non-Hodgkin's lymphoma of the kidney. Haematologica. 1989;74:301-304. [PubMed] |
| 3. | Pahwa M, Gupta N, Tyagi V, Chadha S. Primary renal lymphoma: is prognosis really that bad? Saudi J Kidney Dis Transpl. 2013;24:816-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Ladha A, Haider G. Primary renal lymphoma. J Coll Physicians Surg Pak. 2008;18:584-585. [PubMed] |
| 5. | Stallone G, Infante B, Manno C, Campobasso N, Pannarale G, Schena FP. Primary renal lymphoma does exist: case report and review of the literature. J Nephrol. 2000;13:367-372. [PubMed] |
| 6. | El-Sharkawy MS, Siddiqui N, Aleem A, Diab AA. Renal involvement in lymphoma: prevalence and various patterns of involvement on abdominal CT. Int Urol Nephrol. 2007;39:929-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Madaio MP. Renal biopsy. Kidney Int. 1990;38:529-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 121] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Taneja A, Kumar V, Chandra AB. Primary renal lymphoma: A population-based analysis using the SEER program (1973-2015). Eur J Haematol. 2020;104:390-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | van Gelder T, Michiels JJ, Mulder AH, Klooswijk AI, Schalekamp MA. Renal insufficiency due to bilateral primary renal lymphoma. Nephron. 1992;60:108-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Salem Y, Pagliaro LC, Manyak MJ. Primary small noncleaved cell lymphoma of kidney. Urology. 1993;42:331-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Arranz Arija JA, Carrion JR, Garcia FR, Tejedor A, Pérez-Manga G, Tardio J, Menarguez FJ. Primary renal lymphoma: report of 3 cases and review of the literature. Am J Nephrol. 1994;14:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Okuno SH, Hoyer JD, Ristow K, Witzig TE. Primary renal non-Hodgkin's lymphoma. An unusual extranodal site. Cancer. 1995;75:2258-2261. [PubMed] [DOI] [Full Text] |
| 13. | Chin KC, Perry GJ, Dowling JP, Thomson NM. Primary T-cell-rich B-cell lymphoma in the kidney presenting with acute renal failure and a second malignancy. Pathology. 1999;31:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Colović M, Hadzi-Djokić J, Cemerikić V, Colović R, Janković G, Dacić M. Primary MALT lymphoma of the kidney. Hematol Cell Ther. 1999;41:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Mhawech P, Ahearn J, Medeiros LJ. Pathologic quiz case. A unilateral renal mass in an elderly woman. Arch Pathol Lab Med. 2000;124:919-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Jindal B, Sharma SC, Das A, Banerjee AK. Indolent behaviour of low-grade B cell lymphoma of mucosa-associated lymphoid tissue arising in the kidney. Urol Int. 2001;67:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | O'Riordan E, Reeve R, Houghton JB, O'Donoghue DJ, Waldek S. Primary bilateral T-cell renal lymphoma presenting with sudden loss of renal function. Nephrol Dial Transplant. 2001;16:1487-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Gellrich J, Hakenberg OW, Naumann R, Manseck A, Lossnitzer A, Wirth MP. Primary renal non-Hodgkin's lymphoma - a difficult differential diagnosis. Onkologie. 2002;25:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Levendoglu-Tugal O, Kroop S, Rozenblit GN, Weiss R. Primary renal lymphoma and hypercalcemia in a child. Leuk Lymphoma. 2002;43:1141-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Mansouri H, Gaye M, Hassouni K, Errihani H, Kettani F, El Gueddari B. An unusual primary renal lymphoma. Urol Int. 2002;69:153-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Mita K, Ohnishi Y, Edahiro T, Fujii T, Yamasaki A, Shimamoto F. Primary mucosa-associated lymphoid tissue lymphoma in the renal pelvis. Urol Int. 2002;69:241-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Stokes MB, Wood B, Alpers ChE. Membranoproliferative glomerulonephritis associated with low-grade B cell lymphoma presenting in the kidney. Clin Nephrol. 2002;57:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | O'Sullivan AW, Lee G, Fitzgerald E, O'Sullivan GC. Bilateral primary renal lymphoma. Ir J Med Sci. 2003;172:44-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Olusanya AA, Huff G, Adeleye O, Faulkner M, Burnette R, Thompson H, Adeola T, Woods K. Primary renal non-Hodgkins lymphoma presenting with acute renal failure. J Natl Med Assoc. 2003;95:220-224. [PubMed] |
| 25. | Pervez H, Shaikh M, Potti A, Mehdi SA. Uncommon presentations of non-Hodgkin's lymphoma: case 3. Primary renal lymphoma. J Clin Oncol. 2003;21:567-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Tuzel E, Mungan MU, Yorukoglu K, Basakci A, Kirkali Z. Primary renal lymphoma of mucosa-associated lymphoid tissue. Urology. 2003;61:463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Cupisti A, Riccioni R, Carulli G, Paoletti S, Tognetti A, Meola M, Francesca F, Barsotti G, Petrini M. Bilateral primary renal lymphoma treated by surgery and chemotherapy. Nephrol Dial Transplant. 2004;19:1629-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Ozaltin F, Yalçin B, Orhan D, Sari N, Caglar M, Besbas N, Bakkaloglu A. An unusual cause of acute renal failure: renal lymphoma. Pediatr Nephrol. 2004;19:912-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Zomas A, Leivada A, Gortzolidis G, Michalis E, Skandalis A, Anagnostopoulos NI. Primary renal lymphoma presenting with chronic low-grade fever. Int J Hematol. 2004;79:361-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Ahmad AH, Maclennan GT, Listinsky C. Primary renal lymphoma: a rare neoplasm that may present as a primary renal mass. J Urol. 2005;173:239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Kaya A, Kanbay M, Bayrak O, Eken G, Memis L, Akcay A, Duranay M. Primary renal lymphoma associated with hepatitis C virus infection. Leuk Lymphoma. 2006;47:1976-1978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Bozas G, Tassidou A, Moulopoulos LA, Constandinidis C, Bamias A, Dimopoulos MA. Non-Hodgkin's lymphoma of the renal pelvis. Clin Lymphoma Myeloma. 2006;6:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Guilpain P, Delarue R, Matignon M, Noël LH, Knebelmann B, Fakhouri F. Primary bilateral diffuse renal lymphoma. Am J Hematol. 2006;81:804-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Qiu L, Unger PD, Dillon RW, Strauchen JA. Low-grade mucosa-associated lymphoid tissue lymphoma involving the kidney: report of 3 cases and review of the literature. Arch Pathol Lab Med. 2006;130:86-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Sharma SB, Debnath PR, Tripathi R. Primary renal lymphoma in a child. Indian J Pediatr. 2006;73:947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Valarmathi K, Jamila A, Ravi S, Selvambigai, Muthulatha. A rare case of renal tumour. J Clin Diagn Res. 2013;7:2006-2007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 37. | Becker AM, Bowers DC, Margraf LR, Emmons J, Baum M. Primary renal lymphoma presenting with hypertension. Pediatr Blood Cancer. 2007;48:711-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Diskin CJ, Stokes TJ, Dansby LM, Radcliff L, Carter TB, Graves E, Byron D, Cook WJ. Acute renal failure due to a primary renal B-cell lymphoma. Am J Kidney Dis. 2007;50:885-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | Fang FS, Zhu HL, Song ZG, Lu XC. [Three cases of primary renal lymphoma]. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2007;15:1107-1111. [PubMed] [DOI] [Full Text] |
| 40. | Garcia M, Konoplev S, Morosan C, Abruzzo LV, Bueso-Ramos CE, Medeiros LJ. MALT lymphoma involving the kidney: a report of 10 cases and review of the literature. Am J Clin Pathol. 2007;128:464-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Omer HA, Hussein MR. Primary renal lymphoma. Nephrology (Carlton). 2007;12:314-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 42. | Rajappa S, Digumarti R, Immaneni SR, Parage M. Primary renal lymphoma presenting with paraneoplastic limbic encephalitis. J Clin Oncol. 2007;25:3783-3785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 43. | James TC, Shaikh H, Escuadro L, Villano JL. Bilateral primary renal lymphoma. Br J Haematol. 2008;143:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 44. | Kuo CC, Li WY, Huang CC, Lin WC, Chen YM. Primary renal lymphoma. Br J Haematol. 2009;144:628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Jindal B, Agarwala S, Bakhshi S, Jain V, Gupta AK, Kumar R, Bal CS, Iyer VK, Gupta SD. Bilateral primary renal lymphoma with orbital metastasis in a child. Pediatr Blood Cancer. 2009;52:539-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Kose F, Sakalli H, Mertsoylu H, Sezer A, Kocer E, Tokmak N, Kilinc F, Ozyilkan O. Primary renal lymphoma: report of four cases. Onkologie. 2009;32:200-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Pinggera GM, Peschel R, Buttazzoni A, Mitterberger M, Friedrich A, Pallwein L. A possible case of primary renal lymphoma: a case report. Cases J. 2009;2:6233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Renaud J, Yartsev S, Dar AR, Van Dyk J. Successful treatment of primary renal lymphoma using image guided helical tomotherapy. Can J Urol. 2009;16:4639-4647. [PubMed] |
| 49. | Reuter S, Rahbar K, Busch V, Hillebrand U, Velden J, Pavenstädt H, Schober O, Stegger L. Acute renal failure due to primary bilateral renal large B-cell lymphoma: diagnostics and follow-up by FDG-PET/CT. Clin Nucl Med. 2009;34:722-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 50. | Vázquez Alonso F, Sánchez Ramos C, Vicente Prados FJ, Pascual Geler M, Ruiz Carazo E, Becerra Massare P, Funes Padilla C, Rodríguez Herrera F, Cózar Olmo JM, Tallada Buñuel M. Primary renal lymphoma: report of three new cases and literature review. Arch Esp Urol. 2009;62:461-465. [PubMed] |
| 51. | Chatzipantelis P, Mastorakis E, Tzortzakakis D, Salla C. Fine needle aspiration cytology diagnosis of primary renal lymphoma involving the pleura: a case report. Acta Cytol. 2010;54:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Contreras-Ibáñez JA, Díaz-Gómez L, Muriel-Cueto P. [Renal synchronous carcinoma of clear cells with non-hodgkin lymphoma of phenotype b of type MALT]. Actas Urol Esp. 2010;34:818-819. [PubMed] |
| 53. | Cyriac S, Rejiv R, Shirley S, Sagar GT. Primary renal lymphoma mimicking renal cell carcinoma. Indian J Urol. 2010;26:441-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 54. | Gupta A, Bhatt A, Khaira A, Gupta A, Ran DS. Primary renal lymphoma: a differential diagnosis of renal mass in a young male. Saudi J Kidney Dis Transpl. 2010;21:544-545. [PubMed] |
| 55. | Kumar D, Sharma P, Agarwala S, Thulkar S, Tanveer N, Bakhshi S. Pediatric renal non-hodgkin lymphoma with inferior vena cava thrombosis. J Pediatr Hematol Oncol. 2010;32:147-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 56. | Moslemi MK, Tahvildar SA, Ashtari AA. Primary Lymphoma of the Kidney in an Adult Male - The First Reported Case from Iran. Case Rep Oncol. 2010;3:72-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 57. | Paladugu S, Garro R, Schrijver I, Kambham N, Higgins JP. A 30-month-old child with acute renal failure due to primary renal cytotoxic T-cell lymphoma. Am J Surg Pathol. 2010;34:1066-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 58. | Weng SC, Shu KH, Wen MC, Cheng CH, Wu MJ, Yu TM, Chuang YW, Chen CH. Malignant lymphoma of the kidney mimicking rapid progressive glomerulonephritis. Clin Nephrol. 2010;74:480-484. [PubMed] |
| 59. | Al-Salam S, Shaaban A, Alketbi M, Haq NU, Abouchacra S. Acute kidney injury secondary to renal large B-cell lymphoma: role of early renal biopsy. Int Urol Nephrol. 2011;43:237-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 60. | Belbaraka R, Elyoubi MB, Boutayeb S, Errihani H. Primary renal non-Hodgkin lymphoma: an unusual diagnosis for a renal mass. Indian J Cancer. 2011;48:255-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Dash SC, Purohit K, Mohanty SK, Dinda AK. An unusual case of bilateral renal enlargement due to primary renal lymphoma. Indian J Nephrol. 2011;21:56-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 62. | Kwakernaak AJ, Hazenberg MD, Roelofs JJ, van Noesel CJ, van Oers MH, van Tellingen A. Precursor T-lymphoblastic lymphoma presenting as primary renal lymphoma with acute renal failure. NDT Plus. 2011;4:289-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 63. | Brancato T, Alvaro R, Paulis G, Nupieri P, D'Ascenzo R, Orsolini G. Primary lymphoma of the kidney: case report and review of literature. Clin Genitourin Cancer. 2012;10:60-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 64. | Hart S, Ellimoottil C, Shafer D, Mehta V, Turk TM. A case of primary renal lymphoma. Urology. 2012;80:763-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Vázquez-Alonso F, Puche-Sanz I, Sánchez-Ramos C, Flores-Martín J, Vicente-Prados J, Cózar-Olmo JM. Primary renal lymphoma: long-term results of two patients treated with a chemotherapy + rituximab protocol. Case Rep Oncol Med. 2012;2012:726424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 66. | Chen L, Richendollar B, Bunting S, Campbell S, Zhou M. Lymphomas and lymphoproliferative disorders clinically presenting as renal carcinoma: a clinicopathological study of 14 cases. Pathology. 2013;45:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 67. | Dedekam E, Graham J, Strenge K, Mosier AD. Primary renal lymphoma mimicking a subcapsular hematoma: a case report. J Radiol Case Rep. 2013;7:18-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 68. | Hayakawa A, Shimotake N, Kubokawa I, Mitsuda Y, Mori T, Yanai T, Muramaki M, Miyake H, Fujisawa M, Iijima K. Primary pediatric stage III renal diffuse large B-cell lymphoma. Am J Case Rep. 2013;14:34-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 69. | Hu R, Zhang R, Miao M, Zhu K, Yang W, Liu Z. Central nervous system involvement of primary renal lymphoma with diffuse large B-cell type lymphoma. Am J Case Rep. 2013;14:292-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 70. | Patel S, Kramer N, Cohen AJ, Rosenstein ED. Renal lymphoma: unusual lymphoproliferative manifestation of Sjogren's syndrome. J Rheumatol. 2013;40:102-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 71. | Geetha N, Shahid A, Rajan V, Jacob PM. Primary renal lymphoma-a case report. Ecancermedicalscience. 2014;8:466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 72. | Naveen Kumar BJ, Barman P, Chowdhury N, Bora M. Primary renal lymphoma: An unusual presentation of non-Hodgkin's lymphoma. Indian J Cancer. 2014;51:370-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 73. | Vedovo F, Pavan N, Liguori G, Siracusano S, Bussani R, Trombetta C. Primary renal MALToma: A rare differential diagnosis for a recurrent renal mass after primary ablative therapy. Can Urol Assoc J. 2014;8:E442-E444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 74. | Bahure S, Cheung JC, Lin M. Utility of FDG-PET in primary renal lymphoma. Clin Exp Nephrol. 2015;19:158-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 75. | Dhull VS, Mukherjee A, Karunanithi S, Durgapal P, Bal C, Kumar R. Bilateral primary renal lymphoma in a pediatric patient: staging and response evaluation with ¹⁸F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol. 2015;34:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 76. | Hagihara M, Hua J, Iwaki Y, Inoue M, Sato T. Primary renal lymphoma: a case report and literature review. Intern Med. 2015;54:2655-2659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 77. | Wang Y, Guo S. Primary renal diffuse large B-cell lymphoma with central nervous system involvement: a rare case report and literature review. Int J Clin Exp Pathol. 2015;8:7045-7049. [PubMed] |
| 78. | Chen X, Hu D, Fang L, Chen Y, Che X, Tao J, Weng G, Ye X. Primary renal lymphoma: A case report and literature review. Oncol Lett. 2016;12:4001-4008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 79. | Erdoğmuş Ş, Aktürk S, Kendi Çelebi Z, Kiremitçi S, Kaygusuz G, Altınbaş NK, Üstüner E, Keven K. Diffuse Large B-Cell Lymphoma Presenting with Bilateral Renal Masses and Hematuria: A Case Report. Turk J Haematol. 2016;33:159-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 80. | Jipp J, Sadowski D, Kay P, Schwartz B. Primary Renal Lymphoma Identified in a Robot-Assisted Laparoscopic Nephroureterectomy Specimen. J Endourol Case Rep. 2016;2:96-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 81. | Shetty S, Singh AC, Babu V. Primary Renal Lymphoma - A Case Report and Review of Literature. J Clin Diagn Res. 2016;10:XD05-XD07. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 82. | Butani L, Ducore J. Primary Renal Lymphoma Presenting as End-Stage Renal Disease. Case Rep Med. 2017;2017:9210648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 83. | Coca P, Linga VG, Gundeti S, Tandon A. Renal Lymphoma: Primary or First Manifestation of Aggressive Pediatric B-cell Lymphoma. Indian J Med Paediatr Oncol. 2017;38:538-541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 84. | Rissman CM, Dagrosa LM, Pettus JR, Dillon JL, Sverrisson EF. Primary renal lymphoma: an unusual finding following radical nephrectomy. Clin Nephrol Case Stud. 2017;5:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 85. | Saddadi F, Sabzevari A, Asgari M. Uncommon Presentation of Primary Renal Lymphoma. Iran J Kidney Dis. 2017;11:344. [PubMed] |
| 86. | Thawani R, Amar A, Patowary J, Kaul S, Jena A, Das PK. Primary Renal Cell Lymphoma: Case Report, Diagnosis, and Management. Indian J Med Paediatr Oncol. 2017;38:545-547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 87. | Agochukwu NQ, Kilchevsky A, Hesse D. Primary renal large B-cell lymphoma imitating invasive renal cell carcinoma with inferior vena cava tumor thrombus. Urol Case Rep. 2018;18:84-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 88. | Mustafar R, Kamaruzaman L, Chien BH, Yahaya A, Mohd Nasir N, Mohd R, Cader R, Wei Yen K. A Rare Cause of Acute Kidney Injury: Primary Renal Lymphoma in a Patient with Human Immunodeficiency Virus. Case Rep Med. 2018;2018:8425985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 89. | South AM. Primary renal diffuse large B-Cell lymphoma causing haemodialysis-dependent nephromegaly in a child. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 90. | Cheng X, Huang Z, Li D, Wang Y. Enormous primary renal diffuse large B-cell lymphoma: A case report and literature review. J Int Med Res. 2019;47:2728-2739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 91. | Li J, Zou Y, Wang B, Meng X, Sun X. Concomitant occurrence of primary renal non-Hodgkin lymphoma and a colon cancer: A rare case report. Medicine (Baltimore). 2019;98:e14802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 92. | Silverman B, Levy J, Vagasi AS, Purrazzella R, Andaz S. Primary renal lymphoma: An incidental finding in an elderly male. Urol Case Rep. 2019;26:100965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 93. | Nasrollahi H, Eslahi A, Ahmed F, Geramizadeh B, Ansari M. Primary diffuse large B-cell lymphoma of the right kidney: a case report. Pan Afr Med J. 2022;42:269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 94. | He J, Mu Y, Che BW, Liu M, Zhang WJ, Xu SH, Tang KF. Comprehensive treatment for primary right renal diffuse large B-cell lymphoma with a renal vein tumor thrombus: A case report. World J Clin Cases. 2022;10:5352-5358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 95. | Abdi EM, Afifi MA, Moataz A, Dakir M, Debbagh A, Aboutaieb R. Primary renal lymphoma in an immunocompetent patient. Urol Case Rep. 2022;44:102140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 96. | Benmoussa A, Moukrim I, Khoubila N, Cherkaoui S, Lmchaheb M, Qachouh M, Rachid M, Madani A. [Primary renal marginal zone B lymphoma]. Rev Med Liege. 2023;78:121-123. [PubMed] |
| 97. | Bhat AS, Dsouza LJ, Gatty RC, Shet DS. Primary renal lymphoma masquerading as metastasis in a patient with primary breast cancer and systemic lupus erythematosus. Indian J Cancer. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 98. | Zhao K, Zhang Q, Cong R, Wang Y, Wang Z, Song N. Primary renal lymphoma: a case report and review of the literature. AME Case Rep. 2020;4:8. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 99. | Geramizadeh B, Shojazadeh A, Marzban M. Primary renal non-Hodgkin's lymphoma: A narrative review of literature. Urologia. 2022;89:185-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 100. | Coggins CH. Renal failure in lymphoma. Kidney Int. 1980;17:847-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 101. | Bridoux F, Cockwell P, Glezerman I, Gutgarts V, Hogan JJ, Jhaveri KD, Joly F, Nasr SH, Sawinski D, Leung N. Kidney injury and disease in patients with haematological malignancies. Nat Rev Nephrol. 2021;17:386-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 102. | Bokhari MR, Rana UI, Bokhari SRA. Renal Lymphoma. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 103. | Wang H, Shao R, Liu W, Tang H, Lu Y. Identification of a prognostic metabolic gene signature in diffuse large B-cell lymphoma. J Cell Mol Med. 2021;25:7066-7077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 104. | Wang S, Ma Y, Sun L, Shi Y, Jiang S, Yu K, Zhou S. Prognostic Significance of Pretreatment Neutrophil/Lymphocyte Ratio and Platelet/Lymphocyte Ratio in Patients with Diffuse Large B-Cell Lymphoma. Biomed Res Int. 2018;2018:9651254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |