Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6955
Peer-review started: July 28, 2023
First decision: August 17, 2023
Revised: August 29, 2023
Accepted: September 4, 2023
Article in press: September 4, 2023
Published online: October 6, 2023
Processing time: 58 Days and 22.5 Hours
Wandering spleen is rare clinically. It is characterized by displacement of the spleen in the abdominal and pelvic cavities and can have congenital or acquired causes. Wandering spleen involves serious complications, such as spleen torsion. The clinical symptoms range from asymptomatic abdominal mass to acute abdominal pain. Surgery is required after diagnosis. Cases of wandering spleen torsion with portal vein thrombosis (PVT) are rare. There is no report on how to eliminate PVT in such cases.
Ultrasound and computed tomography revealed a diagnosis of wandering spleen torsion with PVT in a 31-year-old woman with a history of childbirth 16 mo previously who received emergency treatment for upper abdominal pain. She recovered well after splenectomy and portal vein thrombectomy combined with continuous anticoagulation, and the PVT disappeared.
Rare and nonspecific conditions, such as wandering splenic torsion with PVT, must be diagnosed and treated early. Patients with complete splenic infarction require splenectomy. Anticoagulation therapy and individualized management for PVT is feasible.
Core Tip: Cases of wandering spleen torsion with portal vein thrombosis (PVT) are rare. There is no report on how to eliminate PVT in such cases. Here, we report wandering spleen torsion with PVT in a 31-year-old woman with a history of childbirth 16 mo previously who recovered well after splenectomy and portal vein thrombectomy combined with continuous anticoagulation. The PVT disappeared. Wandering splenic torsion with PVT must be diagnosed and treated early. Patients with complete splenic infarction require splenectomy. Anticoagulation therapy and individualized management for PVT is feasible.
- Citation: Zhu XY, Ji DX, Shi WZ, Fu YW, Zhang DK. Wandering spleen torsion with portal vein thrombosis: A case report. World J Clin Cases 2023; 11(28): 6955-6960
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6955.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6955
Wandering spleen is caused by a congenital or acquired defect in the attachment of the spleen. Children aged 3 mo to 10 years and women aged 20-40 years are more likely to experience wandering spleen[1]. The overall incidence among the population is < 0.2%[2]. The clinical manifestations include an active abdominal mass, chronic pain, and acute abdominal pain, or the individual may have no symptoms. A serious complication of a wandering spleen is splenic torsion. Patients with complete splenic torsion require emergency splenectomy, which includes both traditional surgical resection and laparoscopic splenectomy. Wandering spleen torsion with portal vein thrombosis (PVT) is a rarer condition. Only two cases have been reported in Turkey, but there was no detail about the treatment and prognosis of PVT. Here, we report the first case where PVT completely disappeared with low-molecular-weight heparin treatment after portal vein (PV) incision and thrombectomy in a patient with wandering spleen torsion with PVT.
A 31-year-old woman presented to the emergency department with upper left epigastric pain that had lasted 24 h.
Symptoms started 24 h before presentation with upper left epigastric pain associated with several episodes of vomiting. The onset of symptoms was gradual.
The patient had a history of childbirth 16 mo previously.
The personal and family history revealed no information relevant to the current case.
The patient’s temperature was 36.8 ℃, heart rate was 95 beats/min, respiratory rate was 22 breaths/min, and blood pressure was 117/72 mmHg. The physical examination showed a large, firm, and mobile mass in the left lower abdomen, without any other pathological signs.
The laboratory tests showed that leukocyte count was 16 × 109/L (normal range: 3.5 × 109-9.5 × 109/L), suggesting leukocytosis; neutrophil count was 11.91 × 109/L (normal range: 1.8 × 109-6.3 × 109/L), suggesting neutrophilia; platelet count was 185 × 109/L (normal range: 125 × 109-350 × 109/L); prothrombin time was 14.4 s (normal range: 9.4 s-12.5 s); activated partial thromboplastin time was 30.8 s (normal range: 25.4 s-38.4 s); fibrin degradation products was 12.31 μg/mL (normal range: < 5 μg/mL); D-dimer was 2017 ng/mL (normal range: < 250 ng/mL); albumin was 36.4 g/L (normal range: 65 g/L-85 g/L); alanine aminotransferase was 12 U/L (normal range: 7 U/L-40 U/L); glutamic oxaloacetic transaminase was 38 U/L (normal range: 13 U/L-35 U/L); alkaline phosphatase was 79 U/L (normal range: 35 U/L-100 U/L); glutamyltransferase was 9 U/L(normal range: 7 U/L-45 U/L); total bilirubin was 15.1 μmol/L (normal range: 3.4 μmol/L-23.3 μmol/L); and direct bilirubin was 5.7 μmol/L (normal range: 0 μmol/L-6.8 μmol/L).
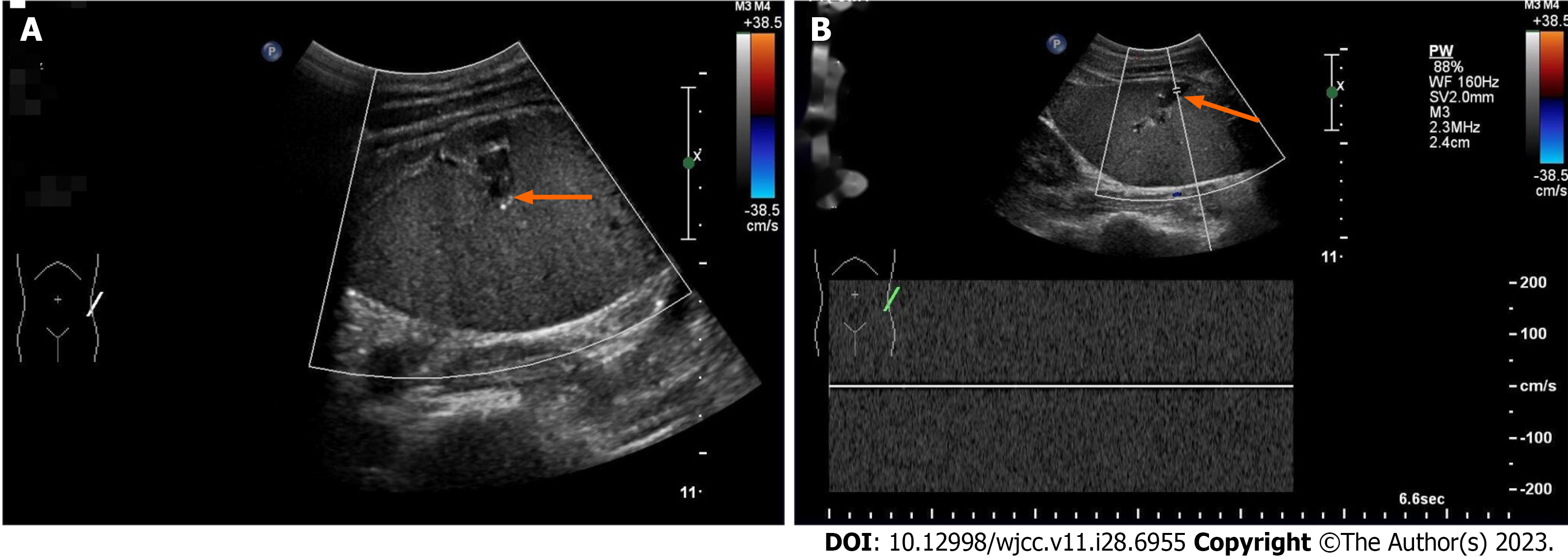
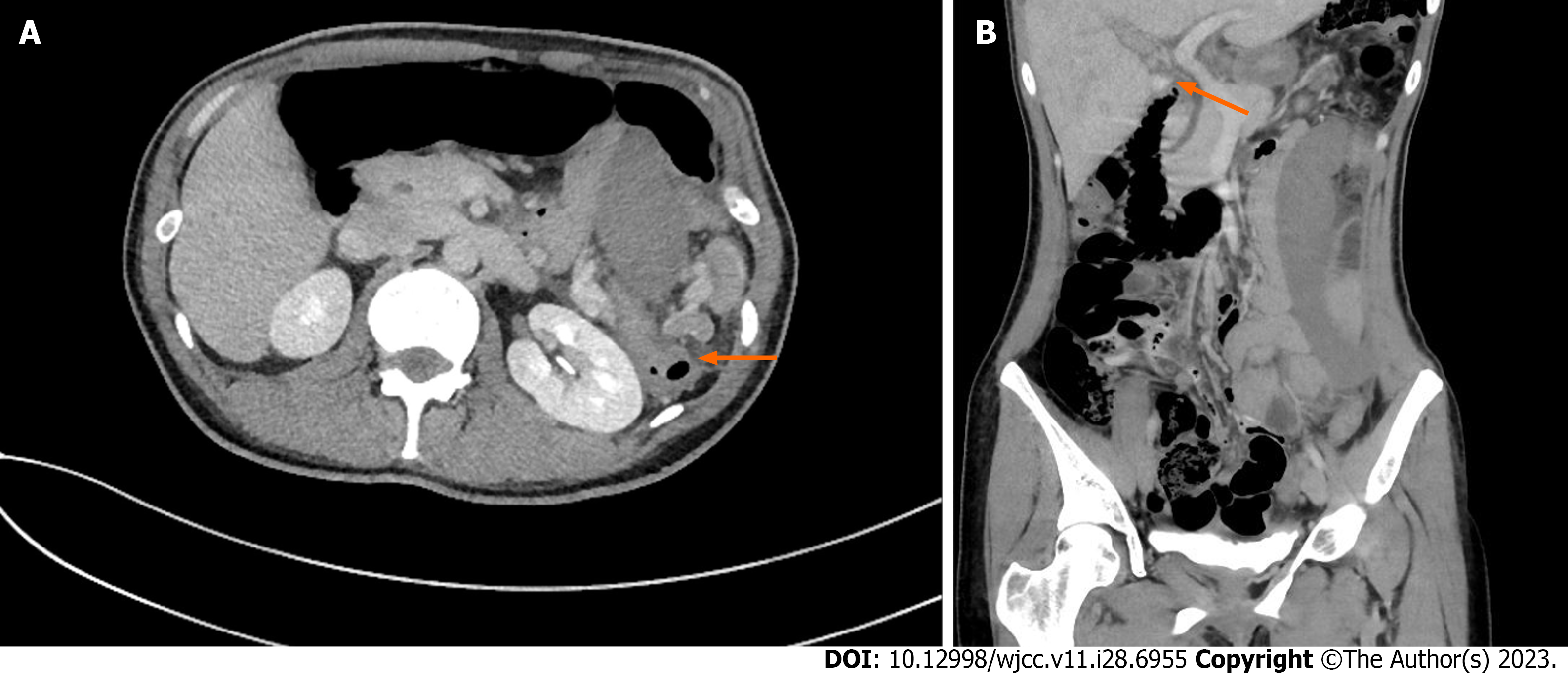
Abdominal ultrasound revealed thrombosis, a spleen located in the left lower abdomen, and a dilated splenic vein (Figure 1). Abdominal and pelvic enhanced computed tomography (CT) showed that the spleen measured 16 cm along its long axis, was located in the left lower abdomen and was not enhanced after contrast injection. The splenic pedicle of the artery and vein showed a vortex sign, and the main and right PV branches were filled with defects. This indicated wandering spleen torsion with PVT (Figure 2).
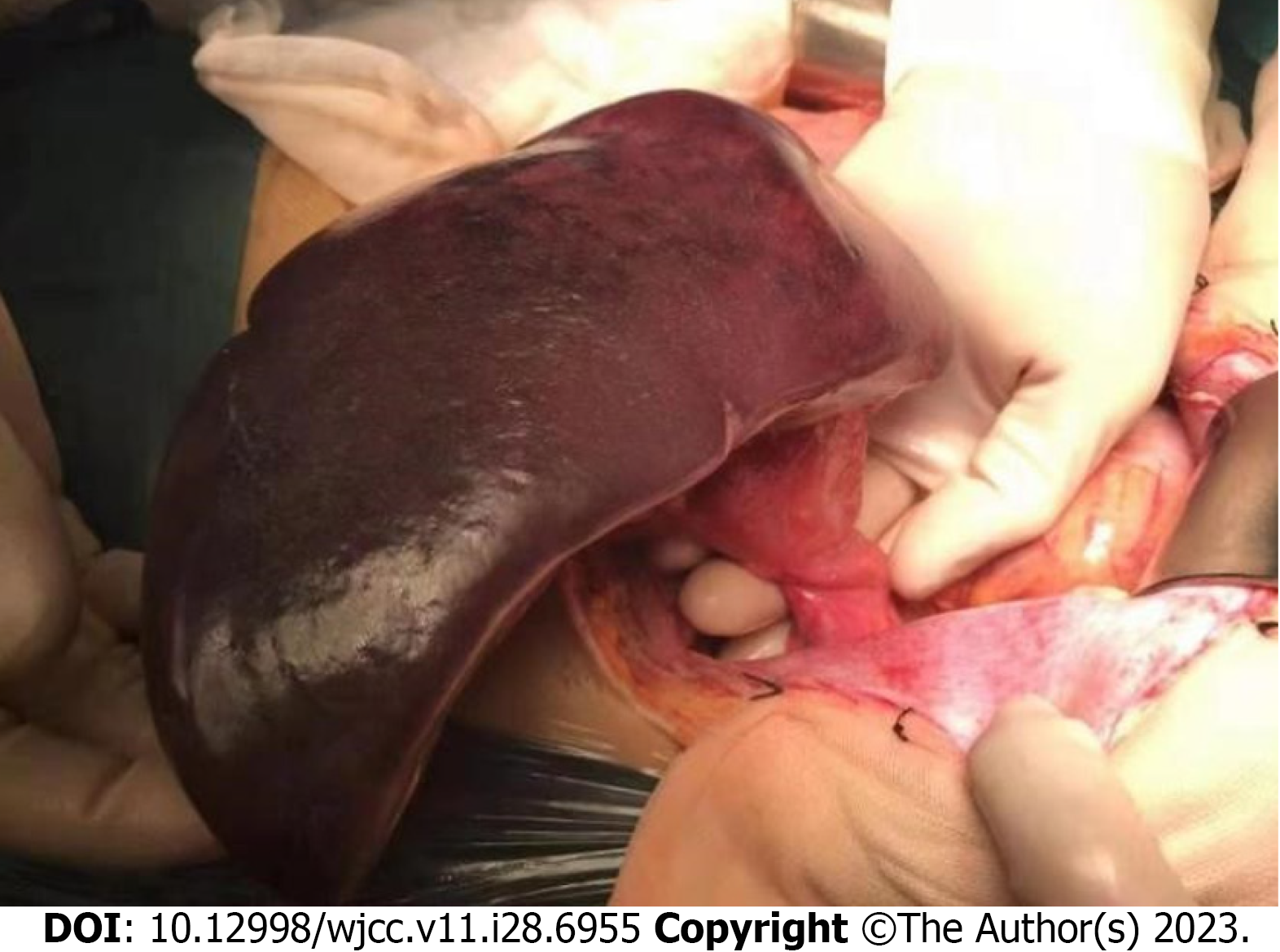
Intraoperative examination revealed a large free spleen with regions of infarction and necrosis in the left lower abdomen. There were no splenogastric ligaments, splenorenal ligaments, diaphragmatic splenic ligaments, or splenocolic ligaments in the spleen. The spleen was purple and had three spiral loops around its pedicle (Figure 3). The main and right branches of the portal vein were filled with thrombosis. This indicated wandering spleen torsion with PVT.
The patient underwent splenectomy and PV thrombectomy. The procedure of portal vein thrombectomy was as follows: The tube wall was cut longitudinally near the main portal vein and the right portal vein branch, with a length of approximately 1 cm. At the same time, in cooperation with the Department of Vascular Intervention, a thrombectomy catheter and balloon were placed through the portal vein incision. The anticoagulation strategy was to continue oral aspirin for 6 mo after discharge with low-molecular-weight heparin during hospitalization. The anti-infective drug ceftazidime was administered.
The patient was hospitalized for 16 d. The PVT disappeared completely after 3 mo. The patient was healthy and asymptomatic at the 4-year follow-up after surgery.
Congenital causes, such as loss or relaxation of ligaments, and acquired causes, such as stomach bloating, splenomegaly, excessive abdominal relaxation, abdominal trauma, and pregnancy, can lead to wandering spleen. All these causes result in the loss or abnormal development of spleen fixation, and the spleen migrates into the abdominal and pelvic cavities[3]. In the present case, there was an acquired cause of postpartum vascular pedicle elongation and abdominal wall relaxation, as well as a congenital cause of missing ligaments.
In a population study based on 23796 consecutive autopsies, Ogren et al[4] found that the overall risk of PVT in the general population is approximately 1%. Severe PVT can easily result in mesenteric ischemia and even intestinal necrosis[5]. PVT can have acute and chronic manifestations and causes of cirrhosis and noncirrhosis. The liver function in the present case was basically normal, with no history of liver cirrhosis. PVT was formed in the short term, indicating that it was caused by acute noncirrhosis. The pathophysiology of PVT is related to the disorder of Virchow’s triad, where venous stasis, endothelial damage, and increased hypercoagulability make the patient prone to thrombosis[6]. Cases involving wandering spleen torsion with thrombosis in the main PV and its branches are rare. However, the cause of PVT is unclear. Yilmaz et al[7] reported a patient with thrombocytosis, accompanied by wandering spleen and spleen torsion, and the formation of PVT, which they believed to be related to thrombocytosis. Our patient had leukocytosis, neutrophilia, and abnormal coagulation, without thrombocytosis. We believe that splenic venous congestion and hypercoagulability in patients after splenic torsion may be the mechanisms underlying PVT. The patient’s hypercoagulable state is associated with neutrophilia. Neutrophil extracellular traps are associated with increased venous thromboembolism risk and/or hypercoagulability[8], which supports our view.
Ultrasonography shows an enlarged spleen with an abnormal location and decreased blood flow on doppler ultrasound[9]. The typical CT imaging manifestations are empty splenic region, unknown mass, ectopic splenic enlargement, and spiral changes of splenic pedicle vessels[10]. Therefore, ultrasound and CT imaging can be used to diagnose and follow up PVT.
If splenic infarction and necrosis have developed, splenectomy is critical. Untwisting and splenic fixation are the recommended treatments only if splenic infarction and necrosis have not developed. In recent years, the use of more conservative and minimally invasive methods, such as laparoscopic surgery, to place a mesh or construct retroperitoneal bags has increased[11]. Thrombolysis, thrombectomy, or transjugular intrahepatic portosystemic shunt are methods of PVT treatment. However, there is no consensus on the intervention strategy. Practical guidelines support anticoagulation as the first-line treatment for PVT. After early anticoagulation treatment, the recanalization rate of thrombi is 38%. The treatment of PVT requires multidisciplinary management for different patients. A detailed introduction of this management and prognosis of wandering spleen torsion with PVT has not been reported in the literature. For patients who undergo splenectomy for complete splenic infarction and develop PVT, anticoagulant therapy is necessary, but the need for surgery remains to be discussed.
Wandering splenic torsion with PVT is a rare nonspecific condition. Splenectomy should be performed in patients with complete splenic infarction. Anticoagulation therapy and individualized management after multidisciplinary consultation according to the patient’s condition are required in the treatment of PVT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jha AK, India; Sato M, Japan S-Editor: Qu XL L-Editor: A P-Editor: Cai YX
| 1. | Göksu M, Baykan AH. Torsion of Wandering Spleen: A Case Report. J Emerg Med. 2020;58:e189-e192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Sharma A, Salerno G. A torted wandering spleen: a case report. J Med Case Rep. 2014;8:133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Ouazzani LCE, Jadib A, Siradji H, Wassi AE, Boutachali R, Tabakh H, Siwane A, Touil N, Kacimi O, Chikhaoui N. Splenic volvulus on ectopic spleen in adults: A case report. Radiol Case Rep. 2022;17:2167-2169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115-2119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 310] [Cited by in RCA: 323] [Article Influence: 17.0] [Reference Citation Analysis (2)] |
| 5. | Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients With and Without Cirrhosis. Gastroenterology. 2019;156:1582-1599.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 244] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 6. | Ju C, Li X, Gadani S, Kapoor B, Partovi S. Portal Vein Thrombosis: Diagnosis and Endovascular Management. Rofo. 2022;194:169-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Yilmaz C, Esen OS, Colak A, Yildirim M, Utebay B, Erkan N. Torsion of a wandering spleen associated with portal vein thrombosis. J Ultrasound Med. 2005;24:379-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Tripodi A, Ammollo CT, Semeraro F, Colucci M, Malchiodi E, Verrua E, Ferrante E, Arnaldi G, Trementino L, Padovan L, Chantarangkul V, Peyvandi F, Mantovani G. Hypercoagulability in patients with Cushing disease detected by thrombin generation assay is associated with increased levels of neutrophil extracellular trap-related factors. Endocrine. 2017;56:298-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Dawson JH, Roberts NG. Management of the wandering spleen. Aust N Z J Surg. 1994;64:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Chauhan NS, Kumar S. Torsion of a Wandering Spleen Presenting as Acute Abdomen. Pol J Radiol. 2016;81:110-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Soleimani M, Mehrabi A, Kashfi A, Fonouni H, Büchler MW, Kraus TW. Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surg Today. 2007;37:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |