Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6943
Peer-review started: July 16, 2023
First decision: July 28, 2023
Revised: August 12, 2023
Accepted: September 11, 2023
Article in press: September 11, 2023
Published online: October 6, 2023
Processing time: 70 Days and 20.5 Hours
Emphysematous cystitis (EC) is a bladder condition commonly caused by gas-generating bacterial infections. Factors that increase the risk for developing this condition include female gender, age ≥ 60 years, and diabetes mellitus, glycosuria, and urinary stasis. The symptoms of EC often lack specificity, making diagnostic imaging techniques crucial for accurate identification of the condition.
This report presents an unusual case of EC that mimicked intestinal perforation. While it was initially challenging to differentiate between intestinal perforation and EC on admission, the patient managed to avoid unnecessary surgery and made a good recovery solely through antibiotic treatment.
Successful treatment of the patient described herein highlights the importance of accurately diagnosing EC, which can be difficult to differentiate from intestinal perforation.
Core Tip: Emphysematous cystitis (EC) is a rare form of complicated urinary tract infection characterized by gas within the bladder wall and lumen. Even with imaging examination(s), such as computed tomography, it can be difficult to differentiate between conditions when there is a significant amount of free air in the abdominal cavity, such as in cases of intestinal perforation and other diseases. Successful treatment of the patient described herein highlights the importance of accurately diagnosing EC, which can be difficult to differentiate from an intestinal perforation.
- Citation: Kang HY, Lee DS, Lee D. Unusual case of emphysematous cystitis mimicking intestinal perforation: A case report. World J Clin Cases 2023; 11(28): 6943-6948
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6943.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6943
Emphysematous urinary tract infections are infectious conditions of the upper or lower urinary tract characterized by the presence of gas within the tissues. They usually involve the renal pelvis or kidney and, in rare cases, the bladder. Diabetes mellitus, urinary tract obstruction, and female sex are the major risk factors for emphysematous cystitis (EC), followed by neurogenic bladder, indwelling catheter, and immunosuppression[1]. In most cases, it can be differentiated using abdo
An 83-year-old woman presented to the emergency department with abdominal pain and diarrhea.
Lower abdominal pain persisted for 1 wk with progressively increasing severity.
The patient’s medical history included hypertension, dementia, hypothyroidism, and osteoporosis. She resided in a nursing home and was a non-smoker and non-drinker.
The patient had worked as a diver, mainly harvesting seafood before retiring 10 years ago.
Physical examination results were as follows: Body temperature, 37.4 °C; blood pressure, 141/88 mmHg; heart rate, 81 beats/min; and respiratory rate, 22 breaths/min. During examination, the patient complained of suprapubic tenderness and displayed diffuse lower abdominal guarding. No signs of abdominal distension or rebound tenderness were obser
Blood test results at the time of admission indicated slight elevations in white blood cell (WBC) count and C-reactive protein (CRP) level. The patient’s WBC count was 11600 cells/mm3 and CRP level was 0.8 mg/L.
The patient was admitted to the internal medicine department and started on antibiotic treatment. On the day of admi
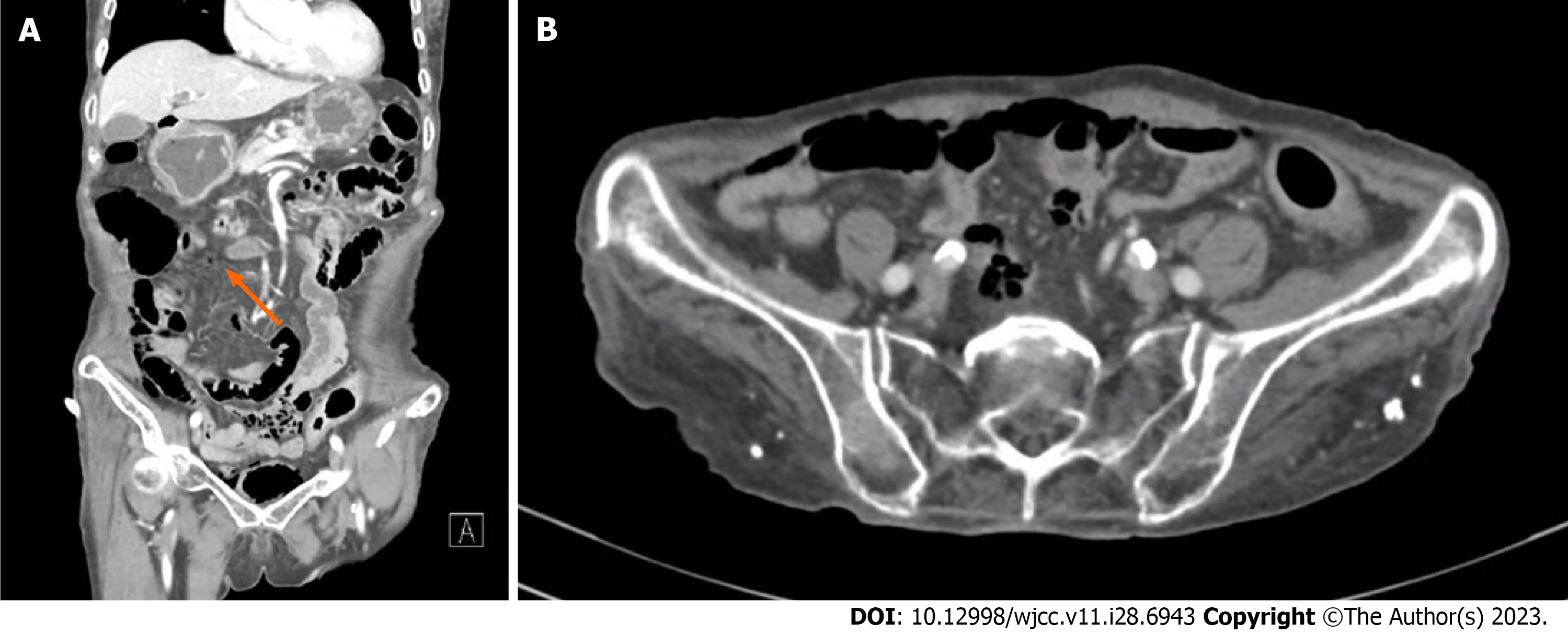
Despite the acute findings on CT, the patient’s vital signs remained relatively stable. However, owing to the scattered presence of free air throughout the abdominal cavity, including visibility under the gallbladder, definitively ruling out intestinal perforations remains challenging. The final diagnosis was intestinal perforation, although EC could not be definitively ruled out. Consequently, due to the potential concern for intestinal perforation and the need for close moni
After urinary catheterization, peripheral blood and urine samples for culture were obtained in the emergency room, and empirical administration of piperacillin/tazobactam (4.5 g) three times daily was initiated. After 7 d of treatment, bacterial cultures yielded positive results for Staphylococcus aureus in both samples. On admission to the intensive care unit, bladder rest was maintained by inserting a Foley catheter with gravity drainage, as per consultation with a urolo
The patient remained afebrile and exhibited stable vital signs, which led to transfer to a general ward on day 4 of hospitalization. On day 12, an abdominopelvic CT scan and a small bowel series were performed to reassess the possi
The patient visited the hospital for a follow-up appointment 2 wk after discharge. There were no notable abnormalities in her laboratory results, nor did she complain of significant discomfort.
EC is a urinary tract infection characterized by the presence of gas in the bladder wall and lumen. It primarily affects females with risk factors in their 60s and 70s, including diabetes, dysuria, recurrent urinary tract infections, and immuno
EC has been characterized in diverse ways, ranging from a severe condition requiring aggressive treatment to prevent unfavorable outcomes, to a benign disease[7]. However, delayed diagnosis can result in infection spreading to the ureters and renal parenchyma, bladder rupture, and even death. Management primarily involves ensuring sufficient urinary drainage, appropriate antibiotic therapy, and improved blood glucose control. Once infection is eradicated, the gas is typi
The diagnosis of EC is primarily made through urine culture to identify the causative organism and imaging examinations such as abdominal CT[8,9]. On abdominal CT, gas formation with a characteristic cobblestone or beaded-necklace appearance is typically observed predominantly on the bladder wall. For cases in which gas is detected not only in the bladder wall but also in the abdominal cavity, distinguishing it from intestinal perforation can be challenging[10]. Additionally, the presence of urogenital gas should be considered in the context of enterobladder fistulas, which can occur due to various underlying conditions such as diverticulosis, Crohn’s disease, rectal sigmoid cancer, or radiation the
Delayed diagnosis of EC can result in the infection spreading to the ureters and renal parenchyma, bladder rupture, and even death[13,14]. Management primarily involves ensuring sufficient urinary drainage, appropriate antibiotic the
In the present case, the patient’s vital signs were stable, and no other abnormalities were noted in blood tests aside from a small increase in CRP and WBC count. However, the presence of free air extending to the upper abdomen adds complexity to the diagnosis and makes it challenging to definitively rule out intestinal perforation. Additional diagnostic measures, such as thorough clinical assessment, imaging studies, and consultation with specialists, are crucial for making accurate diagnoses and guiding appropriate treatment decisions.
EC is described as a critical condition that necessitates intensive treatment to avoid severe, life-threatening complications. However, delayed diagnosis can result in spread of the infection to the ureters and renal parenchyma, and even lead to bladder rupture or death. This case report highlights that EC can manifest in uncommon ways, suggesting that treat
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Duan SL, China; Wen XL, China S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Swede SA, Ojo AO, Momah T. Emphysematous Cystitis in an Uncontrolled Diabetic: A Case Report. Cureus. 2021;13:e20328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Yeh CM, Huang SY, Chou CM. Emphysematous cystitis presenting as pneumoperitoneum and pneumoretroperitoneum. Asian J Surg. 2023;46:2622-2623. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Toyota N, Ogawa D, Ishii K, Hirata K, Wada J, Shikata K, Makino H. Emphysematous cystitis in a patient with type 2 diabetes mellitus. Acta Med Okayama. 2011;65:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Yashima H, Terasaki M, Kushima H, Hirano T. Emphysematous cystitis in an elderly Japanese patient with type 2 diabetes mellitus. Clin Case Rep. 2019;7:585-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Bobba RK, Arsura EL, Sarna PS, Sawh AK. Emphysematous cystitis: an unusual disease of the Genito-Urinary system suspected on imaging. Ann Clin Microbiol Antimicrob. 2004;3:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | BAILEY H. Cystitis emphysematosa; 19 cases with intraluminal and interstitial collections of gas. Am J Roentgenol Radium Ther Nucl Med. 1961;86:850-862. [PubMed] |
| 7. | Sánchez-Oro R, Ibáñez-Muñoz D, Yanguas-Barea N. Emphysematous cystitis as a rare form of urinary tract infection. Arch Esp Urol. 2019;72:980-981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Eken A, Alma E. Emphysematous cystitis: The role of CT imaging and appropriate treatment. Can Urol Assoc J. 2013;7:E754-E756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Wojack PR, Goldman IA. Emphysematous cystitis with extraperitoneal gas: new insights into pathogenesis via novel CT findings. Clin Imaging. 2020;65:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Fumeo M, Manfredi S, Volta A. Emphysematous cystitis: review of current literature, diagnosis and management challenges. Vet Med (Auckl). 2019;10:77-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Yin J, Marino A, Cooke P, Bitar K. Post-radiotherapy vesicocutaneous fistula presenting as gas/fluid-filled groin swelling. J Surg Case Rep. 2011;2011:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Amano M, Shimizu T. Emphysematous cystitis: a review of the literature. Intern Med. 2014;53:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Becker B, George A, Owen R. A nontraditional presentation and treatment for emphysematous cystitis. Urol Case Rep. 2023;46:102321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Rajaian S, Murugavaithianathan P, Krishnamurthy K, Murugasen L. Emphysematous cystitis: diagnosed only if suspected. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Sasaki Y, Shiozaki K, Nakanishi R, Izaki H, Kanda K. [Successful treatment of severe emphysematous cystitis using retropenitoneal drainage: A case report]. Nihon Hinyokika Gakkai Zasshi. 2019;110:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | McCabe JB, Mc-Ginn Merritt W, Olsson D, Wright V, Camporesi EM. Emphysematous cystitis: rapid resolution of symptoms with hyperbaric treatment: a case report. Undersea Hyperb Med. 2004;31:281-284. [PubMed] |