Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6877
Peer-review started: June 18, 2023
First decision: August 10, 2023
Revised: August 15, 2023
Accepted: September 11, 2023
Article in press: September 11, 2023
Published online: October 6, 2023
Processing time: 99 Days and 3 Hours
Rotationplasty is often performed for malignant tumors, but type BIIIb rotationplasty is rarely reported, and there needs to be more evidence of the procedure and treatment. The purpose of this case study was to report a new direction in the use of type BIIIb rotationplasty in treating patients with limb salvage and long-term non-healing infections.
Case 1: A 47-year-old man underwent radiotherapy for hemangioendothelioma in his left thigh, resulting in a femoral fracture. Despite the use of plates, intramedullary nailing, and external fixators, the femoral bone failed to unite due to infectious nonunion. Multiple operations were unable to control the infection, leaving the patient immobile. We performed a modified tibia-pelvic-constrained hip rotationplasty, utilizing a constrained prosthetic hip between the tibia and pelvis following a femur resection. Two years post-surgery, the patient was able to walk with the prosthetic device without any signs of recurring infection. The corresponding functional scores were 72 points for the Musculoskeletal Tumor Society (MSTS), 53 for the Functional Mobility Assessment (FMA), 93 for the Toronto Extremity Salvage Score (TESS), and 56 for the MOS 36-item short form health survey (SF-36). Case 2: A 59-year-old woman presented with liposarcoma in her left thigh. Magnetic resonance imaging revealed tumors in the medial, anterior, and posterior femur muscles, encircling the femoral vessels and nerves. Fortunately, there were no symptoms of sciatic dysfunction, and the tumor had not invaded the sciatic nucleus. After one year of follow-up, the patient expressed satisfaction with limb preservation post-type BIIIb rotationplasty. The corresponding functional scores were 63 points for the MSTS, 47 for the FMA, 88 for the TESS, and 52 for the SF-36.
Our study suggests that type BIIIb rotationplasty may be an alternative to amputation in patients with incurable infections. For malignant tumors of the lower extremities without invasion of the sciatic nerve, type BIIIb rotationplasty remains an excellent alternative to amputation. This surgical method may prevent amputation, improve functional outcomes, and facilitate biological reconstruction.
Core Tip: Rotationplasty has been reported primarily as an alternative to amputation for malignant tumors, while reports on type BIIIb rotationplasty have been rarer. Our study suggests that type BIIIb rotationplasty may be an alternative to amputation or extended tumor prostheses in two cases of patients suffering from incurable infections. This surgical method may prevent amputation, improve functional outcomes, and facilitate biological reconstruction.
- Citation: Chen ZX, Guo XW, Hong HS, Zhang C, Xie W, Sha M, Ding ZQ. Rotationplasty type BIIIb as an effective alternative to limb salvage procedure in adults: Two case reports. World J Clin Cases 2023; 11(28): 6877-6888
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6877.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6877
When a tumour has significantly affected the femoral extremity, rotationplasty, also known as the Van Nes procedure, is used to restore function of the lower extremity after complete separation of the femur[1]. However, psychological distress is highly prevalent in rotationplasty patients. The unusual limb appearance caused by the procedure and its complexity often make rotationplasty a less preferred choice for patients, and the intricate surgical process complicates the success rate for physicians[2]. From a biomechanical perspective, Van Nes rotationplasty has recently become the most valid procedure for active control of the “pseudo-knee”, allowing for a smooth and coordinated gait pattern[3].
In recent years, significant advances have been made in joint preservation. Moses et al[4] reported that pediatric Chinese patients with lower extremity bone sarcoma and slight body build showed good and excellent mid-term results in implant survival and limb function. Concurrently, Kumta et al[5] demonstrated that useful limb salvage could be achieved by applying microsurgical techniques for various indications in limb salvage surgery after tumour excision. Modern innovations in limb repair and reconstruction techniques, such as prostheses with antimicrobial coatings[6,7], 3D-printed multifunctional bone scaffolds[8], and osseointegration techniques[9], have opened new avenues for limb preservation.
Rotationplasty not only provides better functional efficacy but also offers biological reconstruction compared to lower limb amputations[10]. It has distinct advantages for femur cancer patients over those using prostheses, such as the absence of phantom pain, preservation of articular and cutaneous proprioception, and more frequent participation in hobbies and sports[11]. Rotationplasty also offers tremendous benefits for children, who are highly adaptable and still growing. For adults, rotationplasty can improve the patient's quality of life post-procedure and enable self-care in the future. Long-term follow-up data reveal that young patients undergoing Van Nes rotationplasty have higher levels of function and quality of life[12]. Additionally, rotationplasty requires a much lower energy cost of ambulation compared to above-knee amputees[13]. Interestingly, it has been noted that patients who opt for rotationplasty at lower costs are often from low socioeconomic backgrounds and cannot afford a prosthesis, particularly in developing countries[14]. Winkelmann proposed the classification of rotationplasty variants in 1986[15]. For the proximal and middle part of the involved femur, rotationplasty type B is typically the treatment of choice, as opposed to above-knee amputations or prostheses[16]. Rotationplasty type BIII, necessitated by the tumor's location, requires the removal of the entire femur, either affixing the tibia to the pelvis (BIIIa) or replacing a hip prosthesis and attaching the tibia to the pelvis (BIIIb)[17]. The prosthetist's experience with this unusual form of fitment often becomes critical in a patient's acceptance or rejection of this limb salvage method. Currently, type BIIIb rotationplasty is used to treat femur congenital anomalies and malignancies. However, detailed knowledge about this procedure's operation and long-term functional outcomes remains limited. We present two cases in which we utilized this rare procedure to treat patients with femur malignancies of the thigh, achieving functional outcomes without evidence of recurrence over a 24-mo follow-up period. We found that type BIIIb rotationplasty is not suitable for patients without both the hip capsule and the bony stop of the greater trochanter. Both absolute and relative contraindications have been proposed for type BIIIb rotationplasty[18]. Absolute contraindications for rotationplasty include sciatic nerve injury and tumors surrounding the sciatic nerve. A tension-free anastomosis of the vessel after segmental resection is recommended for cases of tumor invasion. Even if the vessel is not invaded, kinking or leaving long and coiled vessels in the limb increases the risk of thrombosis, which may lead to vascular damage and subsequent failure of rotationplasty[2,13,19,20].
The two patients were informed that their case data would be submitted for publication and provided consent.
Case 1: A 47-year-old male patient presented with persistent pain in his left thigh and mobility impairment for over a year.
Case 2: A 61-year-old female patient presented with swelling and pain in her left thigh that had persisted for over 3 mo.
Case 1: The patient had undergone surgical resection and radiotherapy for left femoral hemangioendothelioma at various medical institutions more than 30 times.
Case 2: The patient’s left thigh has been swollen and painful for over 3 mo.
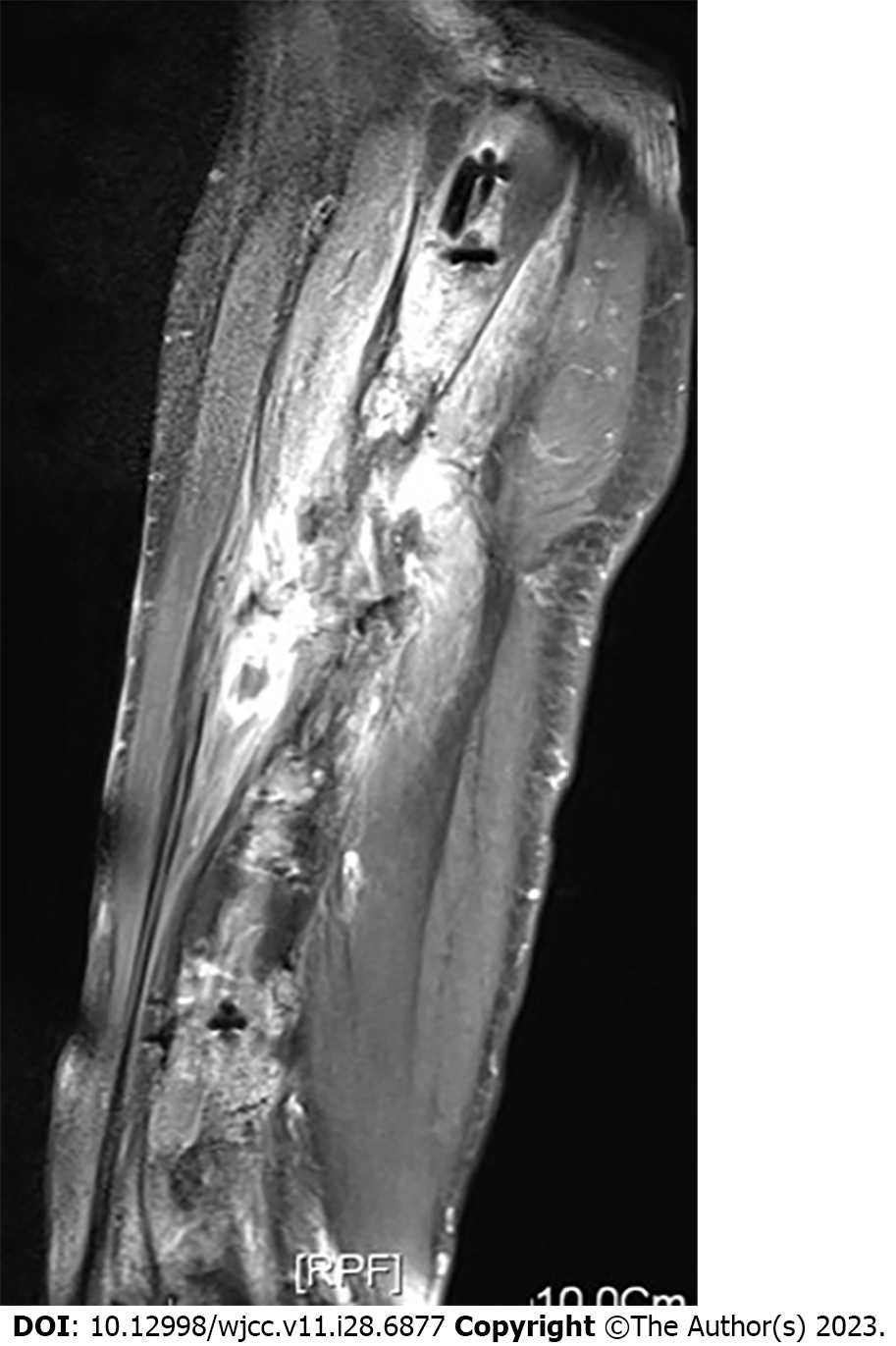
Case 1: In May 2014, the patient fractured his femur due to the effects of chemotherapy and underwent plate internal fixation treatment. Regrettably, the patient later experienced pain from a plate fracture. Subsequently, in November 2014, a femoral bone marrow internal nail treatment was performed. However, due to a wound infection in January 2016, the patient could not be treated with an external fixator for the fractured end. Despite this, the patient's wound continued to discharge pus over the following year (Figure 1). On June 5, 2017, the patient was admitted to our hospital for standardized treatment.
Case 2: The patient had no previous abnormalities.
Case 1: The patient denied any family history of malignant tumors.
Case 2: The patient denied any family history of malignant tumors.
Case 1: The patient's limb refused to move because of the pain of fracture.
Case 2: The patient had limited walking movement of the limb, and the circumference of the affected limb was swollen by 5 cm compared with the opposite side.
Case 1: Laboratory examinations confirmed the diagnosis of left femoral hemangioendothelioma.
Case 2: Laboratory examinations confirmed the diagnosis of left liposarcoma.
Case 1: Radiographs revealed poor healing due to infection following chemotherapy (Figure 2). Magnetic resonance imaging (MRI) indicated that the patient's greater trochanter of the femur was not infected, leading us to decide to preserve it during preoperative planning (Figure 3).
Case 2: Upon admission to our hospital for standardized treatment and evaluation, an ultrasound-guided soft tissue biopsy was performed. The biopsy resulted in a diagnosis of liposarcoma. Preoperative MRI showed that the tumor encircled the blood vessels in the posterior region of the thigh's muscles (Figure 4). Fortunately, the tumor had not invaded the sciatic nerve (Figure 5).
After consulting with multiple hospitals, amputation was recommended. The patient, however, found the prospect of amputation difficult to accept.
After consulting several hospitals and orthopedic surgeons, amputation was suggested, but the family and the patient said that it was difficult to accept.
Combined with the patient’s medical history, the final diagnosis was hemendothelioma of the left thigh with pathological fracture nonunion after surgery.
Combined with the patient’s medical history, the final diagnosis was liposarcoma of the left thigh.
Case 1: A routine preoperative examination was performed. After discussing the risks and benefits of available surgical options, the patient opted for right femur excision with by type BIIIb rotationplasty, which facilitates the maximum removal of non-viable infected tissue. During a preoperative consultation, a bone oncologist explained to the patient the potential postoperative appearance, function, as well as the advantages and disadvantages of the procedure. The patient preferred the aesthetic and functional outcomes of rotationplasty over amputation. This surgical procedure aimed to avoid hip joint dislocation, a goal largely dependent on the successful reconstruction of the ligaments and muscles surrounding the hip joint.
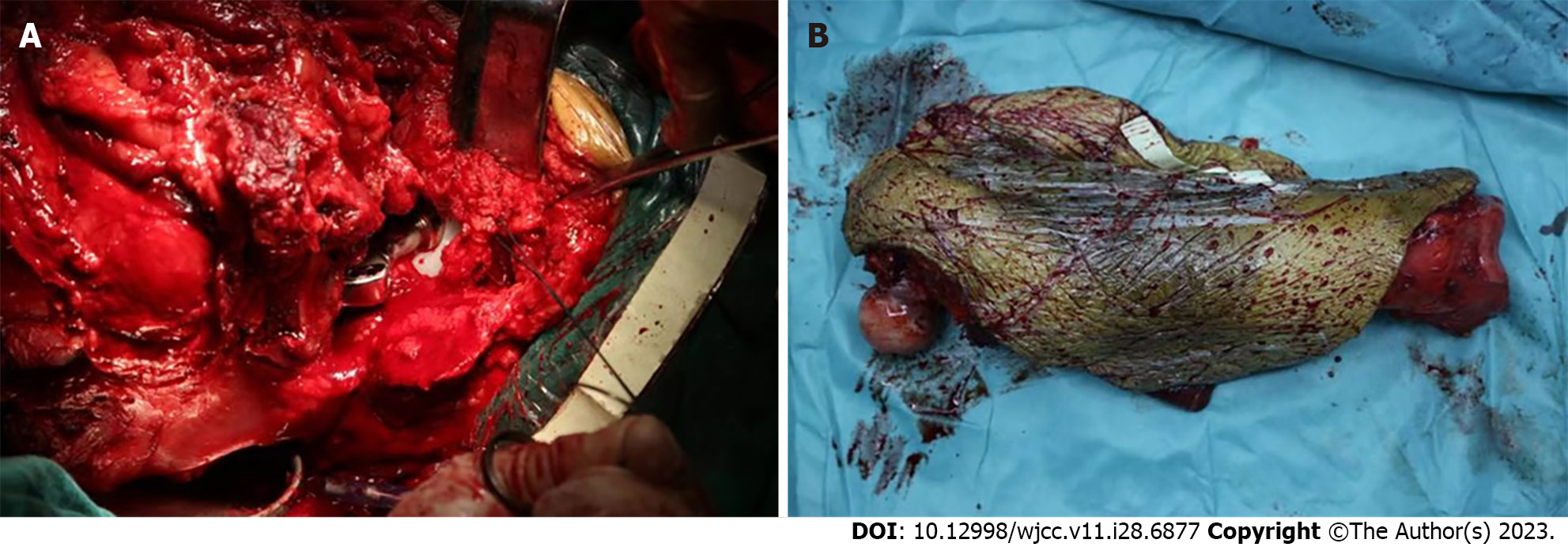
Case 2: After ruling out relevant contraindications to surgery and explaining the risks, postoperative appearance, function, and the pros and cons of performing rotationplasty, the patient gave her consent to undergo a left thigh femoral tumor resection with a type BIIIb rotationplasty procedure.
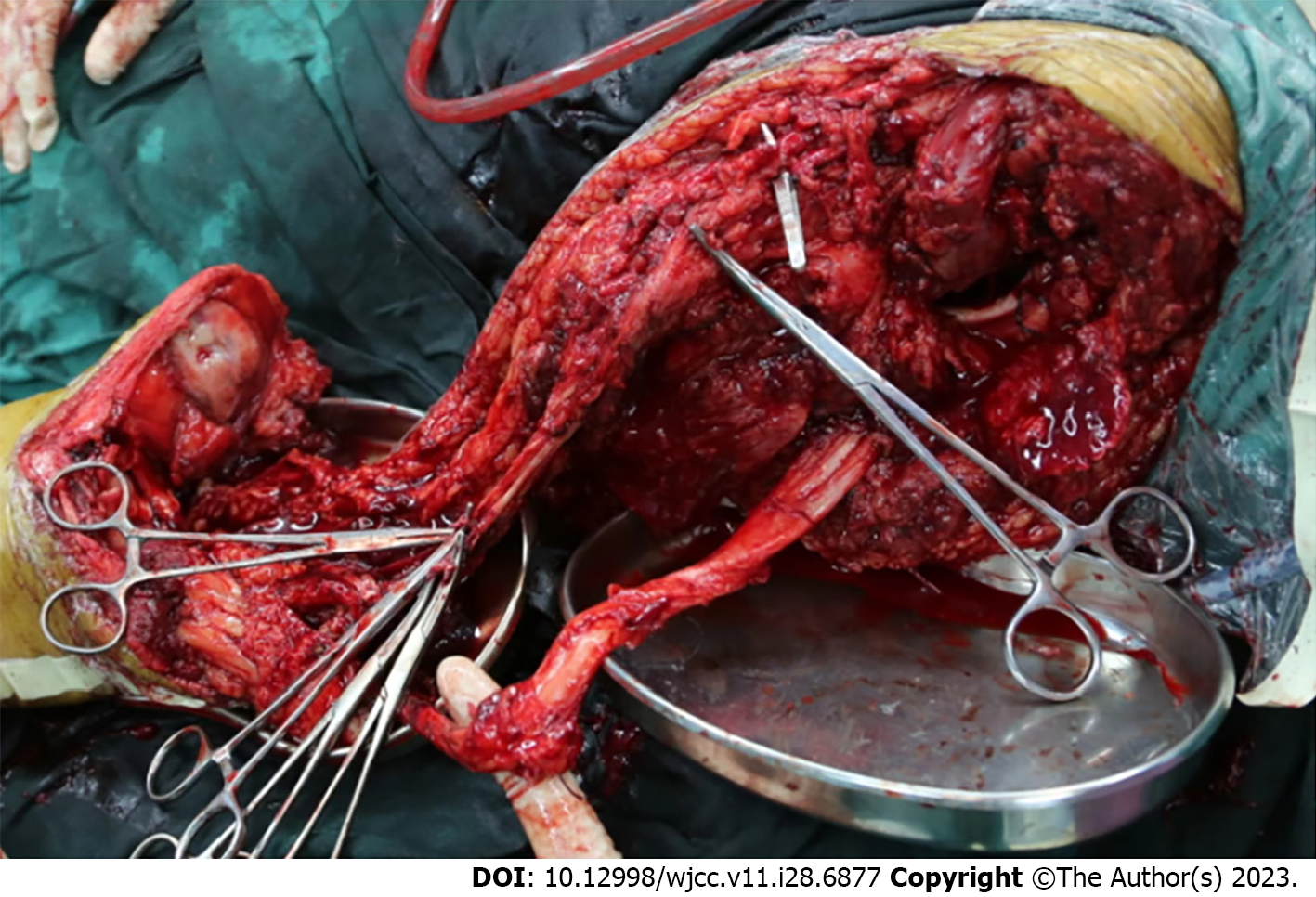
Case 1: Figure 6 illustrates the incision chosen for the surgical removal of the infected femur, which allowed for tension-free suturing after the implantation of the rotationplasty prosthesis. The surgeon preserved the relatively healthy skin and semitendinosus and semimembranosus muscles on the medial side of the patient's leg, while the sciatic nerve was carefully isolated according to its anatomical pathway. The procedure resulted in a stenotic tissue flap, composed of skin, muscle, the sciatic nerve, and femoral vessels (Figure 7).
We then used a swing saw to create a rough surface on the medial side of the tibial plateau to facilitate the attachment of the greater trochanter. Intraoperatively, bone cement was used to securely affix the bipolar head prosthesis to the tibia. This prosthesis was produced by WeiGao Medical Material Co. Ltd (Beijing, China), and the bone cement was supplied by Double Engine Medical Material Co. Ltd (Xiamen, China). We carefully wrapped the vessels around the prosthesis, and used the remaining joint capsule to enclose the bipolar head in a purse-string suturing fashion to prevent hip dislocation. To improve prosthesis stability, the tissue flap was sutured around the prosthesis. At this stage, the blood vessels showed no signs of bending or local compression (Figure 8).
Finally, we sutured the remaining adductor tendon to the biceps femoris tendon of the fibular head. The gluteus maximus and patellar tendons were closed with 0 polypropylene sutures, and the iliopsoas tendon and gastrocnemius were stitched together to stabilize the hip joint. After surgery, we closely monitored the patient's blood flow, swelling, and nerve function.
Case 2: During the procedure, because the tumor had encased the femoral artery, the femoral arterial vessel had to be carefully anastomosed after being removed along with the tumor (Figure 9). As the greater trochanter of the femur had not been preserved in this patient, we anastomosed the tendon of the abductor muscle with the tendon in the pes anserine area. Other intraoperative and postoperative treatments were similar to those in Case 1. The bipolar head prosthesis used was manufactured by WeiGao Medical Material Co. Ltd (Beijing, China), and the bone cement was sourced from Double Engine Medical Material Co. Ltd (Xiamen, China).
On the first day post-surgery, we encouraged the patient to perform ankle flexion and extension exercises. These exercises not only improve venous circulation and prevent ankle stiffness but also stimulate the brain to control different muscle groups. Sutures were removed 2 wk after surgery, with no signs of superficial infection or deep effusion in the affected limb. For 3 wk, we used braces to prevent dislocation.
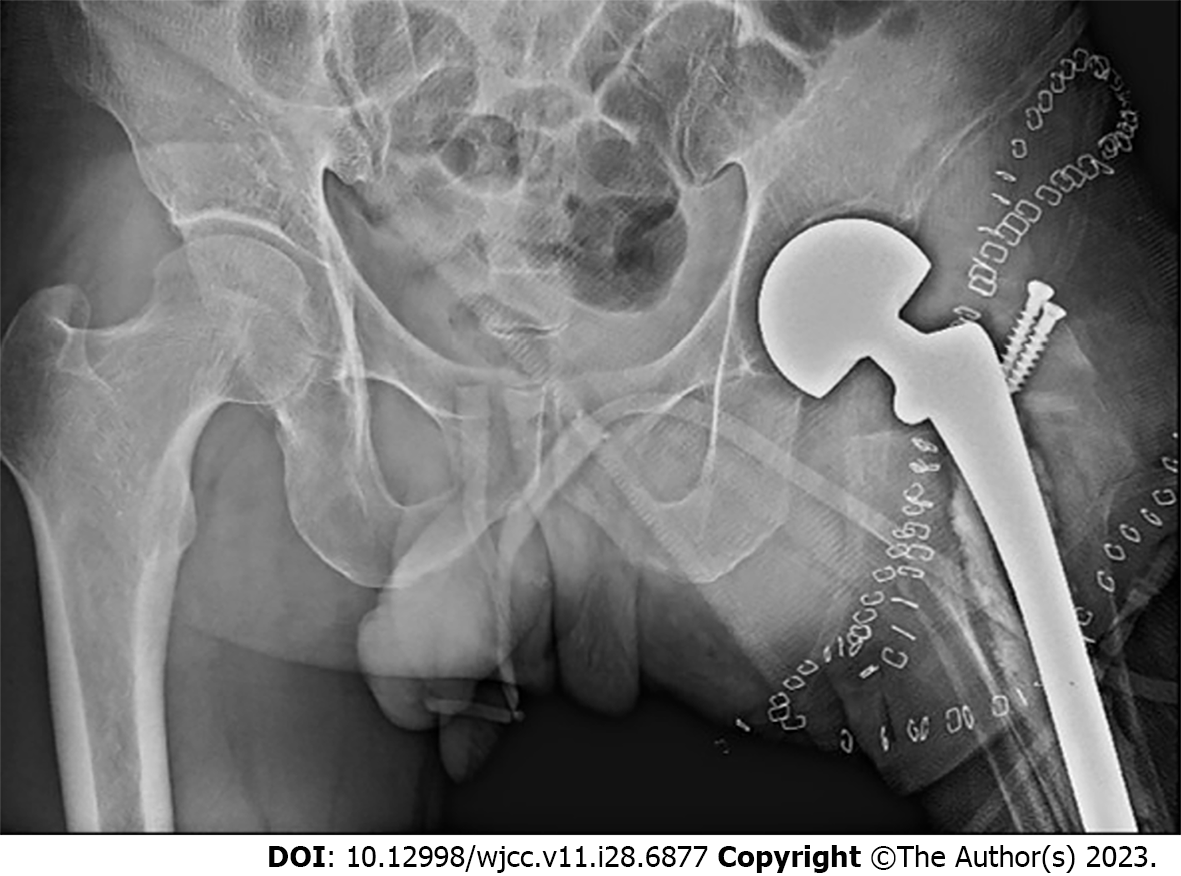
Three weeks post-surgery, under the guidance of a rehabilitation physician, the patient began active and passive exercises for hip joint function. Three months after surgery, prosthetics were fitted and the patient began walking training with additional support. Radiographs of the hip joint revealed that the prosthesis was well-positioned and that the greater trochanter was secured with screws in the orthostatic hip joint (Figure 10). There were no visible deformities and the legs appeared equal in length when examining the prosthetics. A full-length X-ray of both lower extremities showed the ankle joint at the level of the contralateral knee (Figure 11).
The patient could walk comfortably without a walker's aid (Video 1). Two years post-operation, the patient's functional status was satisfactory. The corresponding functional scores were as follows: 72 points for the Musculoskeletal Tumor Society (MSTS), 53 for the Functional Mobility Assessment (FMA), 93 for the Toronto Extremity Salvage Score (TESS), and 56 for the MOS 36-item short form health survey (SF-36)[21].
Postoperatively, the patient developed a skin necrosis of about 2 cm x 1 cm in the skin fold of the inner thigh, which healed following disinfection. An X-ray review after surgery showed that the ankle joint was aligned closely to the healthy knee joint (Figure 12).
After two years of follow-up, the patient was able to walk normally and exhibited good functional activities (Video 2). The patient expressed satisfaction with her current appearance and functionality. Her corresponding functional scores were as follows: 63 points on the MSTS scale, 47 on the FMA, 88 on the TESS, and 52 on the SF-36.
Rotationplasty is primarily employed for conditions such as congenital absence of the femur, malignant tumors of the proximal femur and tibia[22], failed limb salvage operations[16,23,24], and tumor prosthesis infection[25]. Kajetan et al[26] also applied it to severe lower limb trauma. Compared to patients with above-knee amputations, those undergoing rotationplasty have demonstrated improved sensation during walking and standing[14], preservation of knee-level joint function, more efficient gait patterns, and reduced oxygen consumption[27]. However, one of the major challenges remains patient acceptance of the postoperative appearance of the limb.
Absolute contraindications for rotationplasty include sciatic nerve injury, ankle stiffness, and denervation of the calf muscles. Relative contraindications encompass factors such as psychological non-acceptance by the patient, advanced age, bilateral congenital absence of the femur, arterial obliterans, and venous thrombosis[18].
To date, few studies have been reported on type BIIIb rotationplasty[28]. The success of type BIIIb rotationplasty largely depends on lesion resection, vascular reconstruction, and soft tissue coverage, all critical factors for hip stability reconstruction. Our case study focused on the reconstruction of hip stability and surgical techniques in type BIIIb rotationplasty. Due to the complete destruction of the hip joint in these cases, stability was entirely lost. Preserving hip stability in patients undergoing this type of treatment poses a significant challenge. The excellent function exhibited by our two patients can be primarily attributed to our prior surgical experience with proximal femur tumors.
In terms of achieving stable outcomes with neoplastic hip prostheses, the hip capsule plays a crucial role. We were able to retain the hip capsule in both cases, demonstrating good static stability both intraoperatively and postoperatively. Secondly, the reconstruction of the abductor muscles is of utmost importance. In the first case, we retained part of the greater trochanter and fixed it to the host's medial tibial plateau. This ensured a good hip abductor tone, and the patient showed improved hip function at long-term follow-up. In the second case, due to tumor involvement, the bone tissue at the greater trochanter could not be retained. Thus, the abductor's tendon was anastomosed with the tendon of the pes anserine area. This resulted in slightly reduced hip joint abductor function compared to the first patient. The third stabilizing mechanism involves the reconstruction of the surrounding muscles. Given the extensive soft tissue excision, the muscles present are primarily in the abdominal part, making it challenging to ensure greater tension.
It is important to note that the plane of the ankle joint and the contralateral knee joint should be maintained. The error should be controlled within 3 cm as much as possible to ensure that patients appear normal when walking and sitting. In this study, we provided the patients with the longest possible prostheses. However, in the second patient, one knee joint was still 4 cm higher than the other due to a shorter tibia.
During intraoperative reconstruction, attention should also be paid to the rotation of the affected limb. Rotation deformity may cause noticeable abnormal gait and may even necessitate surgical correction[22]. Prosthesis insertion requires the movement of the ankle joint to determine the forward angle of the prosthesis installation, which is particularly important for patients requiring hip reconstruction.
Late soft tissue reconstruction is employed to maintain a stable inclination angle. In the first case, the anterior inclination was fixed by rebuilding the orthostatic stop of the abductor's muscle. In contrast, in the second case, stability was maintained simply by anastomosing the abductor tendon and the tendon of the pes anserine area. However, the tendon of the pes anserine area was skewed backwards and then reversed 180 degrees to the front, resulting in a significant anterior inclination after the suture. Therefore, the anterior part of the abductor's muscle was anastomosed with the tendon of the pes anserine area.
There are two primary methods for the treatment of blood vessels during these procedures: Anastomosis and local entanglement of preserved blood vessels. The latter may lead to the formation of thrombi, while vascular anastomosis is considered a risk factor for vascular damage, potentially resulting in vascular anastomosis failure. Notably, these two surgical methods have no significant difference in causing vascular complications. Therefore, the decision to either resect the vessel or perform surgical anastomosis depends on whether the tumor has invaded the vessel.
It is important to note that repairing infected prostheses by rotationplasty carries a higher risk of vascular distortion than treating primary sarcomas by rotationplasty. This is due to scar formation causing large blood vessels to lose their elasticity, making them more prone to kinks. In our two cases, there were no vascular complications following these two treatments. Hence, type BIIIb rotationplasty is not recommended for patients who cannot preserve both the hip capsule and the bony stop of the greater trochanter.
Even though type BIIIb rotationplasty destroys the hip joint, excellent hip stability and joint function can be achieved with a precise preoperative design and optimal intraoperative soft tissue reconstruction. However, it is crucial to be mindful of potential late complications, such as aseptic prosthesis loosening, implant failure, or deep infection. To prevent deep infections, in addition to the application of antibiotics, we anticipate that further prevention could be achieved by applying an antibacterial silver coating on the prosthesis[29]. It is important to note that in terms of applying an antibacterial silver coating, this is typically not applied to femoral hip stems but rather to the bodies of mega-prostheses where there is ample surface of the implant coating exposed to the tissues.
Rotationplasty is a multidisciplinary procedure requiring the collaboration of orthopedic surgeons, specialist nurses, prosthetic fabricators, rehabilitation physicians, and psychological counselors during the perioperative period. Preoperatively, the surgeon and specialist need to discuss the advantages, disadvantages, and potential complications of the procedure with the patient and his/her family members, demonstrate the appearance and function of previous similar patients, and most importantly, ensure that the patient understands and accepts the expected physical appearance post-procedure. Postoperatively, the rehabilitation physician and prosthetist must provide detailed instructions on the rehabilitation program. The cooperation of this multidisciplinary team is key to ensuring the successful completion of the surgery and good postoperative function for the patient.
Our study indicates that type BIIIb rotationplasty may serve as an alternative to amputation for patients with incurable infections or when the extension of tumor prostheses is not feasible. The advantages of this surgical approach include enhanced functional outcomes and the benefits of biological reconstruction.
We want to express our gratitude to all physicians and nurses involved in the management of the patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: the Professional Group of Bone Tumors of the Whole Army; the Spine Osteopathy Group, Digital Orthopaedics Group, Chinese Medical Association; the Pelvic Oncology Group, Sarcoma Committee of Chinese Anticancer Association; the Fujian Province bone tumor professional group of Chinese medical doctors Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Muthu S, India S-Editor: Lin C L-Editor: Wang TQ P-Editor: Yu HG
| 1. | Cammisa FP Jr, Glasser DB, Otis JC, Kroll MA, Lane JM, Healey JH. The Van Nes tibial rotationplasty. A functionally viable reconstructive procedure in children who have a tumor of the distal end of the femur. J Bone Joint Surg Am. 1990;72:1541-1547. [PubMed] |
| 2. | Sawamura C, Hornicek FJ, Gebhardt MC. Complications and risk factors for failure of rotationplasty: review of 25 patients. Clin Orthop Relat Res. 2008;466:1302-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Catani F, Capanna R, Benedetti MG, Battistini A, Leardini A, Cinque G, Giannini S. Gait analysis in patients after Van Nes rotationplasty. Clin Orthop Relat Res. 1993;270-277. [PubMed] |
| 4. | Moses Li ML, Wong KC, Chiu WK, Kumta SM. Intermediate-term results and risk factors analysis of tumor endoprosthesis in paediatric patients after the resection of lower extremity bone sarcoma. J Orthop Surg (Hong Kong). 2022;30:10225536221132403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Kumta SM, Yip KM, Lee YL, Lin J, Leung PC. Limb salvage surgery with microsurgical reconstruction for the treatment of musculoskeletal tumours involving the upper extremity. Ann Acad Med Singap. 1995;24:8-14. [PubMed] |
| 6. | Tomczak C, Beaman D, Perkins S. Combined Intramedullary Nail Coated With Antibiotic-Containing Cement and Ring Fixation for Limb Salvage in the Severely Deformed, Infected, Neuroarthropathic Ankle. Foot Ankle Int. 2019;40:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Coathup MJ, Cobb JP, Walker PS, Blunn GW. Plate fixation of prostheses after segmental resection for bone tumours. J Orthop Res. 2000;18:865-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Zhu C, He M, Sun D, Huang Y, Huang L, Du M, Wang J, Li Z, Hu B, Song Y, Li Y, Feng G, Liu L, Zhang L. 3D-Printed Multifunctional Polyetheretherketone Bone Scaffold for Multimodal Treatment of Osteosarcoma and Osteomyelitis. ACS Appl Mater Interfaces. 2021;13:47327-47340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 9. | Tanaka KS, Andaya VR, Thorpe SW, Gundle KR, Hayden JB, Duong YC, Avedian RS, Mohler DG, Morse LJ, Zimel MN, O'Donnell RJ, Fang A, Randall RL, Tran TH, New C, Wustrack RL; other members of Study Group FORCE. Survival and failure modes of the Compress® spindle and expandable distal femur endoprosthesis among pediatric patients: A multi-institutional study. J Surg Oncol. 2023;127:148-158. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Winkelmann WW. Type-B-IIIa hip rotationplasty: an alternative operation for the treatment of malignant tumors of the femur in early childhood. J Bone Joint Surg Am. 2000;82:814-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Canavese F, Samba A, Khan A, Dechelotte P, Krajbich JI. Rotationplasty as a salvage of failed primary limb reconstruction: up to date review and case report. J Pediatr Orthop B. 2014;23:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Ackman J, Altiok H, Flanagan A, Peer M, Graf A, Krzak J, Hassani S, Eastwood D, Harris GF. Long-term follow-up of Van Nes rotationplasty in patients with congenital proximal focal femoral deficiency. Bone Joint J. 2013;95-B:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Mahoney CR, Hartman CW, Simon PJ, Baxter BT, Neff JR. Vascular management in rotationplasty. Clin Orthop Relat Res. 2008;466:1210-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Agarwal M, Puri A, Anchan C, Shah M, Jambhekar N. Rotationplasty for bone tumors: is there still a role? Clin Orthop Relat Res. 2007;459:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Winkelmann WW. Hip rotationplasty for malignant tumors of the proximal part of the femur. J Bone Joint Surg Am. 1986;68:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Hillmann A, Gosheger G, Hoffmann C, Ozaki T, Winkelmann W. Rotationplasty--surgical treatment modality after failed limb salvage procedure. Arch Orthop Trauma Surg. 2000;120:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Winkelmann WW. Rotationplasty. Orthop Clin North Am. 1996;27:503-523. [PubMed] [DOI] [Full Text] |
| 18. | Gupta SK, Alassaf N, Harrop AR, Kiefer GN. Principles of rotationplasty. J Am Acad Orthop Surg. 2012;20:657-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Gosheger G, Hillmann A, Ozaki T, Bertsch C, Winkelmann W. Revision hip arthroplasty in a patient with a hip rotationplasty (type B III b). Arch Orthop Trauma Surg. 2002;122:186-187. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Bonardelli S, Nodari F, Maffeis R, Ippolito V, Saccalani M, Lussardi L, Giulini S. Limb salvage in lower-extremity sarcomas and technical details about vascular reconstruction. J Orthop Sci. 2000;5:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Ginsberg JP, Rai SN, Carlson CA, Meadows AT, Hinds PS, Spearing EM, Zhang L, Callaway L, Neel MD, Rao BN, Marchese VG. A comparative analysis of functional outcomes in adolescents and young adults with lower-extremity bone sarcoma. Pediatr Blood Cancer. 2007;49:964-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Sawamura C, Matsumoto S, Shimoji T, Ae K, Tanizawa T, Gokita T, Koyanagi H, Okawa A. Indications for and surgical complications of rotationplasty. J Orthop Sci. 2012;17:775-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Gaillard J, Fouasson-Chailloux A, Eveno D, Bokobza G, Da Costa M, Heidar R, Pouedras M, Nich C, Gouin F, Crenn V. Rotationplasty Salvage Procedure as an Effective Alternative to Femoral Amputation in an Adult With a History of Osteosarcoma: A Case Report and Review. Front Surg. 2021;8:820019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Gottsauner-Wolf F, Kotz R, Knahr K, Kristen H, Ritschl P, Salzer M. Rotationplasty for limb salvage in the treatment of malignant tumors at the knee. A follow-up study of seventy patients. J Bone Joint Surg Am. 1991;73:1365-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 66] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Okazaki N, Kumagai K, Egashira M, Osaki M, Murata M, Tomita M, Shindo H. Hip rotationplasty with antibiotic-loaded bone cement spacer for severe infection following limb-sparing surgery. Orthopedics. 2008;31:713. [PubMed] [DOI] [Full Text] |
| 26. | Klos K, Mückley T, Gras F, Hofmann GO, Schmidt R. Early posttraumatic rotationplasty after severe degloving and soft tissue avulsion injury: a case report. J Orthop Trauma. 2010;24:e1-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Nebelung W, Birger T, Röpke M, Neumann HW. Rotationplasty as a salvage procedure in revision of tumor endoprosthesis of the distal femur--a report of two cases. Arch Orthop Trauma Surg. 2000;120:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Cahill SV, Yu KE, Dussik CM, Lee FY. Rotational Tibio-Pelvic Constrained Hip Arthroplasty: A Surgical Technique: A Case Report. JBJS Case Connect. 2019;9:e0404. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Hardes J, Gebert C, Schwappach A, Ahrens H, Streitburger A, Winkelmann W, Gosheger G. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg. 2006;126:289-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |