Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6698
Peer-review started: June 18, 2023
First decision: August 10, 2023
Revised: August 23, 2023
Accepted: September 7, 2023
Article in press: September 7, 2023
Published online: October 6, 2023
Processing time: 99 Days and 9.9 Hours
The thoracic wall lesions, particularly chest wall tuberculosis, and chest wall tumors and other pyogenic wall and actinomycetes infections, almost always present as a diagnostic challenge.
To explore the value of ultrasound-guided biopsy combined with the Xpert Mycobacterium tuberculosis/resistance to rifampin (MTB/RIF) assay to diagnose chest wall tuberculosis.
We performed a retrospective study of patients with chest wall lesions from March 2018 to March 2021. All patients received the ultrasound-guided biopsy for pathology examination, acid-fast Bacillus staining, mycobacterial culture, and Xpert MTB/RIF analysis. The sensitivity, specificity, and area under the curve (AUC) were calculated for these diagnostic tests, either individually or combined. Rifampicin resistance results were compared between the mycobacterial culture and the Xpert MTB/RIF assay.
In 31 patients with the chest wall lesion biopsy, 22 patients were diagnosed with chest wall tuberculosis. Of them, 3, 6, and 21 patients tested positive for mycobacterial culture, acid-fast stain, and Xpert MTB/RIF assay, respectively. The rifampicin resistance results of the 3 culture-positive patients were consistent with their Xpert MTB/RIF assay results. When considering the sensitivity, specificity, and AUC value, the Xpert MTB/RIF assay (95.5%, 88.9%, and 0.92, respectively) was a better choice than the acid-fast Bacillus stain (27.3%, 100.0%, and 0.64, respectively) and mycobacterial culture (13.6%, 100.0%, 0.57, respectively). No complications were reported during the procedure.
Ultrasound guided biopsy combined with Xpert MTB/RIF has high value in the diagnosis of chest wall tuberculosis, and can also detect rifampicin resistance.
Core Tip: The thoracic wall lesions, particularly chest wall tuberculosis, and chest wall tumors and other pyogenic wall and actinomycetes infections, almost always present as a diagnostic challenge. Our study aims to explore the value of ultrasound guided biopsy combined with Xpert Mycobacterium tuberculosis/resistance to rifampin assay in the diagnosis of chest wall tuberculosis.
- Citation: Yan QH, Chi JY, Zhang L, Xue F, Cui J, Kong HL. Value of ultrasound guided biopsy combined with Xpert Mycobacterium tuberculosis/resistance to rifampin assay in the diagnosis of chest wall tuberculosis. World J Clin Cases 2023; 11(28): 6698-6706
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6698.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6698
Several studies have shown that, among all tuberculosis patients, the proportion of patients with extrapulmonary tuberculosis has steadily increased over the past two decades[1-3] due to improved diagnostic tests, such as imaging scans[2]. In 2019, extrapulmonary tuberculosis accounted for approximately 16% of all newly diagnosed tuberculosis worldwide[4]. Extrapulmonary tuberculosis can affect every organ and tissue structure, with the most common location at the lymph nodes, followed by the pleural space. Chest wall tuberculosis is one type of extrapulmonary tuberculosis that accounts for 1%-2% of all tuberculosis[5,6]. The thoracic wall lesions, particularly chest wall tumors and other pyogenic wall and actinomycetes infections, almost always present as a diagnostic challenge. Studies have reported that chest wall tuberculosis is often a sign of severe and disseminated tuberculosis[7,8] or is secondary to or occurs simultaneously with pulmonary tuberculosis or pleural tuberculosis[9]. Chest wall tuberculosis is a chest wall disease characterized by the formation of cold abscess masses. It is often caused by the primary lesion of the lung or pleura invading the chest wall lymph nodes, and then penetrating the lymph nodes to surrounding tissues in the chest wall[10]. Without appropriate treatments, the infection can form abscesses in the chest wall and destroy the ribs with subsequent developments of a sinus or fistula. Skeletal lesions are often caused through blood pathways[11]. Primary chest wall tuberculosis is rarely reported after the Bacillus-Calmette-Guerin vaccination. Color Doppler ultrasound is easy to detect the location, size, internal echo intensity, and blood flow of chest wall tuberculosis. It can accurately provide the depth and range of the involved surrounding tissues, and can clearly display the course and distribution of sinus fistula. The stage of the lesion can be evaluated based on the characteristics of the ultrasound image. However, ultrasound has difficulty in differentiating chest wall tuberculosis from chest tumors and other purulent infections. A definitive diagnosis requires biopsy and pathology evaluations.
The traditional method to diagnose tuberculosis requires the acid-fast Bacilli stain or mycobacterial culture. When diagnosing a patient with the suspected chest wall tuberculosis, ultrasound-guided biopsy is a safe method to localize the lesion for further pathology examinations. GeneXpert Mycobacterium tuberculosis/resistance to rifampin (MTB/RIF) technology is a semi-nested real-time fluorescence quantitative polymerase chain reaction in vitro diagnostic technology developed by Cepheid Company in the United States. The rifampicin resistance gene rpoB can be used as a target gene to simultaneously detect MTB and evaluate its resistance to rifampicin within 2 h[12]. This method was recommended by the World Health Organization (WHO) for the diagnosis of pulmonary tuberculosis in 2010[13,14]. In 2013, the WHO recommended it for the diagnosis of extrapulmonary tuberculosis. In recent years, an increasing number of studies have reported to use GeneXpert MTB for the diagnosis of various extrapulmonary tuberculosis, such as bone tuberculosis, tuberculous pleurisy, urinary tract tuberculosis, tuberculous meningitis[15-18]. However, there are limited reports on the diagnostic accuracy and safety of the combined ultrasound-guided biopsy and Xpert MTB/RIF assay to diagnose chest wall tuberculosis.
In the present study, we investigated the benefits and risks of combining the ultrasound-guided biopsy with the Xpert MTB/RIF assay to diagnose chest wall tuberculosis.
We performed a retrospective study at the Shandong Public Health Clinical Center, China, from March 2018 to March 2021. We conducted this study on August 26. Patients with chest wall tuberculosis received the ultrasound-guided biopsy and laboratory examinations. The study protocol was approved by the ethics committee of Shandong Public Health Clinical Center, Shandong Chest Hospital, (2021XKYYEC-23). All study steps adhered to the principles of the Declaration of Helsinki.
After reviewing the hospital patient records, we selected the study participants who received the ultrasound-guided biopsy and subsequent laboratory examinations, including pathology, acid-fast Bacillus stain, mycobacterial culture, and Xpert MTB/RIF analysis. Patients who received the anti-tuberculosis treatment prior to the biopsy or had incomplete medical records were excluded from the current study. Of the 22 selected patients, there were 13 males and 9 females with a mean age of 39.7 years ± 16.1 years (ranging from 16-67 years old).
Tuberculosis was diagnosed based on the WHO guidelines[19] and Chinese Medical Association Tuberculosis Clinical Diagnostic Standard[20]. Patients were clinically diagnosed with tuberculosis according to the following criteria: (1) Exhibited clinical tuberculosis symptoms; (2) had typical image findings consistent with tuberculosis; and (3) showed satisfactory responses to the anti-tuberculosis treatment. The patients’ ages, genders, laboratory examination results, treatment outcomes, and complications during the biopsy were retrieved from the medical records.
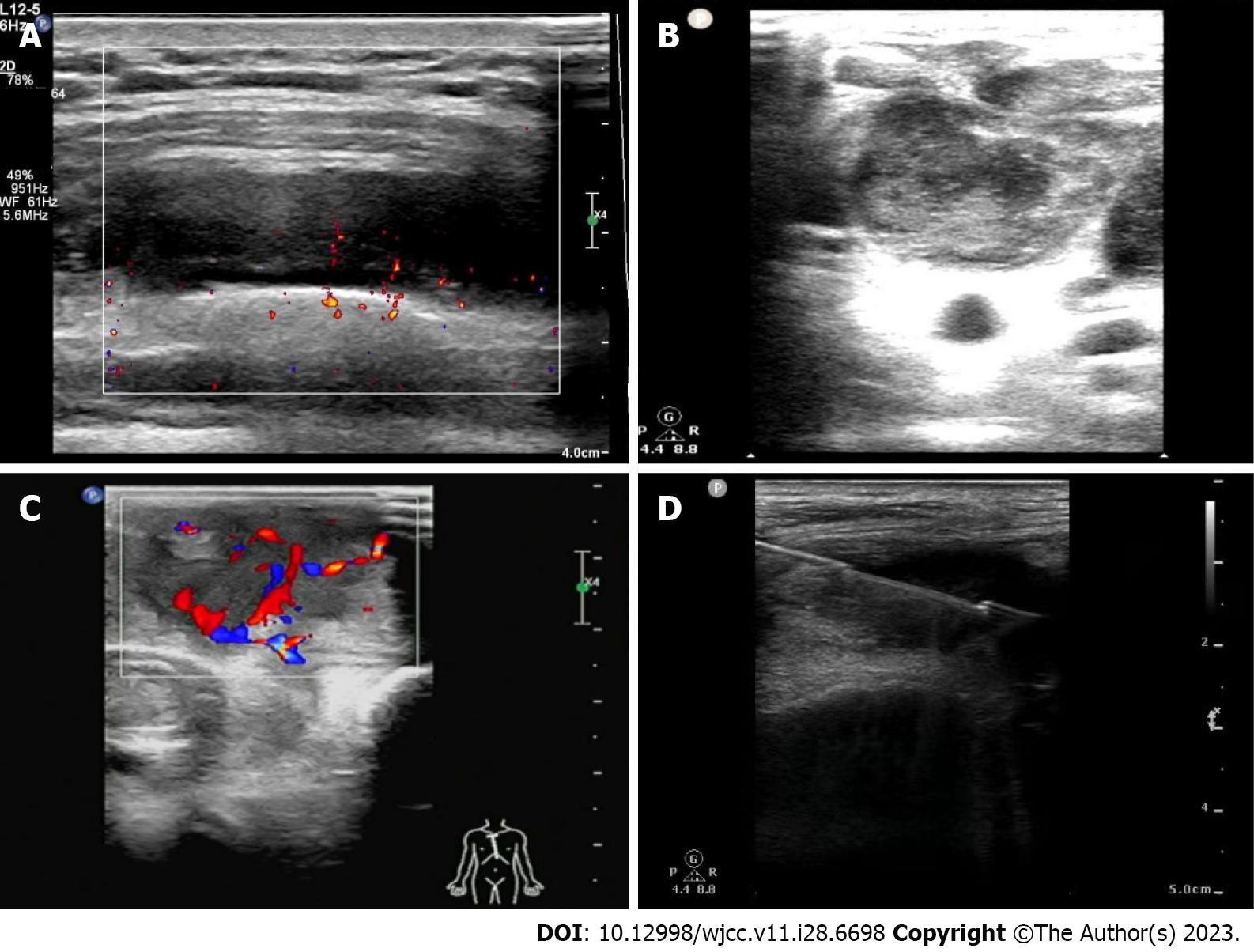
All biopsy procedures were performed by experienced ultrasonographers with the necessary technique skills for the ultrasound-guided biopsy. A Philips q7c ultrasound machine (Philips, Netherlands) was used for the procedure. The probe frequency was selected at 5-12 MH. The patient was placed in the supine, lateral, or sitting position according to the location of the lesion. The biopsy site was routinely disinfected, covered with the sterile towels, and locally anesthetized with 2% lidocaine. All biopsies were performed with a semi-automatic cutting biopsy needle (18G, 10-cm, Becton, Dickinson and Company, United States). The biopsy needle was slowly inserted into the lesion under continuous real-time ultrasound monitoring. Two or three punctures were performed in each patient for one biopsy (Figure 1). The specimens from the biopsy were sent for routine pathology, acid-fast Bacillus stain, BACTEC MGIT 960 mycobacterial culture, and Xpert MTB MTB/RIF assay.
A pathological examination was performed in the 4 μm-thick slides sectioned from the chest wall specimens after being fixed with 10% formalin and embedded in paraffin. After the hematoxylin and eosin staining, the slides were inspected by two pathologists. Microscopic lesions that showed typical epithelial cell granulomas, Langlie Hans cells, and caseous necrosis, as well as fibrosis and calcification, were considered as the typical pathological characteristics of tuberculosis.
Laboratory tests included: (1) Acid-fast Bacillus stain; (2) mycrobacterial culture; and (3) Xpert MTB/RIF detection. For the acid-fast, stain, we used the improved alkaline reddening method and acid-fast staining solution and evaluated the results according to the instructions from the manufacture (Zhuhai beso, China). For the mycobacterial culture, a BACTEC MGIT 960 mycobacterial culture monitoring system and supporting reagents (Becton, Dickinson and Company, United States) were used for the strain identification. For Xpert MTB/RIF detection, the pathological specimens were homogenized with a micro grinder fast-prep-24 (MP biomedicals, United States) after adding an appropriate amount of phosphate buffer[21]. Then, an Xpert detection reaction box and automatic detection platform (Cepheid, United States) were used to detect the samples and obtain results. Xpert MTB/RIF detection is based on semi-nested PCR technology, fully automatic amplification of nucleic acid, and automatic fluorescence detection[22].
All data were entered into Excel 2010 (Microsoft, United States). Statistical analyses were performed in SPSS (version 24.0, IBM, United States). Continuous data are presented as mean with standard deviation (mean ± SD) or median with interquartile range (mean ± IQR), depending on the normality test results. Categorical data are presented as a frequency or ratio. Student t-test or Chi-square analysis were used when appropriate. McNemar’s Chi-square test was used to compare the different diagnostic tests, where P < 0.05 was considered statistically significant.
In 31 patients who underwent chest wall lesion biopsy, 22 patients (13 males and 9 females; mean age of 39.7 years ± 16.1 years, ranging 16-67 years) were diagnosed as chest wall tuberculosis. Of them, 8 (36.4%), 6 (27.3%), 2 (9.1%), and 5 (22.7%) patients exhibited local pain, mass with fluctuation, abscess rupture, and fever, respectively. In addition, 14 patients had concurrent pulmonary tuberculosis, and 18 patients had concurrent pleural tuberculosis.
Based on the internal echo, the ultrasonic characteristics of chest wall tuberculosis were grouped into three types: (1) The solid echo type was found in 6 patients (27.3%), in which lesions were mostly disc-shaped or oval solid hypoechoic and limited to the subcutaneous soft tissue or intercostal space of the chest wall. Patchy strong echo was found in 2 patients (9.1%); (2) The liquid dark area type was observed in 4 patients (18.2%), in which most of the lesions were irregular liquid dark echo with weak fine dot hyperechos, and clear boundary with the surrounding tissues; and (3) The mixed echo type was seen in 12 patients (54.5%), where lesions were mostly circular and quasicircular mixed echo, with an unclear boundary, irregular shape, and a small amount of liquid dark area.
All 22 patients successfully completed the ultrasound-guided chest wall biopsy. The length of the puncture tissue strip was 0.5-1.8 cm. The patients were finally diagnosed with chest wall tuberculosis based on clinical, imaging, and laboratory examination.
Among the 22 patients, 3, 6, and 21 patients were positive for the mycobacterial culture, acid-fast stain, and Xpert MTB/RIF (Table 1), with positive diagnostic rates of 13.6%, 27.3%, and 95.5%, respectively. The Xpert MTB/RIF assay having the highest positive rate. All 3 patients with positive results for the mycobacterial culture also tested positive in the Xpert MTB/RIF assay. The rifampicin resistance results in these 3 patients were consistent with the results of the Xpert MTB/RIF assay. The 5 patients with negative results of mycobacterial culture and acid-fast stain tested positive in the Xpert MTB/RIF assay. The Xpert MTB/RIF assay increased the pathogenic positive detection rate by 22.7% (5/22) (Table 2). The kappa values of the Xpert MTB/RIF assay, acid-fast stain, and mycobacterial culture were 0.84, 0.18, and 0.08, respectively. The area under the curve (AUC) values of the Xpert MTB/RIF assay, acid-fast stain, and mycobacterial culture were 0.92, 0.64, and 0.57, respectively (Figure 2). The AUC and kappa value of the combined test by the pathology examination and the Xpert MTB/RIF assay had the highest positive diagnostic rate of 100.0%, with AUC = 0.94 and kappa = 0.92.
| Detection techniques | Results | Clinical comprehensive diagnosis (n) | ||
| Chest wall tuberculosis | Non chest wall tuberculosis | Total | ||
| Pathology | Positive | 18 | 0 | 18 |
| Negative | 4 | 9 | 13 | |
| Total | 22 | 9 | 31 | |
| Acid-fast stain | Positive | 6 | 0 | 6 |
| Negative | 16 | 9 | 25 | |
| Total | 22 | 9 | 31 | |
| Mycobacterial culture | Positive | 3 | 0 | 3 |
| Negative | 19 | 9 | 28 | |
| Total | 22 | 9 | 31 | |
| Xpert MTB/RIF | Positive | 21 | 1 | 22 |
| Negative | 1 | 8 | 9 | |
| Total | 22 | 9 | 31 | |
| Pathology and acid-fast stain | Positive | 18 | 0 | 18 |
| Negative | 4 | 9 | 13 | |
| Total | 22 | 9 | 31 | |
| Pathology and mycobacterial culture | Positive | 18 | 0 | 18 |
| Negative | 4 | 9 | 13 | |
| Total | 22 | 9 | 31 | |
| Pathology and Xpert MTB/RIF | Positive | 22 | 1 | 23 |
| Negative | 0 | 8 | 8 | |
| Total | 22 | 9 | 31 | |
| Detection techniques | AUC | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Kappa value | P value | Total coincidence rate (%) | Jordan index |
| Pathology | 0.909 | 81.8% | 100.0% | 100.0% | 69.2% | 0.723 | 0.000 | 87.1% | 81.8% |
| Acid-fast stain | 0.636 | 27.3% | 100.0% | 100.0% | 36.0% | 0.179 | 0.081 | 48.4% | 27.3% |
| Mycobacterial culture | 0.568 | 13.6% | 100.0% | 100.0% | 32.1% | 0.084 | 0.244 | 38.7% | 13.6% |
| Xpert MTB/RIF | 0.922 | 95.5% | 88.9% | 95.5% | 88.9% | 0.843 | 0.000 | 93.6% | 84.3% |
| Pathology and acid-fast stain | 0.909 | 81.8% | 100.0% | 100.0% | 69.2% | 0.723 | 0.000 | 87.1% | 81.8% |
| Pathology and mycobacterial culture | 0.909 | 81.8% | 100.0% | 100.0% | 69.2% | 0.723 | 0.000 | 87.1% | 81.8% |
| Pathology and Xpert MTB/RIF | 0.944 | 100.0% | 88.9% | 95.7% | 100.0% | 0.913 | 0.000 | 96.8% | 88.9% |
One patient displayed the pleural reaction with nausea, vomiting, and dizziness during the puncture, which resolved after the symptomatic treatments and bed rest. No patients required closed thoracic drainage or an extended hospital stay. There were no other complications reported.
Pulmonary tuberculosis is the main type of tuberculosis disease, for which diagnosis is mainly based on the respiratory specimens. Patients with extrapulmonary tuberculosis but without any respiratory symptoms always present a diagnostic challenge. As the incidence of chest wall tuberculosis is relatively low, most cases are caused by secondary infection due to the tuberculosis foci from the lung or pleural space directly spreading to the chest wall after penetrating the pleura. Secondary infection can also occur when pulmonary tuberculosis or pleural tuberculosis invades the lymph nodes in the chest wall through the lymphatic system, then infiltrates the surrounding tissues in the chest wall[8]. They can lead to the formation of an abscess, sinus, or fistula in the chest wall, subsequently damaging the ribs[23,24]. Typical chest wall tuberculosis can be diagnosed based on clinical presentations and ultrasonic characteristics. If it is not clear, ultrasound-guided biopsy can be performance, which is an important method to diagnose the chest wall tuberculosis.
Chest wall tuberculosis is frequently reported in young or middle-aged patients[25]. The present study included 13 males and 9 females, with a mean age of 39.7 (± 16.1) years, which is consistent with the previous report.
Tuberculosis commonly causes a chronic infection and pathological changes, such as inflammatory exudation, nodular hyperplasia, and caseous necrosis. The fibrosis and calcification can gradually progress as the disease advances, which can further affect the pathological and ultrasonic findings[26]. Among the 22 patients, 6, 4, and 12 patients had the solid echo, liquid dark area, and mixed echo type of ultrasound images, respectively. The solid echo type needs to be differentiated from the chest wall soft tissue tumor[27]. Chest wall tumors typically have an irregular shape, some of which can bulge from the body surface as a chest wall mass[28] or protrude toward the lung. During the ultrasound examination, the mass does not move with the aerated lung tissue. Therefore, Color Doppler ultrasound is used to accurately measure the depth and extent of the mass, as well as potential penetrations into the surrounding tissues. It can also reveal the blood flow signals of the mass, which might be used to differentiate a tumor (rich signals) from tuberculosis infection (poor signals). The type of liquefied dark area in the chest wall should be distinguished from the abscess due to other pathogenic bacteria that mostly cause local and systemic symptoms. The mixed echo type should be differentiated from a metastatic tumor of the chest wall and primary bone tumor. Metastatic tumors of the chest wall are often not accompanied by calcification, while primary bone tumors mainly present with bone destruction and less soft tissue masses. Chest wall tuberculosis can easily cause sinus formation. In the present study, 15 patients exhibited sinus formation that was connected with the pleural lesions, presenting as a dumbbell lesion[29]. Considering the advantages of accuracy, real-time, and small trauma, ultrasound-guided puncture biopsy can be used to obtain specimens from chest wall lesions for further pathological examinations and laboratory tests when chest wall tuberculosis diagnosis is in question[30].
The Xpert MTB/RIF assay is a diagnostic test to detect the MTB DNA. When the MTB is found, the rifampicin resistance related to mutation of the rpoB gene is also examined. The test results can be obtained within 2 h, which can help achieve an early and rapid diagnosis, effectively avoid cross-contamination, and be less impacted by the anti-tuberculosis treatments[31]. Herein, we calculated the sensitivity, specificity, and AUC for the acid-fast stain, mycobacterial culture, and Xpert MTB/RIF assay in the diagnosis of chest wall tuberculosis (Table 2). The AUC value of the Xpert MTB/RIF assay was higher than that of the acid-fast staining, while the latter was higher than the mycobacterial culture. This suggests that the Xpert MTB/RIF assay has the high diagnostic value in chest wall tuberculosis. In addition, we also analyzed the diagnostic accuracy of the pathology examination combined with the three laboratory tests. Among them, the pathology examination combined with the Xpert MTB/RIF assay gave the best results, with a sensitivity of 100.0%, AUC value of 0.94, and kappa value of 0.92. Many previous studies have reported the diagnostic value of the Xpert MTB/RIF assay in extrapulmonary tuberculosis. For example, the sensitivity and specificity of the Xpert MTB/RIF assay in the diagnosis of lymph node tuberculosis were 74.4%-87.8% and 91.1%, respectively, which were significantly higher than those of smear microscopy and cytology[32,33]. Moreover, the sensitivity and specificity of the Xpert MTB/RIF assay in the diagnosis of bone and joint tuberculosis were reported to be 82.0% and 100.0%, respectively[15]. In addition, the Xpert MTB/RIF assay has been suggested as the gold standard diagnostic criterion for tuberculous pleurisy and tuberculous pericarditis, since it showed a high sensitivity (90.0% and 72.0%, respectively) and specificity (100.0% and 100.0%, respectively)[17]. Our current study further confirms the important clinical application of combing the pathology examination with the Xpert MTB/RIF assay in the diagnosis of chest wall tuberculosis.
No major complication was reported in our study. Ultrasound-guided biopsy was performed under direct visualization to observe the lesion and blood supply, as well as monitor the position of the needle in the real-time to ensure the accuracy and safety of the puncture. Therefore, ultrasound-guided biopsy is a safe procedure to perform in patients with suspected chest wall tuberculosis.
The limitations of our study included its small sample size, retrospective design, and single center research. In addition, a contrast-enhanced ultrasound or ultrasound elastography guided biopsy may facilitate the puncture and make the biopsy more accurate. Future multicenter prospective studies are required to confirm our study findings here.
Ultrasound guided biopsy combined with Xpert MTB/RIF detection can accurately and safely diagnose chest wall tuberculosis, while also determining rifampicin resistance with high sensitivity and specificity.
The thoracic wall lesions, particularly chest wall tuberculosis, and chest wall tumors and other pyogenic wall and actinomycetes infections, almost always present as a diagnostic challenge.
Color Doppler ultrasound is easy to detect the location, size, internal echo intensity, and blood flow of chest wall tuberculosis. It can accurately provide the depth and range of the involved surrounding tissues, and can clearly display the course and distribution of sinus fistula. The stage of the lesion can be evaluated based on the characteristics of the ultrasound image. However, ultrasound has difficulty in differentiating chest wall tuberculosis from chest tumors and other purulent infections. A definitive diagnosis requires biopsy and pathology evaluations.
We investigated the benefits and risks of combining the ultrasound-guided biopsy with the Xpert MTB/RIF assay to diagnose chest wall tuberculosis.
We performed a retrospective study of patients with chest wall lesions from March 2018 to March 2021. All patients received the ultrasound-guided biopsy for pathology examination, acid-fast Bacillus staining, mycobacterial culture, and Xpert MTB/RIF analysis. The sensitivity, specificity, and area under the curve (AUC) were calculated for these diagnostic tests, either individually or combined. Rifampicin resistance results were compared between the mycobacterial culture and the Xpert MTB/RIF assay.
Patients (3, 6, and 21) tested positive for mycobacterial culture, acid-fast stain, and Xpert MTB/RIF assay, respectively. The rifampicin resistance results of the 3 culture-positive patients were consistent with their Xpert MTB/RIF assay results. When considering the sensitivity, specificity, and AUC value, the Xpert MTB/RIF assay (95.5%, 88.9%, and 0.92, respectively) was a better choice than the acid-fast Bacillus stain (27.3%, 100.0%, 0.64, respectively) and mycobacterial culture (13.6%, 100.0%, 0.57, respectively). No complications were reported during the procedure.
Ultrasound guided biopsy combined with Xpert MTB/RIF has high value in the diagnosis of chest wall tuberculosis, and can also detect rifampicin resistance.
The precise, safe, and minimally invasive characteristics of ultrasound-guided puncture are combined with advanced genetic testing technology Xpert MTB/RIF technology to diagnose chest wall tuberculosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin S, Turkey S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 434] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 2. | Sandgren A, Hollo V, van der Werf MJ. Extrapulmonary tuberculosis in the European Union and European Economic Area, 2002 to 2011. Euro Surveill. 2013;18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Wang X, Yang Z, Fu Y, Zhang G, Wang X, Zhang Y. Insight to the Epidemiology and Risk Factors of Extrapulmonary Tuberculosis in Tianjin, China during 2006-2011. PLoS One. 2014;9:e112213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, Kapata N, Mfinanga S, Hasnain SE, Katoto PDMC, Bulabula ANH, Sam-Agudu NA, Nachega JB, Tiberi S, McHugh TD, Abubakar I, Zumla A. Global Tuberculosis Report 2020 - Reflections on the Global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021;113 Suppl 1:S7-S12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 421] [Cited by in RCA: 571] [Article Influence: 142.8] [Reference Citation Analysis (0)] |
| 5. | Morris BS, Maheshwari M, Chalwa A. Chest wall tuberculosis: a review of CT appearances. Br J Radiol. 2004;77:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Abid H, Toujani S, Ammar J, Marghli A, Slim L, Hantous S, Ayadi A, Hamzaoui A. Chest swelling with adenopathy: Don't forget tuberculosis. Respirat Med CME. 2011;4:47-49. [DOI] [Full Text] |
| 7. | Boruah DK, Sanyal S, Sharma BK, Prakash A, Dhingani DD, Bora K. Role of Cross Sectional Imaging in Isolated Chest Wall Tuberculosis. J Clin Diagn Res. 2017;11:TC01-TC06. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Kabiri EH, Alassane EA, Kamdem MK, Bhairis M, Amraoui M, El Oueriachi F, El Hammoumi M. Tuberculous cold abscess of the chest wall: A clinical and surgical experience. Report of 16 cases(Case series). Ann Med Surg (Lond). 2020;51:54-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Sakuraba M, Sagara Y, Komatsu H. Surgical treatment of tuberculous abscess in the chest wall. Ann Thorac Surg. 2005;79:964-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Jang T, Aubin C, Sineff S, Naunheim R. Ultrasound training. Acad Emerg Med. 2003;10:1144-1145. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Swanson SJ. Commentary: The tale of technology: Extending the boundaries of thoracic surgery. JTCVS Tech. 2021;10:577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Rice JP, Seifert M, Moser KS, Rodwell TC. Performance of the Xpert MTB/RIF assay for the diagnosis of pulmonary tuberculosis and rifampin resistance in a low-incidence, high-resource setting. PLoS One. 2017;12:e0186139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | New diagnostic test changes tuberculosis landscape. Bull World Health Organ. 2013;91:163-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005;72:1761-1768. [PubMed] |
| 15. | Gu Y, Wang G, Dong W, Li Y, Ma Y, Shang Y, Qin S, Huang H. Xpert MTB/RIF and GenoType MTBDRplus assays for the rapid diagnosis of bone and joint tuberculosis. Int J Infect Dis. 2015;36:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Held M, Laubscher M, Workman L, Zar HJ, Dunn R. Diagnostic accuracy of GeneXpert MTB/RIF in musculoskeletal tuberculosis: High sensitivity in tissue samples of HIV-infected and HIV-uninfected patients. S Afr Med J. 2017;107:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Saeed M, Ahmad M, Iram S, Riaz S, Akhtar M, Aslam M. GeneXpert technology. A breakthrough for the diagnosis of tuberculous pericarditis and pleuritis in less than 2 hours. Saudi Med J. 2017;38:699-705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Bahr NC, Marais S, Caws M, van Crevel R, Wilkinson RJ, Tyagi JS, Thwaites GE, Boulware DR; Tuberculous Meningitis International Research Consortium. GeneXpert MTB/Rif to Diagnose Tuberculous Meningitis: Perhaps the First Test but not the Last. Clin Infect Dis. 2016;62:1133-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | World Health Orgnazation. Tuberculosis (TB). [cited 12 August 2023]. Available from: https://www.who.int/tb/areas-of-work/Laboratory/en/. |
| 20. | Chinese Medical Association. Clinical diagnosis standardof TB for clinicaltechnologyoperation (TBvol-umes). People’s Medical Publishing House. 2005. [DOI] [Full Text] |
| 21. | Grosser M, Dittert DD, Luther T. Re: Molecular detection of M. tuberculosis DNA in tuberculosis and sarcoidosis. Diagn Mol Pathol. 2001;10:66-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Telenti A, Imboden P, Marchesi F, Lowrie D, Cole S, Colston MJ, Matter L, Schopfer K, Bodmer T. Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet. 1993;341:647-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 919] [Cited by in RCA: 859] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 23. | Yuan X, Zhang J, Quan C, Cao J, Ao G, Tian Y, Li H. Differentiation of malignant and benign pulmonary nodules with first-pass dual-input perfusion CT. Eur Radiol. 2013;23:2469-2474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Keum DY, Kim JB, Park CK. Surgical treatment of a tuberculous abscess of the chest wall. Korean J Thorac Cardiovasc Surg. 2012;45:177-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Zhang ZX, Gao JB, Yang XH, Zhou ZG, Guo H, Yue SW, Gao YG, Gao J. Multi slice spiral CT diagnosis of chest wall tuberculosis. Yiyao Luntan Zazhi. 2010;31. [DOI] [Full Text] |
| 26. | Li JR, Duan XQ. Clinical value of high frequency color Doppler ultrasound in the diagnosis of chest wall tuberculosis. Jiceng Yixue Luntan. 2013;17:226-227. [DOI] [Full Text] |
| 27. | Li W, Sha W. Diagnosis of Chest Wall Tuberculosis Using Fine Needle Aspiration: A Single-Center Experience. Infect Drug Resist. 2023;16:2281-2290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 28. | Liu JX, Qin XB. A case report and literature review of anterior mediastinal rhabdomyosarcoma. Shiyong Yiyuan Linchuang Zazhi. 2012;9:247-248. [DOI] [Full Text] |
| 29. | Manios Y, Moschonis G, Karatzi K, Androutsos O, Chinapaw M, Moreno LA, Bere E, Molnar D, Jan N, Dössegger A, De Bourdeaudhuij I, Singh A, Brug J; ENERGY Consortium. Large proportions of overweight and obese children, as well as their parents, underestimate children's weight status across Europe. The ENERGY (EuropeaN Energy balance Research to prevent excessive weight Gain among Youth) project. Public Health Nutr. 2015;18:2183-2190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Chandrasekhar AJ, Reynes CJ, Churchill RJ. Ultrasonically guided percutaneous biopsy of peripheral pulmonary masses. Chest. 1976;70:627-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Meldau R, Peter J, Theron G, Calligaro G, Allwood B, Symons G, Khalfey H, Ntombenhle G, Govender U, Binder A, van Zyl-Smit R, Dheda K. Comparison of same day diagnostic tools including Gene Xpert and unstimulated IFN-γ for the evaluation of pleural tuberculosis: a prospective cohort study. BMC Pulm Med. 2014;14:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 32. | Laushkina ZA, Krasnov VA, Cherednichenko AG. Diagnostic value of gene xpert mtb-rif in tuberculosis control practice. Tuberkulez i Bolezni Lëgkih. 2016;94:37-39. [DOI] [Full Text] |
| 33. | Tadesse M, Abebe G, Abdissa K, Aragaw D, Abdella K, Bekele A, Bezabih M, Apers L, de Jong BC, Rigouts L. GeneXpert MTB/RIF Assay for the Diagnosis of Tuberculous Lymphadenitis on Concentrated Fine Needle Aspirates in High Tuberculosis Burden Settings. PLoS One. 2015;10:e0137471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |