Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6613
Peer-review started: June 28, 2023
First decision: August 5, 2023
Revised: August 9, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: September 26, 2023
Processing time: 84 Days and 7 Hours
Internal hernia is a rare cause of acute abdomen and intestinal obstruction in adults. Internal abdominal hernias include paraduodenal, perigastric, foramen of Winslow, intersigmoid, and post-anastomotic hernias and can be congenital or acquired. Internal hernias occur in 1%-2% of patients, and transmesocolic hernias are extremely rare. This report presents a patient with a transverse mesocolic hernia with a preoperative diagnosis of small intestinal obstruction.
A 45-year-old Chinese woman was admitted to the hospital with middle and upper abdominal pain for 2 d, abdominal distension, and vomiting. After abdominal computed tomography, she was diagnosed with an internal abdominal hernia complicated by small intestinal obstruction and underwent emergency laparoscopic surgery. The patient recovered well and was discharged 6 d postoperatively.
Transmesocolic hernias must be considered in adult patients with signs and symptoms of intestinal obstruction, even without a history of abdominal trauma or surgery.
Core Tip: Transverse mesocolic hernia with intestinal obstruction is a rare cause of acute abdomen in adults. This case emphasizes the importance of considering a diagnosis of transmesocolic hernia in adult patients with intestinal obstruction, even in the absence of a history of abdominal trauma or surgery. Intraoperative images and video included with this case report highlight the surgical procedures required to treat these rare hernias.
- Citation: Zhang C, Guo DF, Lin F, Zhan WF, Lin JY, Lv GF. Transverse mesocolic hernia with intestinal obstruction as a rare cause of acute abdomen in adults: A case report. World J Clin Cases 2023; 11(27): 6613-6617
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6613.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6613
Transmesenteric hernias are extremely rare. Approximately 0.6%-5.8% of all small intestinal obstructions are due to internal abdominal hernias[1], and transmesocolic hernias account for approximately 5%-10% of all internal abdominal hernias[2]. The overall mortality rate of strangulated small intestinal obstruction is over 50%. In adults, transmesocolic hernias are usually caused by previous abdominal surgery, abdominal trauma, or intraperitoneal inflammation. It is extremely rare for a patient with no history of abdominal surgery to develop a transmesocolic hernia[3]. This report presents the case of a patient with a transmesocolic hernia accompanied by an incarcerated small intestine.
Middle and upper abdominal pain for 2 d.
A 45-year-old Chinese woman with no history of abdominal surgery was admitted to the hospital with middle and upper abdominal pain for 2 d, abdominal distension, and vomiting.
Upon admission, her blood pressure was 137/82 mmHg, heart rate was 87 beats/min, and body temperature was 36.7 °C. A physical examination of the abdomen revealed tenderness in the middle and upper abdomen without rebound pain.
Upon admission, laboratory assessments revealed a white blood cell count of 10.6 × 109/L (NEUT%, 84.4%); haemoglobin concentration of 121 g/L; platelet count of 10.6 × 109/L; C-reactive protein of 15 mg/dL; sodium of 134 mmol/L; potassium of 3.7 mmol/L; aspartate aminotransferase of 39 U/L; alanine aminotransferase of 51 U/L; alkaline phosphatase of 86 U/L; lactate dehydrogenase of 195 U/L; blood urea nitrogen of 5.97 mmol/L; and creatinine of 62 umol/L.
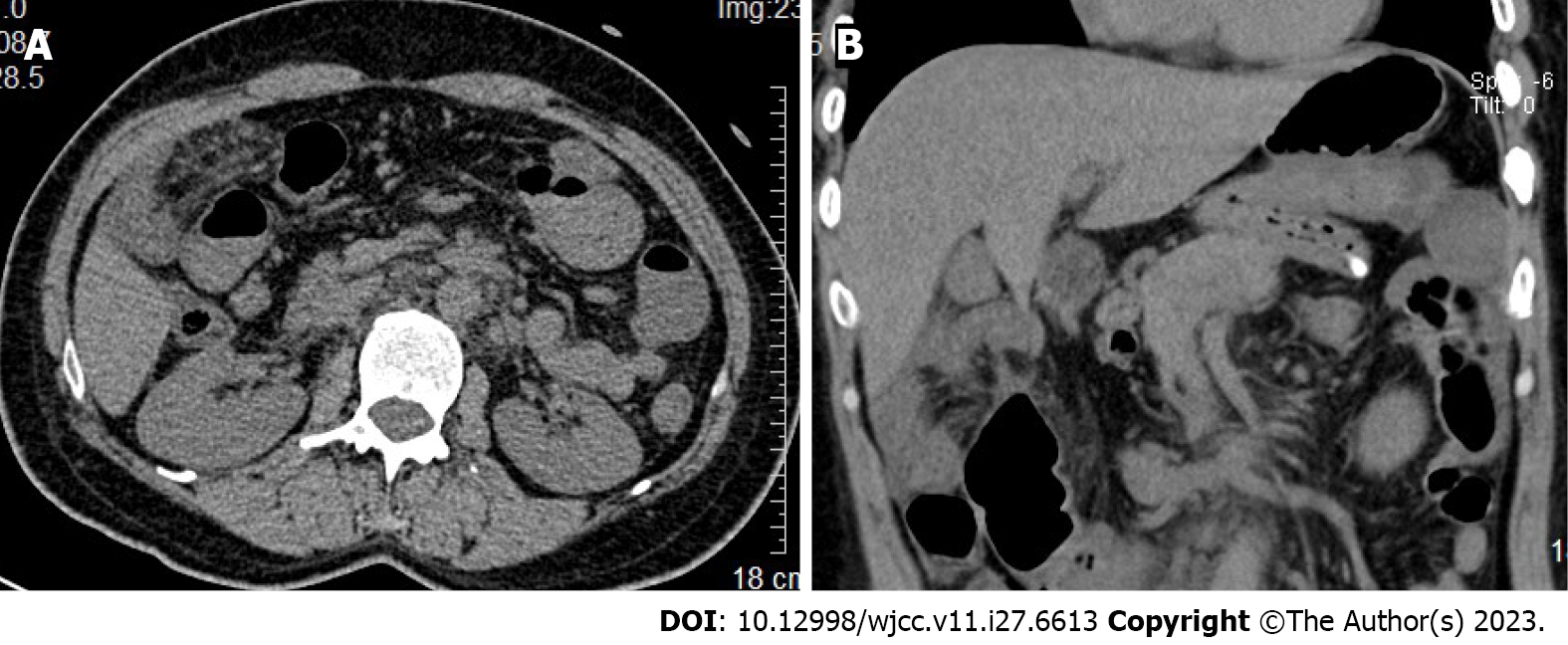
Abdominal computed tomography (CT) revealed local intestinal dilation in the abdominal cavity, thickening of the intestinal tube wall, an abnormal location and disordered arrangement of the small intestine, and partial thickening and edema of the intestinal wall and mesangium above the transverse colon near the hepatoduodenal ligament and gallbladder (Figure 1).
An internal abdominal hernia with small intestinal obstruction was suspected.
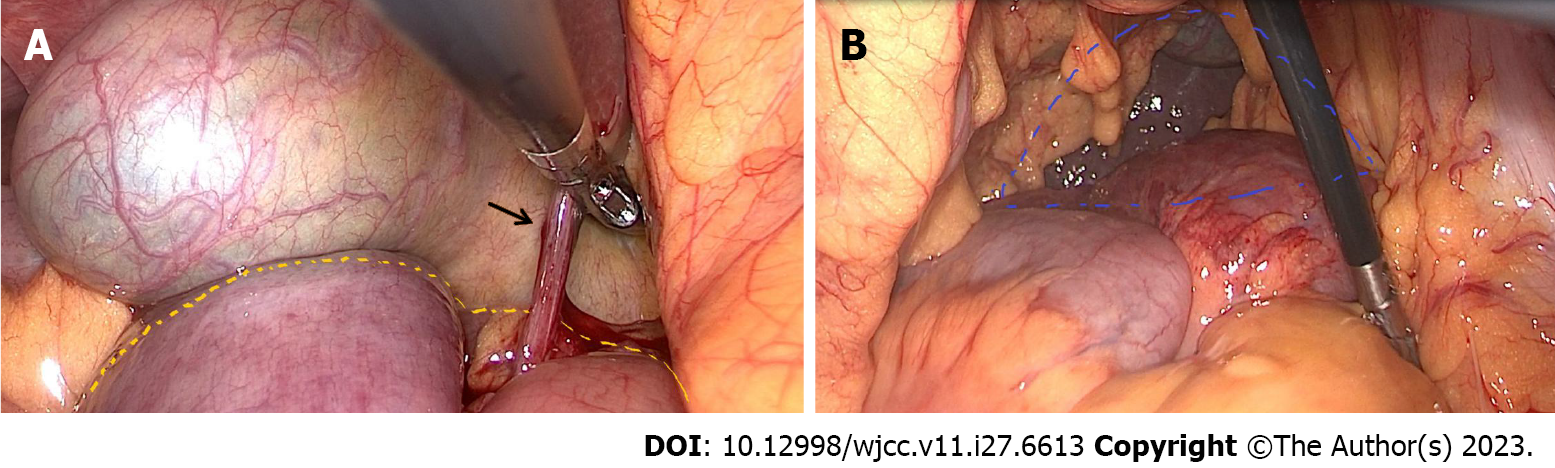
The patient underwent emergency laparoscopic surgical exploration. Intraoperatively, the small intestine was discovered to be herniated from the mesocolon defect below the transverse colon to the lower part of the liver and gallbladder and was trapped by an adhesive band between the liver and duodenum. The entrapment intestinal obstruction involved a trapped small intestine and mesocolon, a loosened adhesive band, and the entrapment of the small intestine because of the mesocolon defect below the transverse colon. The defect area of the transverse mesocolon was approximately 25 cm2. The blood flow within the small intestine recovered well, and no intestinal resection or anastomosis was required (Figure 2). The small intestinal obstruction in this patient was closely related to adhesive tape entrapment. An intraoperative evaluation revealed that the mesocolic defect in this patient was large and that the possibility of recurrence of small intestinal obstruction was minimal, so the decision was made not to repair the mesocolic defect during the operation.
The patient was discharged on postoperative day 6 with a favourable outpatient follow-up at 6 mo postoperatively (Figure 3).
An internal abdominal hernia involves the protrusion of an abdominal organ through a normal or abnormal mesentery or peritoneal pore[4]. Internal hernias may occur because of trauma, surgical procedures, or other reasons related to congenital peritoneal defects. Internal hernias with unique clinical and imaging features are classified according to their anatomical regions: Paraduodenal (left or right) (53%), foramen of Winslow (8%), cecum (13%), sigmoid colon (6%), intestinal membrane (8%), interventricular (1%-4%), and anastomotic, bladder, and pelvic (6%) hernias[5]. Transmesenteric hernias are difficult to diagnose preoperatively and typically require the removal of the affected intestinal area during surgery[6]. Few mesocolic hernias have been reported. Congenital mesocolic hernias have three types. The first two are the right and left types, comprising 25% and 75% of all cases, respectively. The third type is extremely rare and known as a transverse mesocolic hernia[7].
Congenital mesocolic defects are extremely rare, and previous studies have proposed theories regarding their congenital causes. Because mesenteric perforations and associated hernias are often found in infants with closed intestinal segments, they may be related to prenatal intestinal ischaemic accidents. In adults, mesenteric defects are caused mostly by previous gastrointestinal surgery, abdominal trauma, or intraperitoneal inflammation[8,9]. The presentation of a transverse mesocolic hernia in an adult with no history of trauma or prior abdominal surgery, as in this report, is rare.
A clear preoperative diagnosis is difficult in most patients with internal abdominal hernias because they have no obvious symptoms or signs. These hernias manifest mostly as abdominal pain, abdominal distension, and vomiting and cannot be distinguished from other acute abdominal diseases. Abdominal CT is a useful auxiliary diagnostic technique. With the patient presented in this report, CT revealed local intestinal dilation in the abdominal cavity, intestinal tube wall thickening, an abnormal location and disordered arrangement of the small intestine, intestinal wall thickening, edema, and mesangium above the transverse colon near the hepatoduodenal ligament and gallbladder. The small intestine is not typically located in this region. Therefore, this patient underwent an emergency laparoscopic operation to investigate an intraperitoneal hernia with small intestinal obstruction. For intraperitoneal hernias with mesocolic defects, most surgeons will choose to close the defect[10]. However, the small intestinal obstruction was closely related to adhesive tape entrapment in this patient. An intraoperative evaluation revealed that the mesocolic defect in this patient was large, and the possibility of recurrence of small intestinal obstruction was minimal, so a decision was made not to repair the mesocolic defect during the operation.
Transmesocolic hernias, especially transverse mesocolic hernias, are rare. Most previous reports of mesocolic hernias are case reports and involve open surgery. The surgical images provided in this report reflect the incarceration caused by the internal abdominal hernia. The patient had no history of abdominal trauma or surgery, and the laparoscopic emergency operation was successful. The surgical pictures (Figure 2) and videos (Video) provided in this report highlight the incarceration of the internal abdominal hernia, allowing readers to gain a better understanding of this condition and the required surgical treatment.
In conclusion, the preoperative diagnosis of intestinal obstruction caused by internal hernias, especially mesocolic hernias, remains difficult. Therefore, considering the possibility of transmesocolic hernias in adult patients with signs and symptoms of intestinal obstruction is important, even when the patient has no history of abdominal trauma or surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Seretis C, Greece; Viswanath YK, United Kingdom S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Agresta F, Mazzarolo G, Bedin N. Incarcerated internal hernia of the small intestine through a re-approximated peritoneum after a trans-abdominal pre-peritoneal procedure--apropos of two cases: review of the literature. Hernia. 2011;15:347-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 3. | Jung P, Kim MD, Ryu TH, Choi SH, Kim HS, Lee KH, Park JH. Transmesocolic hernia with strangulation in a patient without surgical history: case report. World J Gastroenterol. 2013;19:1997-1999. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Mathieu D, Luciani A; GERMAD Group. Internal abdominal herniations. AJR Am J Roentgenol. 2004;183:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 89] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Gomes R, Rodrigues J. Spontaneous adult transmesentric hernia with bowel gangrene. Hernia. 2011;15:343-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Deger KC. Laparoscopic Reduction and Repair of a Mesocolic Hernia Causing Small Bowel Obstruction: A Case Report and Review of Literature. Cureus. 2023;15:e37421. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Shaffner Lde S, Pennell TC. Congenital internal hernia. Surg Clin North Am. 1971;51:1355-1359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Mock CJ, Mock HE Jr. Strangulated internal hernia associated with trauma. AMA Arch Surg. 1958;77:881-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |