Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6592
Peer-review started: June 26, 2023
First decision: August 10, 2023
Revised: August 22, 2023
Accepted: August 29, 2023
Article in press: August 29, 2023
Published online: September 26, 2023
Processing time: 86 Days and 13.9 Hours
Micrococcus luteus (M. luteus)-induced endophthalmitis is very rare and and may present as either acute or chronic postoperative endophthalmitis. The aim of this study was to report a case of delayed-onset M. luteus-induced endophthalmitis that occurred several months after cataract surgery.
A 78-year-old man presented with decreased vision, pain and redness in the right eye that had begun 3 days prior. He had undergone cataract surgery 4 mo prior. Visual acuity was counting fingers; slit-lamp examination revealed conjunctival injection, posterior corneal precipitates, anterior chamber inflammation (cell 4+), and hypopyon. Fundus examination revealed moderate vitreous haze. Urgent vitrectomy was performed for suspected infectious endophthalmitis, followed by vitreous irrigation with injections of antibiotics. On the postoperative day 1, anterior chamber cell decreased to 2+ and hypopyon was not observed on slit lamp examination. Six days postoperatively, the patient had recurrent eye pain, and the anterior chamber cell grade increased to 4+; hypopyon recurred in the anterior chamber, and whitish plaque was observed in the lens capsule. Therefore, the patient underwent intraocular lens (IOL) and lens capsule removal, followed by vitreous irrigation, antibiotics injection, and vitrectomy. M. luteus was identified from a lens capsule culture.
In cases of delayed-onset M. luteus-induced endophthalmitis, early vitrectomy and removal of the IOL and lens capsule may be necessary.
Core Tip:Micrococcus luteus (M. luteus)-induced endophthalmitis is very rare, and no case of delayed-onset M. luteus-induced endophthalmitis several months after phacoemulsification has been reported. Early vitrectomy, vitreous irrigation, antibiotic injection, and removal of the intraocular lens and lens capsule may be necessary to treat this condition.
- Citation: Nam KY, Lee HW. Delayed-onset micrococcus luteus-induced postoperative endophthalmitis several months after cataract surgery: A case report. World J Clin Cases 2023; 11(27): 6592-6596
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6592.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6592
Infectious endophthalmitis, pathogen-induced inflammation of the intraocular cavity, is a very severe eye disease with a poor visual prognosis. The routes of intraocular infection by pathogens in infectious endophthalmitis are broadly divided into exogenous and endogenous. The most common cause of exogenous infectious endophthalmitis is intraocular surgery[1]. Depending on the timing and characteristics of onset, postoperative endophthalmitis can be classified as acute or chronic (or delayed-onset). Acute endophthalmitis generally occurs within 6 wk postoperatively, while chronic endophthalmitis occurs > 6 wk postoperatively[2]. Acute endophthalmitis is 2- to 5-fold more common than chronic endophthalmitis[3]. Propionibacterium acnes is the most common causative pathogen in cases of chronic endophthalmitis (41%–63% of cases)[3].
Chronic endophthalmitis generally manifests as mild inflammation that persists and recurs; it begins as anterior chamber inflammation and gradually progresses to the posterior eye. Pain may not be present, but vision is usually impaired. The inflammation responds to steroid therapy, but it tends to recur when steroid treatment is reduced[3,4].
We encountered a case of chronic (or delayed-onset) micrococcus luteus (M. luteus)-induced endophthalmitis that encountered several months after cataract surgery. This pathogen is a very rare cause, and there have been few relevant reports. Here, we describe this case and review the existing literature.
The patient visited our ophthalmology clinic due to a visual impairment, pain, redness and discharge in the right eye.
The patient is a 78-year-old male and the symptoms had begun 3 d earlier.
The patient had undergone cataract surgery 4 mo prior.
The patient had hypertension, no history of trauma.
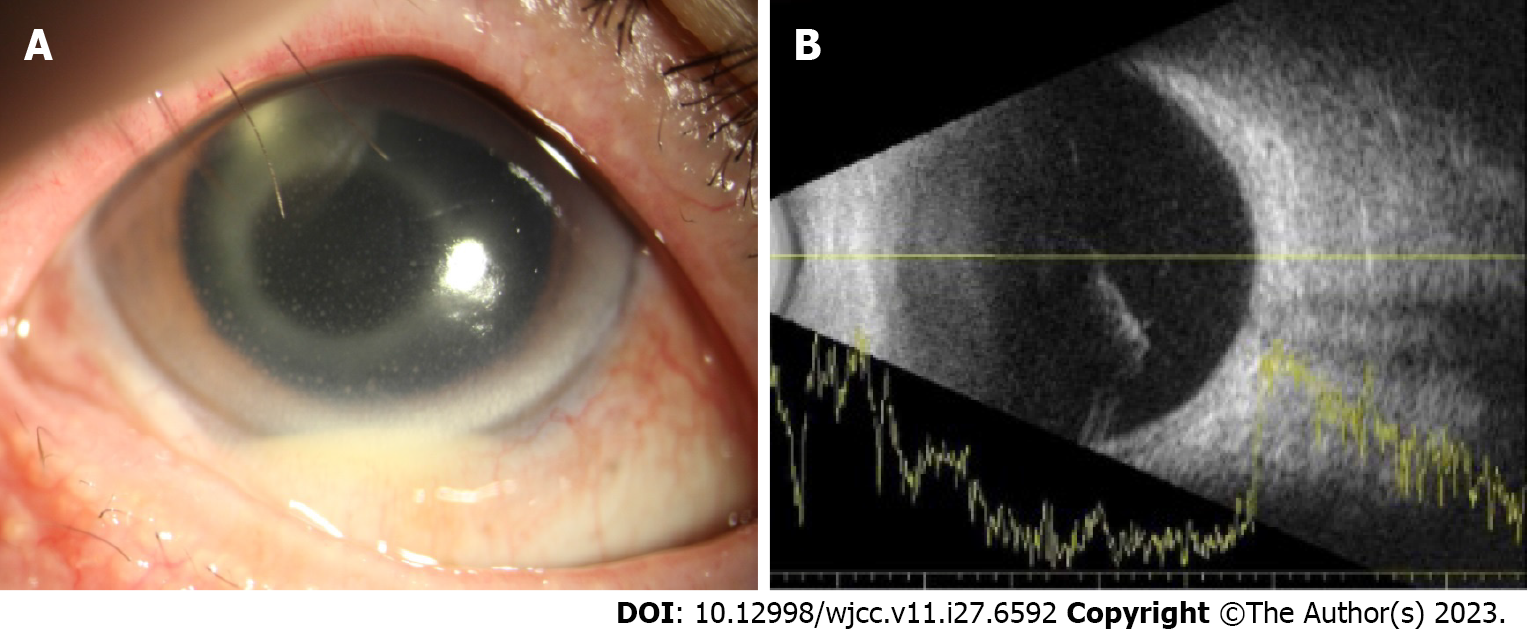
The patient had a visual acuity of counting fingers in the right eye and an intraocular pressure of 11. Slit-lamp examination showed conjunctival injection, corneal endothelial precipitates, anterior chamber cell grade 4+, and hypopyon 1 mm. Fundus examination revealed moderate vitreous opacities (Figure 1). In the left eye, the best-corrected visual acuity (BCVA) was 0.5, and the intraocular pressure was 14. Slit-lamp examination was unremarkable. Fundus examination revealed epiretinal membrane.
There were no special abnormalities.
B-scan ultrasonography showed vitreous opacity.
The patient was suspected of having infectious endophthalmitis.
Because of suspected infectious endophthalmitis, emergency vitrectomy and anterior chamber irrigation were performed. Vitreous and anterior chamber aqueous humor samples were obtained for microbial culture test. Intraoperatively, the vitreous cavity was irrigated with 0.2 mg/mL vancomycin (Hanomycin; Samjin Pharm., Seoul, South Korea) and 0.45 mg/mL ceftazidime (Dimcef; Chong Kun Dang Pharm., Seoul, South Korea); vancomycin (1.0 mg/0.1 mL) and ceftazidime (2.25 mg/0.1 mL) were also injected intravitreally. Because there were no specific abnormal findings in the intraocular lens (IOL) and lens capsule, they were not removed.
Postoperatively, 0.5% moxifloxacin (Vigamox®, Novartis) eye drops were applied at 1-h intervals, and 1% cyclo
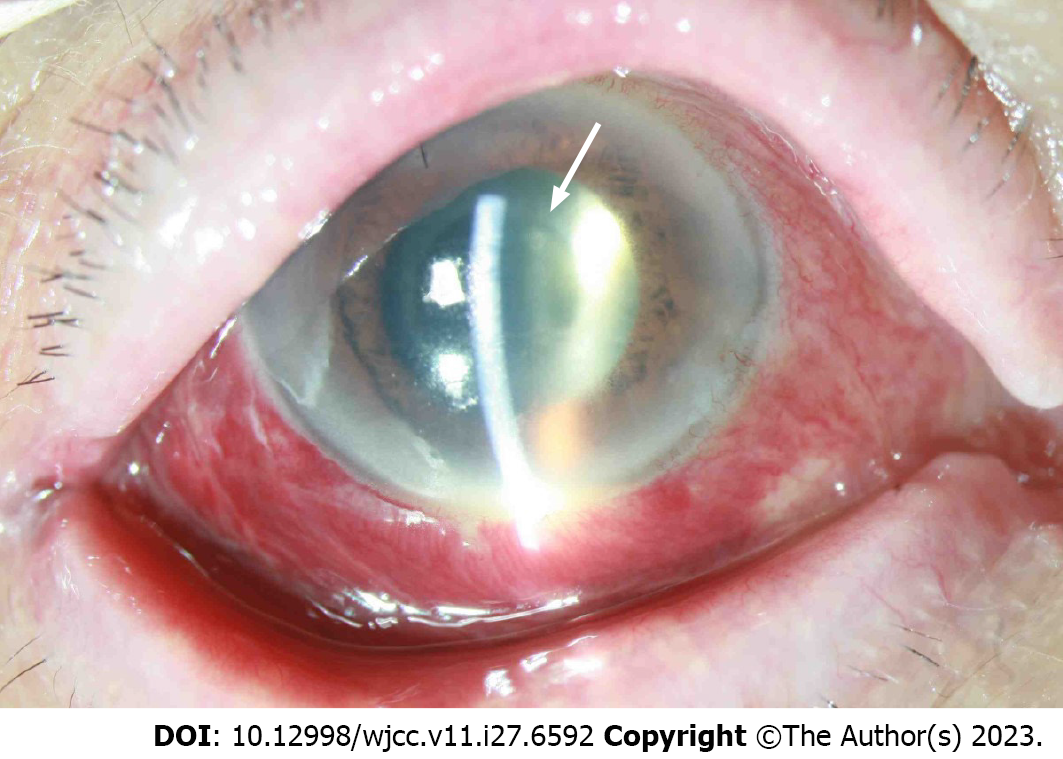
On the first postoperative day, the visual acuity remained counting fingers; however, the anterior chamber cell grade decreased to 2+, the hypopyon disappeared, and the pain improved. No bacteria were grown in the vitreous culture. On the fifth postoperative day, the BCVA was 0.1, but the anterior chamber cell grade increased again; thus, vancomycin (1.0 mg/0.1 mL) and ceftazidime (2.25 mg/0.1 mL) were intravitreally injected. However, on the next day, pain in the right eye recurred, the anterior chamber cell grade increased to 4+, the hypopyon flare reappeared, and a whitish plaque was observed in the posterior capsule of the lens (Figure 2).
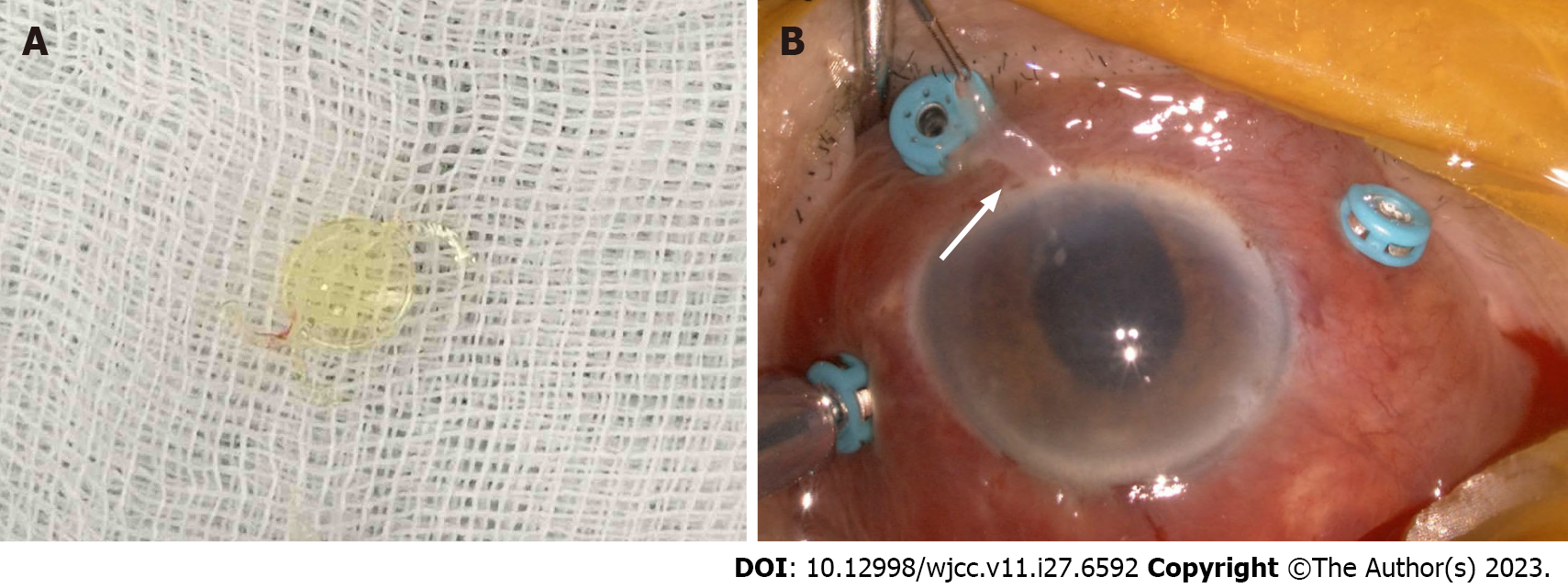
Accordingly, it has been decided to proceed with a reoperation on the sixth postoperative day. The IOL and capsule were removed (Figure 3); intravitreal washout was conducted with vancomycin 0.2 mg/mL and ceftazidime 0.45 mg/mL, as well as intravitreal injection of vancomycin 1.0 mg/0.1 mL and ceftazidime 2.25 mg/0.1 mL. This time, in addition to vitreous and aqueous humor, we also conducted culture tests on the removed IOL and capsular bag. When checking the results of the culture test on the second day after surgery, other samples had negative culture results, but M. luteus was identified in a capsular bag culture. The inflammation gradually subsided, the inflammatory cell grade decreased to a trace, and the BCVA improved to 0.15 at 1 wk after reoperation. The inflammation did not recur. At 4 mo postoperatively, the BCVA was 0.8, and the intraocular pressure was 12 mmHg. No signs of inflammation, such as congestion, anterior chamber cells, or vitreous opacity, were observed; transscleral fixation of the IOL is under consideration.
M. luteus is a Gram-positive, coagulase-negative member of the normal flora of the eyelid and conjunctiva[5]. In a Korean study of bacterial cultures from the conjunctival sacs of normal patients before cataract surgery or intraocular injection,
The present case was regarded as chronic endophthalmitis because it occurred 4 mo after uneventful cataract surgery. Chronic endophthalmitis typically manifests as mild persistent inflammation; in our patient, it manifested as acute endophthalmitis with sudden vision loss, pain, severe anterior inflammation, and hypopyon. It is unclear whether inflammation was present before symptoms began, but the patient reported no specific symptoms before endophthalmitis onset. Fogla et al[5] also described a similar course of M. luteus-induced endophthalmitis after extracapsular cataract extraction. Their patient developed persistent anterior inflammation 4 d postoperatively, which improved with steroid treatment but recurred when the medication was tapered. Seven weeks postoperatively, the patient developed acute endophthalmitis with sudden symptom onset.
Surgical removal of the IOL is recommended as treatment for chronic endophthalmitis. In chronic endophthalmitis, bacterial cells penetrate between the IOL and lens capsule, causing persistent inflammation. Moreover, the endophthalmitis does not recur after IOL removal, implying that such removal is necessary to eliminate the source of infection[8]. In the present case, vitrectomy and intravitreal antibiotics were used as primary treatment, but the IOL was not removed. The inflammation improved after the initial vitrectomy, but it recurred as whitish plaques increased on the IOL and lens capsule. During the second surgery, the IOL and lens capsule were removed; the inflammation improved without recurrence. Although vitreous cultures collected during the first and second surgeries were negative, bacteria grew in the lens capsule culture obtained during the second surgery.
Although the recurrence may be associated with antibiotics resistance, Cartwright et al[7] reported that initial broad-spectrum coverage with cephazolin sodium and gentamicin is adequate in most cases of M. luteus-induced endophthalmitis since M. luteus is highly sensitive. In this case, the recurrence is highly likely to be attributed to microorganisms remaining in the residual IOL and lens capsule after the initial surgery, and inflammation was resolved after removal IOL and the lens capsule during second surgery.
We have described a case of delayed-onset M. luteus-induced endophthalmitis after cataract surgery. M. luteus is a very rare cause of endophthalmitis that can manifest as either persistent and recurrent mild inflammation or acute inflammation with sudden symptom onset even several months after intraocular surgery. Therefore, when endophthalmitis follows such courses, M. luteus should be considered as a potential causative agent. Based on previous reports and the treatment course and culture results in the present case, we recommend considering removal of the intraocular lens and capsule to prevent endophthalmitis recurrence.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Morya AK, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Doft BH. The endophthalmitis vitrectomy study. Arch Ophthalmol. 1991;109:487-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Johnson MW, Doft BH, Kelsey SF, Barza M, Wilson LA, Barr CC, Wisniewski SR. The Endophthalmitis Vitrectomy Study. Relationship between clinical presentation and microbiologic spectrum. Ophthalmology. 1997;104:261-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 111] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Maalouf F, Abdulaal M, Hamam RN. Chronic postoperative endophthalmitis: a review of clinical characteristics, microbiology, treatment strategies, and outcomes. Int J Inflam. 2012;2012:313248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Zambrano W, Flynn HW Jr, Pflugfelder SC, Roussel TJ, Culbertson WW, Holland S, Miller D. Management options for Propionibacterium acnes endophthalmitis. Ophthalmology. 1989;96:1100-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Fogla R, Biswas J, Parikh S, Madhavan HN. Micrococcal endophthalmitis following extracapsular cataract extraction with foldable silicone intraocular lens implantation. Indian J Ophthalmol. 2000;48:50-52. [PubMed] |
| 6. | Kang JY, Lee W, Noh GM, Jeong BH, Park I, Lee SJ. Fluoroquinolone resistance of Staphylococcus epidermidis isolated from healthy conjunctiva and analysis of their mutations in quinolone-resistance determining region. Antimicrob Resist Infect Control. 2020;9:177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Cartwright MJ, King MH, Weinberg RS, Guerry RK. Micrococcus endophthalmitis. Arch Ophthalmol. 1990;108:1523-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Deramo VA, Ting TD. Treatment of Propionibacterium acnes endophthalmitis. Curr Opin Ophthalmol. 2001;12:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |