Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6537
Peer-review started: May 30, 2023
First decision: August 8, 2023
Revised: August 18, 2023
Accepted: August 31, 2023
Article in press: August 31, 2023
Published online: September 26, 2023
Processing time: 113 Days and 3.6 Hours
An intradermal nevus is a common skin tumour, and the classical method of re
We describe two adult patients with eyebrow intradermal nevi treated by shea
Shearing combined with electrocautery and curettage has superior merits, inclu
Core Tip: An intradermal nevus is a common skin tumour. This study aimed to evaluate the efficacy and safety of using shear combined with electrocautery and curettage for removing eyebrow intradermal nevi. In this work, we present two cases of eyebrow intradermal nevi that were treated by shearing combined with electrocautery and curettage and followed up regularly. The results showed no recurrence of the eyebrow intradermal nevus, no obvious scars or hypopigmentation, and high patient satisfaction. The study indicates that shearing combined with electrocautery and curettage is a safe and effective treatment option for intracutaneous nevus removal, presenting great potential for wider application.
- Citation: Liu C, Liang JL, Yu JL, Hu Q, Li CX. Successful treatment of eyebrow intradermal nevi by shearing combined with electrocautery and curettage: Two case reports. World J Clin Cases 2023; 11(27): 6537-6542
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6537.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6537
Melanocytic nevi are common benign skin tumours that arise from the proliferation of melanocytes[1]. According to the position of nevi cells in the skin, melanocytic nevi can be classified into three types: Junctional, compound, and intradermal nevi. Intra
Case 1: A 35-year-old Chinese male presented with a slowly increasing grey-brown papule that had been located on the brow arch for 15 years.
Case 2: A 43-year-old female patient complained of the presence of hemispherical papules that were located on the right eyebrow and had persisted for 30 years.
Case 1: At the age of 17, the patient developed a greyish-brown papule on the left eyebrow arch, with multiple hairs growing above it. The papule gradually increased in size over time. In November 2020, the presence of a hemispherical grey-brown circular tubercle on the left eyebrow arch, measuring 13 mm × 10 mm in size and concomitant with several hairs, was observed.
Case 2: The onset of a small skin papule on the right side of the patient’s brow was observed at the age of 13, and the papule gradually increased in size over time. By May 2019, the papules were hemispheric and measured approximately 8 mm in diameter.
The past medical history was not remarkable for these two patients.
The two patients had no relevant family history of cancer or chronic disease.
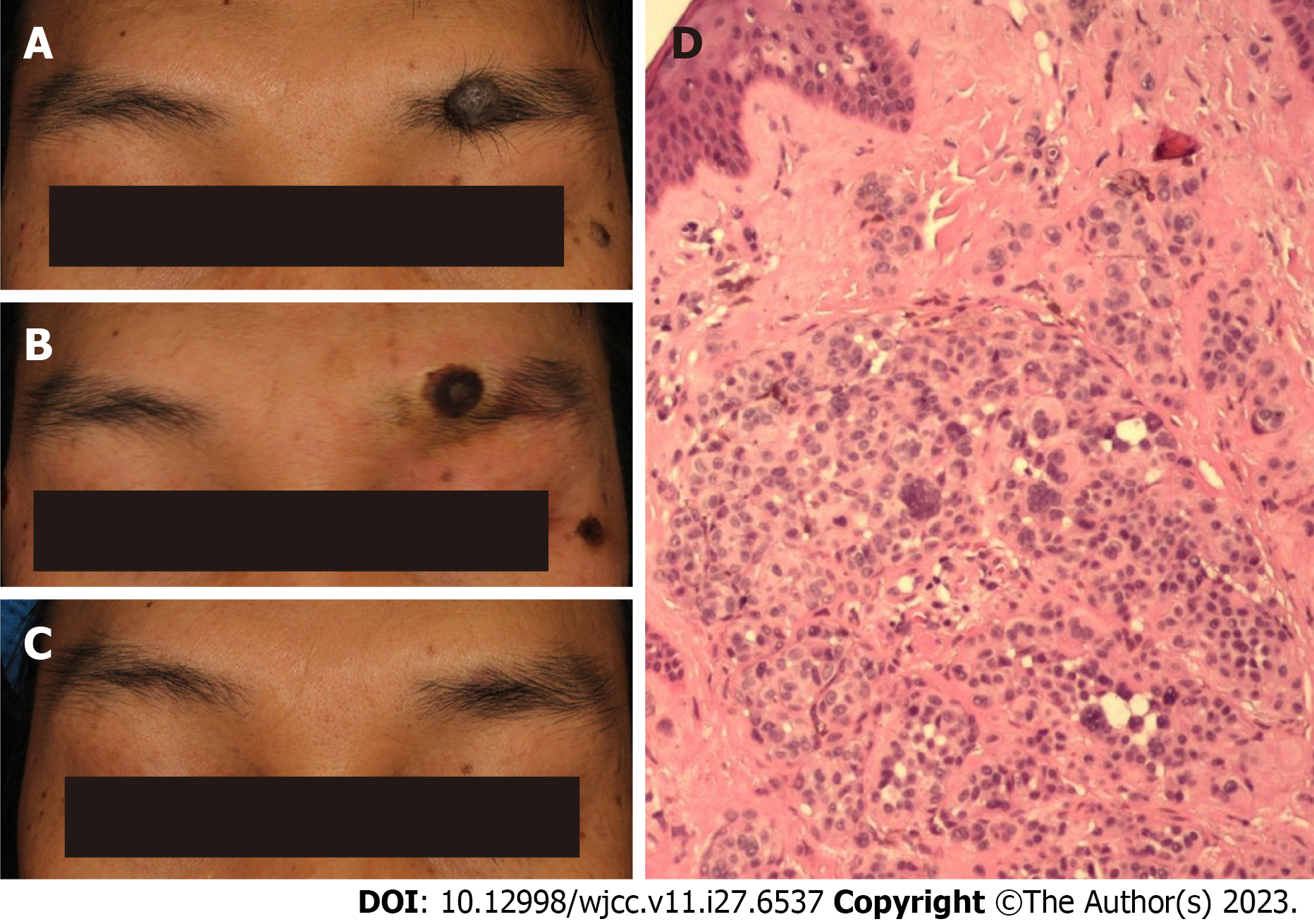
Case 1: Systemic examination revealed no obvious abnormalities. The patient had a hemispherical grey-brown circular nodule on the left eyebrow arch, approximately 13 mm × 10 mm in size, exhibiting the growth of eyebrow hair (Figure 1A).
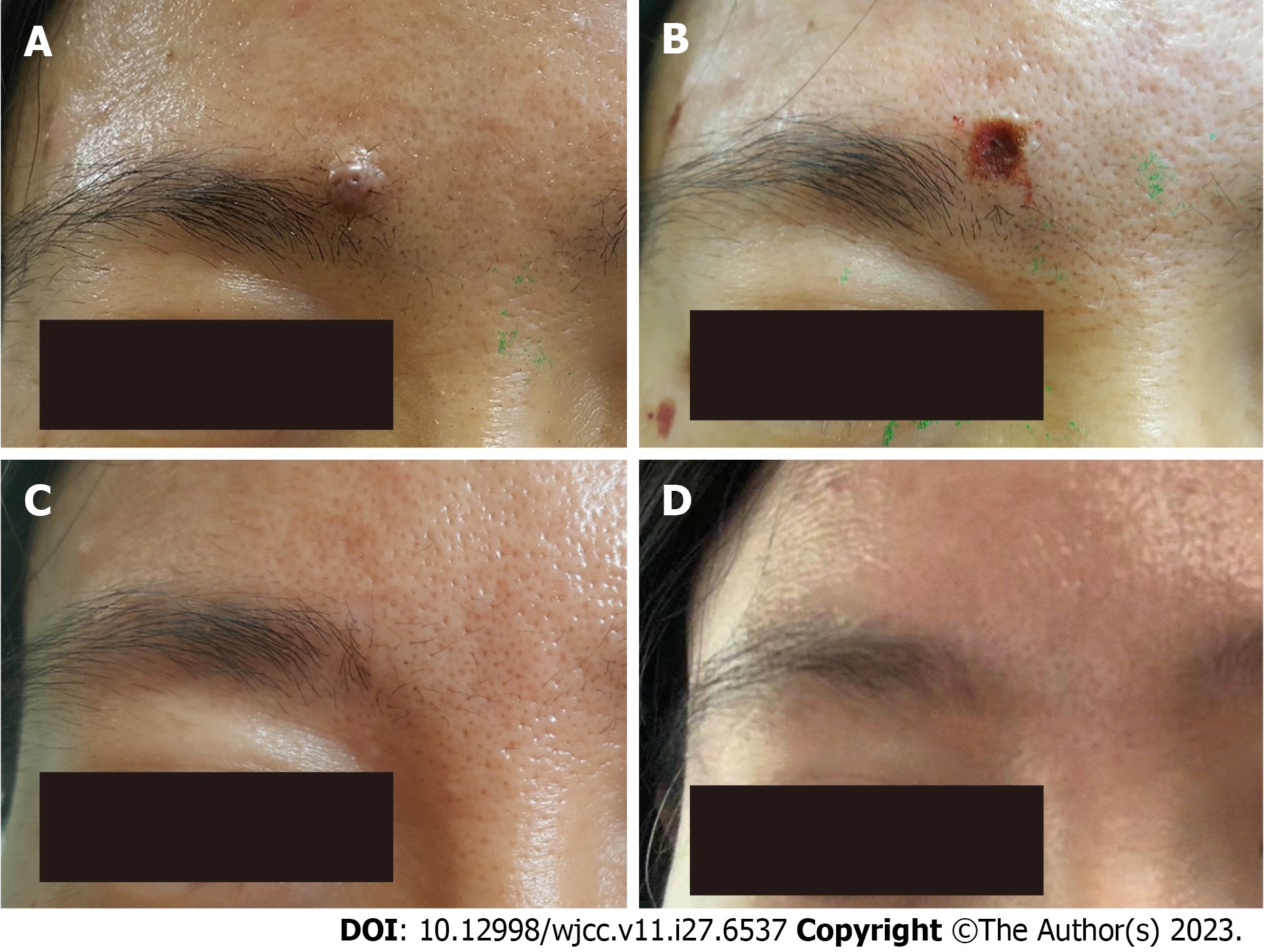
Case 2: Systemic examination revealed no obvious abnormalities. By May 2019, the papules on the patient’s right eyebrow had a hemispherical skin tone with a few black spots and a diameter of approximately 8 mm (Figure 2A).
Laboratory examination of both patients revealed no abnormalities.
These two patients had not undergone an imaging examination.
Intramucosal nevus of the eyebrow.
Both patients underwent shearing combined with electrocautery and curettage. Routine disinfection of the operative field was performed with complex iodine, followed by a local injection of 2% lidocaine to the base of the lesion. The surgeon’s left middle finger and thumb pressed both ends of the intradermal nevus close to the patient’s bone surface, and curved-tip ophthalmic scissors were used to remove the shin mass at the base of the lesion, parallel to the surrounding normal skin. Patient A underwent removal of a skin mass with a diameter of 10 mm, and the excised tissue was biopsied. Patient B had a skin mass with a diameter of 8 mm removed. After shearing, a small amount of blood oozed from the exposed surface, which had a flesh-white surface resembling the residue of the intradermal nevus. The surgeon then used sterile gauze to compress the wound to stop the bleeding. Once the bleeding had stopped, the surgeon used electric cautery microneedles and medium-sized curettes alternately for multiple stratified gasification and curettage to remove residual intradermal nevus lesions. Cotton swabs dampened with 30% ferric chloride tincture were applied to the wound for approximately 30 s to stop the bleeding. Subsequently, a depressed, brown, dry wound formed on the eyebrows of both patients. After the operation, the topical medical healing biofilm (Velvetfeeling) was applied to the wound 3 to 5 times a day for one week. Both patients were followed for more than 1 year to determine their prognosis.
Case 1: Patient A presented a hemispherical grey-brown round nodule with a size of approximately 13 mm × 10 mm that was located on the left brow arch and had several hairs. During the postoperative period and up to the 1-year follow-up, the patient’s wounds gradually crusted and healed. Thirteen months after surgery, there was no hyperpigmentation or depigmentation, no depressed or hyperplastic scars, and normal eyebrow hair growth in the original lesion (Figures 1B and C). The postoperative pathology was consistent with an intradermal nevus (Figure 1D). The patient was very satis
Case 2: Patient B was a 43-year-old female with a hemispherical papule on the right eyebrow for 30 years. After the patient gave informed consent, shearing combined with electrocautery and curettage was performed under local anaesthesia, which took approximately 5 min. Similar to patient A, nearly four years after the operation, the skin of the original lesion was almost indistinguishable from the surrounding normal skin, and no obvious scars were visible (Figures 2B-D).
Intradermal nevus is a type of melanocytic nevus with nevus cell nests located in the dermis. According to Lea and Pawlowski[8-10], intradermal nevi can be defined as epidermal structures surrounded by basement membrane bands located outside the nevus cell nests. At present, there are two popular methods to remove nevus cell nests, including ultrawide surgical resection of nevus cell nests, electrocauterization and use of a CO2/erbium laser. On the one hand, the latter method uses high-temperature gasification to eliminate nevus cell nests[3]. However, it is a challenge for dermatologists to completely remove the mole cells and not cause excessive damage to the surrounding normal tissue. On the other hand, the cosmetic effects of this method vary from person to person, and in some cases, patients might even experience disfigurement. This paper reports two cases of successful treatment of eyebrow intradermal nevi by shearing combined with electrocautery and curettage. Neither of the two patients showed any clear recurrence or scar formations, and such an outcome can further enhance patient satisfaction. This formula is effective in eradicating the lesion and the method requires less equipment, which makes it easier to be widely disseminated.
An interesting phenomenon that seems to contradict the current consensus emerged in the present study. Immediately after surgery, both patients presented obvious depressed wounds, but the depressions became shallower and eventually resembled the surrounding skin, with no obvious remaining depressions. Normal skin dermal tissue contains elastic fibres, which have spring-like properties[11]. Intradermal nevi are epidermal structures located in the dermis, with cell nests surrounded by a basement membrane. During the proliferation of melanocytes, the expanding cell nests exert pressure on the surrounding tissues, causing deformation and shortening of elastic fibres. Within a certain deformation space, if the diseased tissue can be completely removed without harming the surrounding normal tissue, the surrounding connective tissue can fill the space occupied by the diseased tissue due to the retraction of the elastic fibres. The lack of visible scarring observed in the patients after surgery may have been due to the minimal damage to elastic fibres and the subsequent regeneration and backfilling of surrounding connective tissue.
Currently, the optimal therapeutic goal for nonsurgical excision of intradermal nevi is believed to be the complete removal of nevus nests located in the invaginated dermis, along with the surrounding basement membrane, while pre
There are some limitations to this study: (1) This article only reports two cases involving patients who were succe
In summary, the results of two patients who showed no residual disease, no recurrence, and no obvious scars after the procedure corroborate that shearing combined with electrocautery and curettage can produce satisfactory cosmetic results. When using this method to remove the lesion tissue in the dermis of an intradermal nevus, there is no extensive damage of the normal tissue around the lesion, so the patient can achieve satisfactory results of mole removal. However, use of this procedure does not guarantee the complete removal of mole cells, and there is still a risk of scar formation. Nonetheless, the method is simple, efficient, inexpensive, and easy to learn and master. Moreover, the technique can be utilized to treat other benign lesions in specific areas.
In this study, we report the successful removal of intradermal nevi from the eyebrow area of two patients by using shearing combined with electrocautery and curettage. The procedure resulted in the absence of any postoperative re
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Venugopal V, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Hauschild A, Egberts F, Garbe C, Bauer J, Grabbe S, Hamm H, Kerl H, Reusch M, Rompel R, Schlaeger M; expert group "Melanocytic nevi". Melanocytic nevi. J Dtsch Dermatol Ges. 2011;9:723-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Greco V, Cappello M, Megna M, Costa C, Villani A, Fabbrocini G, Marino V, Scalvenzi M. Dermoscopic patterns of intradermal naevi. Australas J Dermatol. 2020;61:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Ibrahimi OA, Alikhan A, Eisen DB. Congenital melanocytic nevi: where are we now? Part II. Treatment options and approach to treatment. J Am Acad Dermatol. 2012;67:515.e1-13; quiz 528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Guida S, Bencini PL, Manganoni AM, Gianotti R, Lospalluti L, Greco P, Pellacani G, Farnetani F. Recurrence of melanocytic lesions after laser treatment: benign vs. malignant upon dermoscopy. J Eur Acad Dermatol Venereol. 2017;31:e526-e528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Camini L, Manzoni APD, Weber MB, Luzzato L, Soares AS, Bonamigo RR. Shave Excision Versus Elliptical Excision of Nonpigmented Intradermal Melanocytic Nevi: Comparative Assessment of Recurrence and Cosmetic Outcomes. Dermatol Surg. 2021;47:e21-e25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Tursen U, Kaya TI, Ikizoglu G. Round excision of small, benign, papular and dome-shaped melanocytic nevi on the face. Int J Dermatol. 2004;43:844-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Fraser L, Smith WK. Excisional technique for intradermal nevi of the external auditory canal. J Otolaryngol Head Neck Surg. 2009;38:501-503. [PubMed] |
| 8. | Lea PJ, Pawlowski A. Human melanocytic naevi. I. Electron microscopy and 3-dimensional computer reconstruction of naevi and basement membrane zone from ultrathin serial sections. Acta Derm Venereol Suppl (Stockh). 1986;127:5-15. [PubMed] |
| 9. | Lea PJ, Pawlowski A. Human melanocytic naevi. II. Depth of dermal protrusion: comparative measurements of the basement membrane zone and diameters of intracellular microfibrils using a microcomputer analysis system. Acta Derm Venereol Suppl (Stockh). 1986;127:17-21. [PubMed] |
| 10. | Lea PJ, Pawlowski A. Human melanocytic naevi. III. Immunofluorescence and immunoelectron microscopy of the basement membrane zone. Acta Derm Venereol Suppl (Stockh). 1986;127:23-30. [PubMed] |
| 11. | Jo H, Brito S, Kwak BM, Park S, Lee MG, Bin BH. Applications of Mesenchymal Stem Cells in Skin Regeneration and Rejuvenation. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 124] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 12. | Anderson RR. Lasers in dermatology--a critical update. J Dermatol. 2000;27:700-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |