Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6424
Peer-review started: June 23, 2023
First decision: August 9, 2023
Revised: August 11, 2023
Accepted: August 29, 2023
Article in press: August 29, 2023
Published online: September 26, 2023
Processing time: 78 Days and 15.7 Hours
Unlike the already established effect of Helicobacter pylori (H. pylori) eradication on gastric mucosa-associated lymphoid tissue (MALT) lymphoma, its therapeutic effect on primary gastric diffuse large B-cell lymphoma (DLBCL) is still unclear.
To clarify the efficacy of H. pylori eradication treatment for primary gastric DLBCL.
We reported on 3 new cases, and added them to 3 previously reported cases. We analyzed the usefulness of H. pylori eradication treatment for gastric DLBCL for a total of 6 cases at our center.
Of the 6 patients (27-90 years old, 3 males and 3 females), all 3 patients with single lesions (one transformed from MALT lymphoma) achieved complete remission (CR) after H. pylori eradication. Regarding the 2 newly reported cases, CR was maintained for more than 6 years with eradication treatment alone. In contrast, none of the 3 patients with 2 lesions achieved CR. In 1 newly reported case, endo
We believe it is worthwhile to attempt H. pylori eradication for elderly patients with primary gastric DLBCL in a single lesion with a small tumor burden.
Core Tip: Unlike the already established effect of Helicobacter pylori (H. pylori) eradication on gastric mucosa-associated lymphoid tissue lymphoma, its therapeutic effect on primary gastric diffuse large B-cell lymphoma (DLBCL) is not clear. Previously, we reported 1 successful case and 2 failed cases. We report here on 3 new cases, and we considered a total of 6 cases. Three patients with a single lesion achieved complete remission, in contrast, 3 patients with multiple lesions persisted or progressed. We believe it is worthwhile to attempt H. pylori eradication for an elderly patient with a single lesion and a small tumor burden of primary gastric DLBCL.
- Citation: Saito M, Mori A, Kajikawa S, Yokoyama E, Kanaya M, Izumiyama K, Morioka M, Kondo T, Tanei ZI, Shimizu A. Helicobacter pylori eradication treatment for primary gastric diffuse large B-cell lymphoma: A single-center analysis. World J Clin Cases 2023; 11(27): 6424-6430
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6424.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6424
There are several reports that explain the effectiveness of eradication treatment for early-stage primary gastric diffuse large B-cell lymphoma (DLBCL), which is positive for Helicobacter pylori (H. pylori), regardless of the presence or absence of the mucosa-associated lymphoid tissue (MALT) lymphoma component[1-5]. However, unlike the already established effect of H. pylori eradication on gastric MALT lymphoma[6,7], its therapeutic effect on primary gastric DLBCL is still unclear. We have placed great importance on the efficacy of this noninvasive treatment, and previously, we reported on 1 successful case (short-term)[8] and 2 failed cases[9]. However, these 3 cases were mainly reported retrospectively. This time, we report on 3 new cases as a prospective study and examine the efficacy of H. pylori eradication for a total of 6 cases of primary gastric DLBCL.
This was an observational study at our center with both prospective and retrospective perspectives.
Previously, we reported 3 cases of primary gastric DLBCL treated with H. pylori eradication between January 2014 and June 2016. One of the patients (case A[8]) was young, 27 years old. She reached complete remission (CR) but was given the established standard treatment, rituximab + cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) chemotherapy × 3 courses, followed by gastric irradiation (40.6 gray). One patient (70 years old, male, case B[9]) appeared to have reached CR in both the pylorus and the antrum region 3 mo after eradication treatment; however, the lesion recurred in another area (the lesser curvature of the lower corpus - ventricular angle) one year after the initial onset. The lesion had spread to the para-inferior vena cava lymph nodes (Lugano-Stage II2). The patient was administered rituximab + cyclophosphamide, pirarubicin, vincristine and prednisone chemotherapy × 6 courses, and CR was maintained for more than 6 years. In another patient (64 years old, female, case C[9]), 2 lesions in the gastric corpus were found to have enlarged (Lugano-Stage I) 8 mo after the initial onset and H. pylori eradication. R-CHOP chemotherapy × 3 courses followed by gastric irradiation (30 gray), and CR has been maintained for more than 6 years.
In this study, we experienced 3 new cases of primary gastric DLBCL with low tumor burden that were treated with H. pylori eradication therapy between July 2016 and February 2021. We prospectively investigated and reported these cases here. In addition, a total of 6 cases, including the 3 cases presented above, were comprehensively examined for the effi
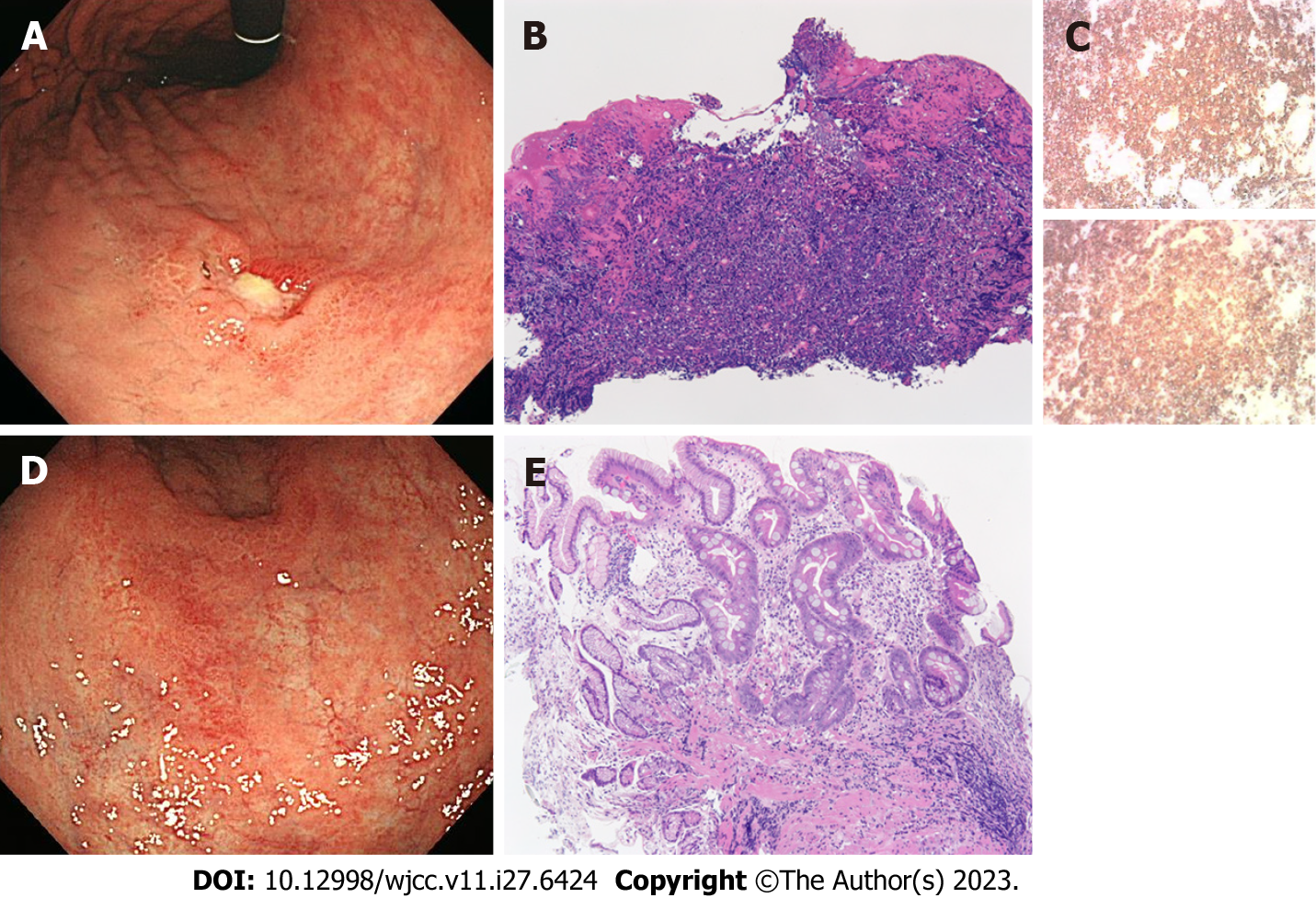
Case 1: A 71-year-old man underwent esophagogastroduodenoscopy (EGD) for screening at a municipal hospital while hospitalized for diabetes. An ulcerative lesion was found in the lesser curvature of the lower corpus of the stomach (Figure 1A), and a pathological diagnosis of DLBCL was made by biopsy (Figures 1B and C). Since H. pylori was positive by urea breath test, eradication treatment was performed at the hospital until the diagnosis was confirmed. Eradication therapy was performed by oral administration of vonoprazan fumarate, amoxicillin hydrate and clarithromycin (20 mg, 750 mg and 200 mg, respectively, twice daily) for one week. Two months later, a re-examination by EGD at our hospital revealed that the ulcerative lesion had already regressed, and no DLBCL findings were found on biopsy (Figures 1D and E). Eradication of H. pylori was confirmed by rapid urease test and histopathology. Computed tomography (CT) and positron emission tomography (PET)-CT did not detect any neoplastic lesions. After that, he was followed-up again at the municipal hospital with no treatment, and he was in CR endoscopically and histopathologically for more than 6 years.
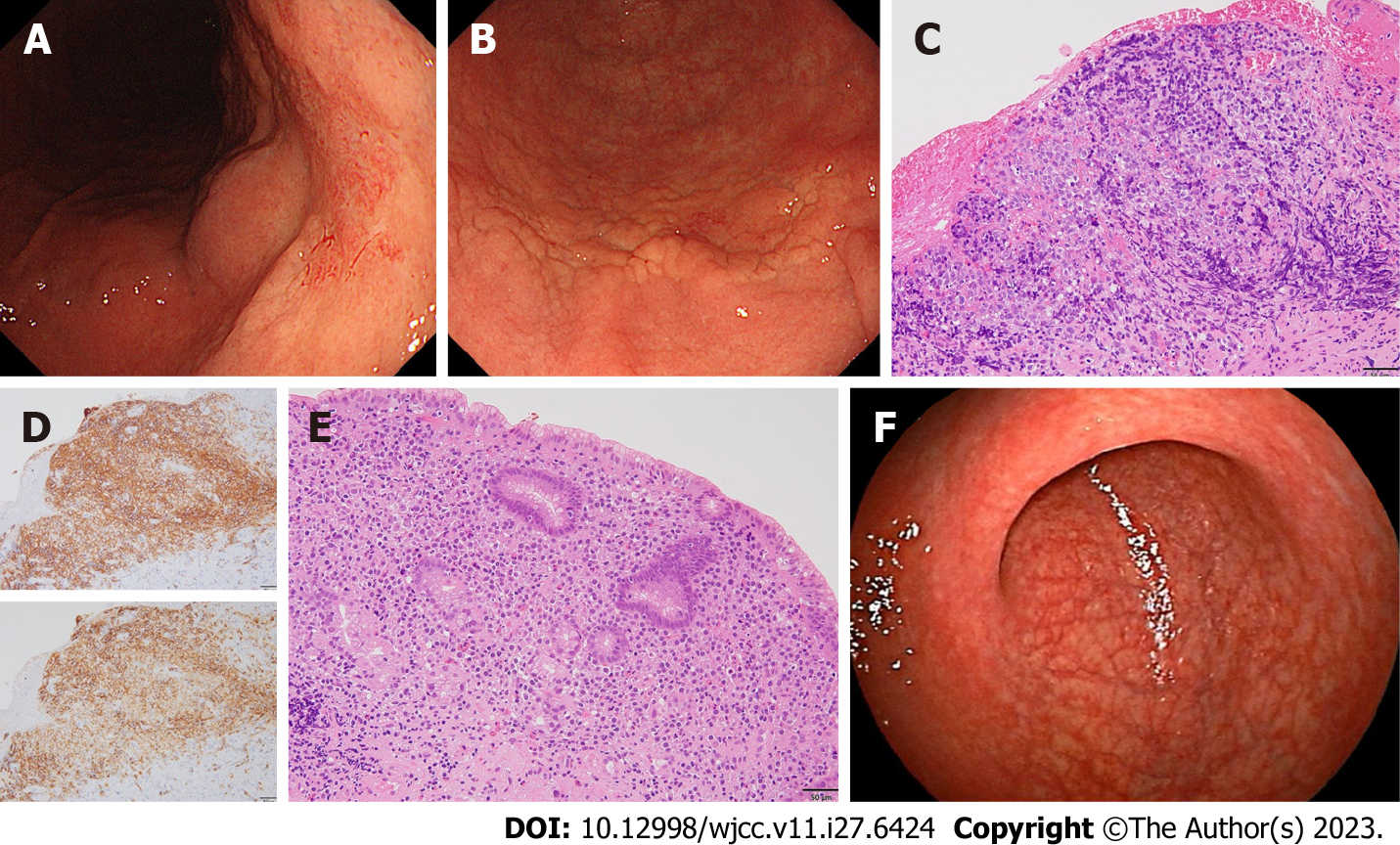
Case 2: A 67-year-old woman seen at a university hospital for immunoglobulin G4-related disease, mainly affected submandibular gland, underwent EGD for screening. A reddish change was observed on the mucosal surface at the posterior wall (Figure 2A), and a raised mucosal change was observed in the corpus of the stomach (Figure 2B). A biopsy was performed for each lesion; the former was pathologically diagnosed as DLBCL (Figures 2C and D) and the latter as MALT lymphoma (Figure 2E). CT and PET-CT did not reveal gastric lesions. The patient was referred to our center. Since H. pylori was positive by rapid urease test and histopathological study, eradication treatment was performed using the same method as case 1. When the patient was re-examined by EGD 3 mo later, the lesions were not clear, and a biopsy was histopathologically negative for H. pylori (rapid urease test was also negative), with no findings of DLBCL or MALT lymphoma (Figure 2F). Since then, CR has been maintained endoscopically and histopathologically for more than 6 years.
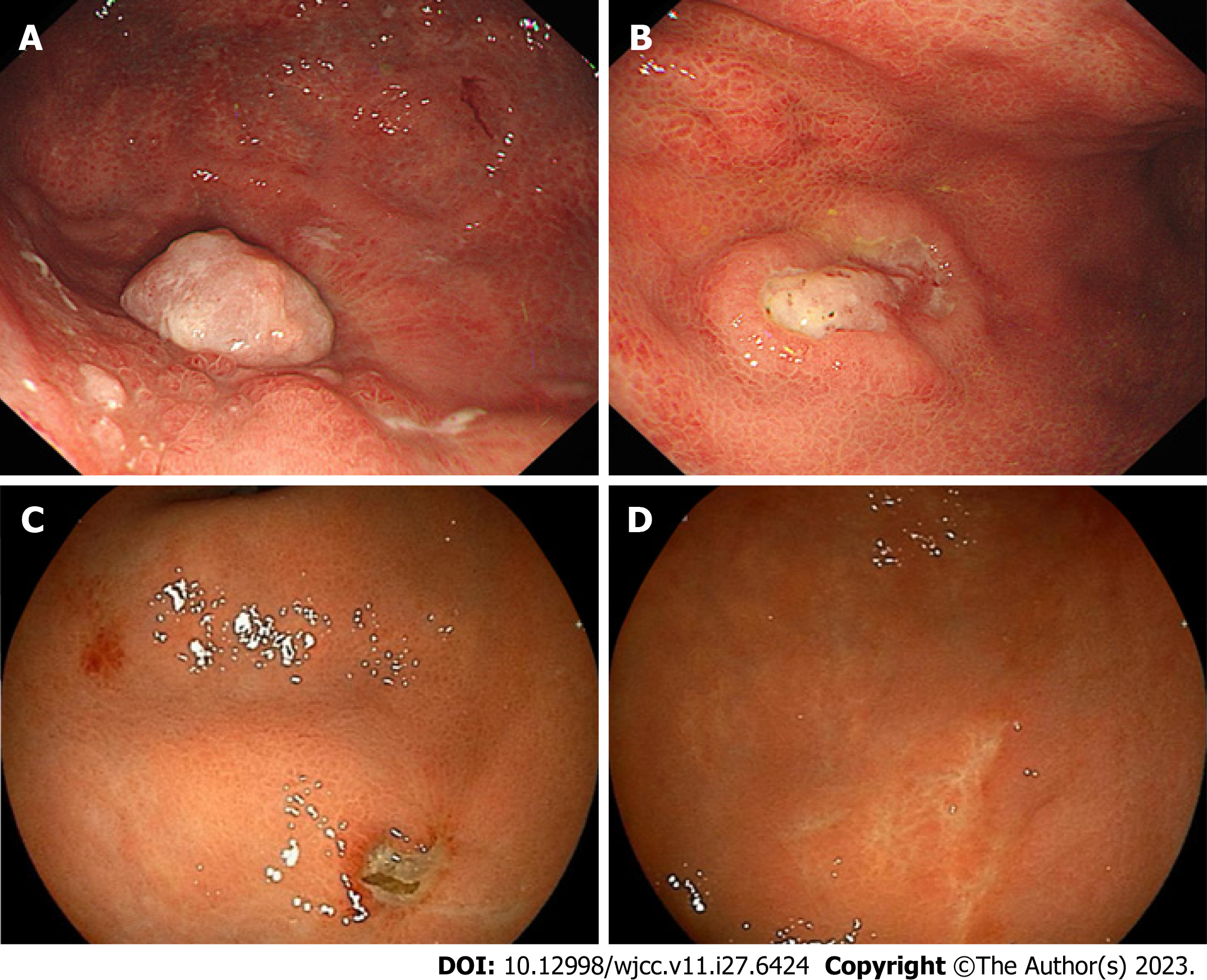
Case 3: A 90-year-old man underwent EGD at a nearby hospital to search for the cause of his fever and was found to have a polypoid elevated lesion (Figure 3A) in the fundus and an ulcerative lesion (Figure 3B) in the greater curvature of the gastric corpus. A biopsy was histopathologically positive for H. pylori and revealed an MIB-1 index of 90% for both lesions. Immunostaining was positive for c-myc, and a pathological diagnosis of non-GCB-type DLBCL was made. PET-CT detected both gastric lesions, which were not apparent on CT. No lesions were found outside the stomach on those images. A screening test detected serum M-protein, it was found that this patient had monoclonal gammopathy of undetermined significance. Eradication treatment for H. pylori was performed at our center using the same method as case 1 and case 2. Since then, fever was no longer observed. Three months later, a fecal H. pylori antigen test was negative, and an EGD was performed again. The elevated lesion at the fundus was ulcerated (Figure 3C), and the ulcerative lesion at the corpus was scarred (Figure 3D). Five months after eradication treatment, CR was able to be maintained endoscopically for the latter lesion, but the former lesion was non-CR. In addition, rituximab (375 mg/m2) was administered once a week for 4 consecutive weeks. As a result, the lesions that had already reached CR were maintained in the CR state; however, the lesions that had been non-CR eventually returned to the original polypoid tumor (stable disease). The patient refused any further treatment. Nearly 2 years have passed since then, and he is still alive with the disease.
Table 1 shows the clinical features of the 6 gastric DLBCL patients (27-90 years old, 3 males and 3 females) who were treated with H. pylori eradication. In all cases, the tumor burden was low endoscopically at the beginning of the diagnosis, and 1 patient (case 2) was found to have coexisting MALT lymphoma, suggesting transformation from MALT lymphoma. Including this patient, CR was achieved in all 3 patients with a single lesion. The patient of case A was treated with anti
| Case | Age | Sex | Number of lesions | Endoscopic morphology | MALT lymphoma component | Comorbidities | Therapeutic effect | Additional treatment | Current condition | Ref. |
| 1 | 71 | Male | 1 | Ulcerative | (-) | Diabetes | CR | (-) | Maintaining CR (≥ 6 yr) | |
| 2 | 67 | Female | 1 | Superficial | (+) | IgG4-related disease | CR | (-) | Maintaining CR (≥ 6 yr) | |
| 3 | 90 | Male | 2 | Ulcerative. Elevated | (-) | MGUS | CR. SD | RTX (1/wk) × 4 wk | Alive with disease (2 yr) | |
| A | 27 | Female | 1 | Ulcerative | (-) | (-) | CR | R-CHOP × 3 courses + gastric irradiation | Maintaining CR (≥ 9 yr) | [8] |
| B | 70 | Male | 2 | Ulcerative (both 2 lesions) | (-) | Diabetes | CR (both lesions). Recurrence (PD) | R-THP-COP × 6 courses | Maintaining CR (≥ 6 yr) | [9] |
| C | 64 | Female | 2 | Ulcerative (both 2 lesions) | (-) | (-) | PD (both lesions) | R-CHOP × 3 courses + gastric irradiation | Maintaining CR (≥ 6 yr) | [9] |
In contrast, all 3 patients with 2 lesions were non-CR after H. pylori eradication treatment. In 1 new patient (case 3), both lesions had an MIB-1 index of 90% and were non-GCB-type DLBCL positive for c-myc. For 1 lesion, CR was obta
Recently, it was reported that the H. pylori infection rate in patients with primary gastric DLBCL was 54.7% (123/225)[10]. Another review reported that the probability of inducing CR in gastric DLBCL with H. pylori eradication alone was 60% (33/55) in MALT-derived DLBCL and 49.3% (40/81) in non-MALT-derived, de novo DLBCL; in addition, the probabilities were 50.7% (40/79) in stage I and 42.8% (6/14) in stage II[11]. Furthermore, the latter paper reported that among the 71 patients who failed to achieve remission with H. pylori eradication, 63 out of 64 patients (98.4%) achieved CR based on treatments including additional anticancer drugs (mainly R-CHOP)[11]. Even if the condition worsened (recurrence/progression) after H. pylori eradication, long-term CR could be maintained by second-line treatment, including chiefly R-CHOP chemotherapy, considering either this review[11] or our 2 successful experiences (case B and case C[9]). It is cur
The efficacy of H. pylori eradication in patients with DLBCL may be related to the depth of tumor invasion. As an indication for H. pylori eradication treatment for primary gastric DLBCL with or without the MALT lymphoma com
It has been reported that in gastric DLBCL, the expression of BCL10, nuclear factor kappaB (p65), cytotoxin-associated gene A (CagA)[13] and CagA-signaling molecules is clinically and biologically H. pylori-dependent[5], or miR-200 was associated with the susceptible group for H. pylori[14]. Although knowledge about B-cell receptor signaling related to susceptibility to H. pylori eradication treatment in gastric DLBCL is advancing[15], clinical application is still difficult. In this study, molecular medical markers were not scrutinized, which was a limitation of our research.
We studied 3 new cases prospectively, which are inherently different from the 3 cases we previously reported as a retrospective study (1 successful case, but short-term observation[8], and 2 failed cases[9]). Of the current 3 patients with 4 lesions, medium- to long-term CR was obtained successfully in 3 lesions with H. pylori eradication alone, and stable disease was obtained in 1 lesion. However, two lesions in case 3 had a MIB-1 index of 90% and a non-GCB-type DLBCL positive for c-myc and had a high degree of biological malignancy. It is significant that CR was obtained even for 1 lesion endoscopically by eradication treatment, and this patient has been alive with the disease for approximately 2 years.
We considered the benefits of H. pylori eradication on gastric DLBCL with a total of 6 cases, including 3 previously reported cases. Three patients with a single lesion achieved CR, in contrast, 3 patients with multiple lesions persisted or progressed. This may be the first report showing that the number of tumors affected the efficacy of H. pylori eradication treatment for primary gastric DLBCL.
In conclusion, especially in elderly individuals, it is worthwhile to try H. pylori eradication treatment first in single pri
The efficacy of Helicobacter pylori (H. pylori) eradication treatment for gastric mucosa-associated lymphoid tissue (MALT) lymphoma has been established.
The therapeutic efficacy of H. pylori eradication treatment for primary gastric diffuse large B-cell lymphoma (DLBCL) remains unclear.
This study aimed to clarify the efficacy of H. pylori eradication for primary gastric DLBCL.
We examined the usefulness of H. pylori eradication treatment for gastric DLBCL in a total of 6 patients at our center, including 3 previously reported cases.
Of the 6 patients (27-90 years old, 3 males and 3 females), all 3 patients with a single lesion achieved complete remission (CR) after H. pylori eradication. Regarding the 2 newly reported patients (one transformed from MALT lymphoma, and the other was de novo), CR was maintained for more than 6 years with eradication treatment alone. In contrast, none of the 3 patients with 2 lesions achieved CR. In 1 newly reported patient, CR was achieved endoscopically in 1 lesion, while stable disease was obtained in the other lesion. Two patients with progressive disease responded to standard chemo
It is considered worthwhile to try H. pylori eradication first for elderly patients with a single primary gastric DLBCL lesion, which has a low tumor burden.
The number of relevant cases is still small, and it is necessary to further increase the number of patients and continue the examination.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng H, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Kuo SH, Yeh KH, Wu MS, Lin CW, Hsu PN, Wang HP, Chen LT, Cheng AL. Helicobacter pylori eradication therapy is effective in the treatment of early-stage H pylori-positive gastric diffuse large B-cell lymphomas. Blood. 2012;119:4838-44; quiz 5057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Ferreri AJ, Govi S, Raderer M, Mulè A, Andriani A, Caracciolo D, Devizzi L, Ilariucci F, Luminari S, Viale E, Müllauer L, Dell'Oro S, Arcidiacono PG, Ponzoni M, Patti C. Helicobacter pylori eradication as exclusive treatment for limited-stage gastric diffuse large B-cell lymphoma: results of a multicenter phase 2 trial. Blood. 2012;120:3858-3860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Ferreri AJ, Govi S, Ponzoni M. The role of Helicobacter pylori eradication in the treatment of diffuse large B-cell and marginal zone lymphomas of the stomach. Curr Opin Oncol. 2013;25:470-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Paydas S. Helicobacter pylori eradication in gastric diffuse large B cell lymphoma. World J Gastroenterol. 2015;21:3773-3776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Kuo SH, Chen LT, Lin CW, Yeh KH, Shun CT, Tzeng YS, Liou JM, Wu MS, Hsu PN, Cheng AL. Expressions of the CagA protein and CagA-signaling molecules predict Helicobacter pylori dependence of early-stage gastric DLBCL. Blood. 2017;129:188-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Nakamura S, Sugiyama T, Matsumoto T, Iijima K, Ono S, Tajika M, Tari A, Kitadai Y, Matsumoto H, Nagaya T, Kamoshida T, Watanabe N, Chiba T, Origasa H, Asaka M; JAPAN GAST Study Group. Long-term clinical outcome of gastric MALT lymphoma after eradication of Helicobacter pylori: a multicentre cohort follow-up study of 420 patients in Japan. Gut. 2012;61:507-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (1)] |
| 7. | Cook JR, Isaacson PG, Chott A, Nakamura S, Müller-Hermelink HK, Harris NL. Swerdlow SH. Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. WHO classification of tumours of haematopietic and lymphoid tissues. Revised 4th ed. Lyon, France: IARC press, 2017: 259-262. |
| 8. | Saito M, Masutani M, Mabe K, Izumiyama K, Mori A, Irie T, Tanaka M, Morioka M, Tanino M. Regression of gastric de novo diffuse large B-cell lymphoma following Helicobacter pylori eradication: a case report. Acta Gastroenterol Belg. 2016;79:367-369. [PubMed] |
| 9. | Saito M, Mori A, Ogasawara R, Izumiyama K, Morioka M, Kondo T, Miyashita K. Progression of Primary Gastric Diffuse Large B-Cell Lymphoma after Helicobacter pylori Eradication. Case Rep Gastroenterol. 2020;14:534-539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Feng Y, Duan TJ, Huang Q, Li ZY, Liu YP, Luo MS, Lu GF, Shi W, Zhang ZY, Li HX. The clinicopathological characteristics of gastric cancer and precancerous conditions in gastric DLBCL and MALT lymphoma patients: a multi-center retrospective study. Ann Med. 2023;55:2193423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 11. | De Francesco V, Manta R, Marmo R, Marmo C, Rago A, Antonelli G, Hassan C, Zullo A. Efficacy of Helicobater pylori eradication in patients with diffuse large B-cell lymphoma of the stomach: A systematic review. Eur J Haematol. 2022;109:643-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Tari A, Asaoku H, Kashiwado K, Yoshino T, Kitadai Y, Tanaka S, Fujihara M. Predictive value of endoscopy and endoscopic ultrasonography for regression of gastric diffuse large B-cell lymphomas after Helicobacter pylori eradication. Dig Endosc. 2009;21:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Tsai HJ, Tai JJ, Chen LT, Wu MS, Yeh KH, Lin CW, Wang TE, Wang HP, Yu FJ, Liou JM, Hsiao CF, Cheng TY, Yeh HJ, Ko CW, Chen MJ, Lo GH, Hsu PI, Chang CS, Hwang WS, Chuang SS, Lee HW, Shun CT, Chiu CF, Wang WM, Hsieh CY, Liu TW, Lin JT, Kuo SH, Cheng AL; Taiwan Cooperative Oncology Group. A multicenter prospective study of first-line antibiotic therapy for early-stage gastric mucosa-associated lymphoid tissue lymphoma and diffuse large B-cell lymphoma with histological evidence of mucosa-associated lymphoid tissue. Haematologica. 2020;105:e349-e354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Huang WT, Kuo SH, Kuo YC, Lin CW. miR-155-regulated mTOR and Toll-like receptor 5 in gastric diffuse large B-cell lymphoma. Cancer Med. 2022;11:555-570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 15. | Torisu T, Kawano S, Miyawaki K, Yamamoto H, Ihara Y, Matsuno Y, Torisu K, Sugio T, Sasaki K, Shimakawa T, Kato K, Akashi K, Nakamura S, Kitazono T. B cell receptor signaling related to resistance to Helicobacter pylori eradication therapy in gastric diffuse large B cell lymphoma. Hematol Oncol. 2021;39:145-147. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |