Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6374
Peer-review started: June 6, 2023
First decision: July 17, 2023
Revised: July 28, 2023
Accepted: August 23, 2023
Article in press: August 23, 2023
Published online: September 26, 2023
Processing time: 106 Days and 11.3 Hours
The nasal bone, being the most protruding bone in the center of the facial bones, is particularly susceptible to damage. Nasal bone fractures can often result in secondary deformation and dysfunction of the nose, including septal fractures. Studies on functional or intra-nasal complications have been rarely reported after nasal bone fracture reduction.
To evaluate the severity of nasal obstruction and its improvement following nasal bone fracture reduction using inferior turbinoplasty.
We conducted a retrospective review of data from 50 patients with symptomatic nasal obstruction between January to December 2010. All patients underwent preoperative Computed tomography evaluation, and symptom changes and nasal cavity volume were analyzed using a visual analog scale and acoustic rhinometry before and after surgery. Closed reduction and out-fracture of both inferior turbinates performed by the same surgeon. Treatment outcomes were assessed by comparing changes in the nasal airway volume measured using acoustic rhinometry before and after surgery. The minimal cross-sectional area (MCA) was also analyzed based on the Stranc classification.
Before reduction, the mean MCA for all cases was 0.59 ± 0.06 cm2, which represented an 11% decrease compared to the average size of a Korean adult (0.65 ± 0.03 cm2). The MCA for frontal impact was 0.60 ± 0.02 cm2 and for lateral impact, it was 0.58 ± 0.03 cm2. After reduction via inferior turbinoplasty, the MCA improved to 0.64 ± 0.04 cm2.
This study suggests that turbinoplasty is helpful in addressing nasal obstruction. Out-fracture of the inferior turbinate is an effective and durable technique that can be easily performed to enlarge the nasal airway with minimal morbidity.
Core Tip: We analyzed subjective symptoms and computed tomography images of patients with nasal bone fractures before and after surgery. Acoustic nasal aeration was examined before and after surgery to determine the effect of the inferior turbinate anatomy on nose function through cross-sectional changes. We reviewed the data of 50 patients with symptomatic nasal obstruction. Treatment outcomes were evaluated by comparing changes in nasal airway volume measured using acoustic rhinometry before surgery. The minimal cross-sectional area was improved up to 0.64 ± 0.04 cm2 after reduction with inferior turbinoplasty. Our results suggest that out-fracture of the inferior turbinate is an effective and durable technique that can be easily performed to enlarge the nasal airway with minimal morbidity.
- Citation: Kim SY, Nam HJ, Byeon JY, Choi HJ. Effectiveness of out-fracture of the inferior turbinate with reduction nasal bone fracture. World J Clin Cases 2023; 11(27): 6374-6382
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6374.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6374
Among facial bones, the nasal bone is located at the center of the facial bones. The nasal bone, being the most protruding bone in the center of the facial bones, is particularly susceptible to damage. Nasal bone fractures can often result in secondary deformation and dysfunction of the nose, including septal fractures[1,2]. However, current practices have had little consideration towards anatomical structures such as the nasal cavities, which often involve airway obstruction and olfactory disturbances due to fractures or efforts to objectify patient's subjective or temporary symptoms[3]. Although a study by Kim et al[4], has previously evaluated the degree of improvement in intranasal airway obstruction in nasal bone fractures using acoustic nasal airway examination, limitations exist, as the study neglects the possible complications, solely focusing on the presence of obstruction and the degree of improvement after non-invasive reduction surgery. Although the closed reduction of nasal bone fracture is a relatively simple technique, patient satisfaction after operation remains inadequate, as exhibited in patients’ complaints in the appearance and functional problems such as olfactory disorders and nasal obstruction[5-7]. The site directly involved in the dynamic of intranasal ventilation, which is often responsible for functional problems of the nose, is known as the nasal valve or inferior turbinate front section[8-10]. In the field of otolaryngology, inferior turbinate outward osteotomy and septal curvature have mainly been performed to address functional problems of the nose. However, studies involving such structures have been rare in the field of plastic surgery[11-16].
Therefore, our study investigated the effect of the anatomical structure of the inferior turbinate on the function of the nose in nasal bone fractures through the changes of the nasal cavity, determined by subjects’ pre- and post-operative symptoms, computed tomography (CT) analysis, and pre- and post-operative acoustic nasal airway examination. The results of this study, in conjunction with a literature review, indicate satisfactory improvements in both subjective and objective measures of nasal appearance and function following inferior turbinate outward osteotomy and concurrent closed reduction in patients with nasal bone fractures.
From January to December 2010, pre-operative radiological examination and acoustic rhinometry were performed on nasal bone fracture patients with nasal obstruction symptoms prior to receiving closed reduction. CT was performed in all patients before surgery, and acoustic rhinometry was performed before and 14 d after surgery. In addition, questionnaires on the patients’ symptoms were conducted before surgery, and two weeks, four weeks, and eight weeks after surgery. To determine the level of improvement in nasal obstruction after surgery, patients were asked to evaluate their symptoms on a visual analog scale (VAS) of 0 to 10, where 0 indicated no symptoms of nasal obstruction and 10 indicated a state of complete nasal obstruction. The VAS is a psychometric measurement instrument widely used in the field of rhinology and other fields to subjectively quantify patient symptom severity[17].
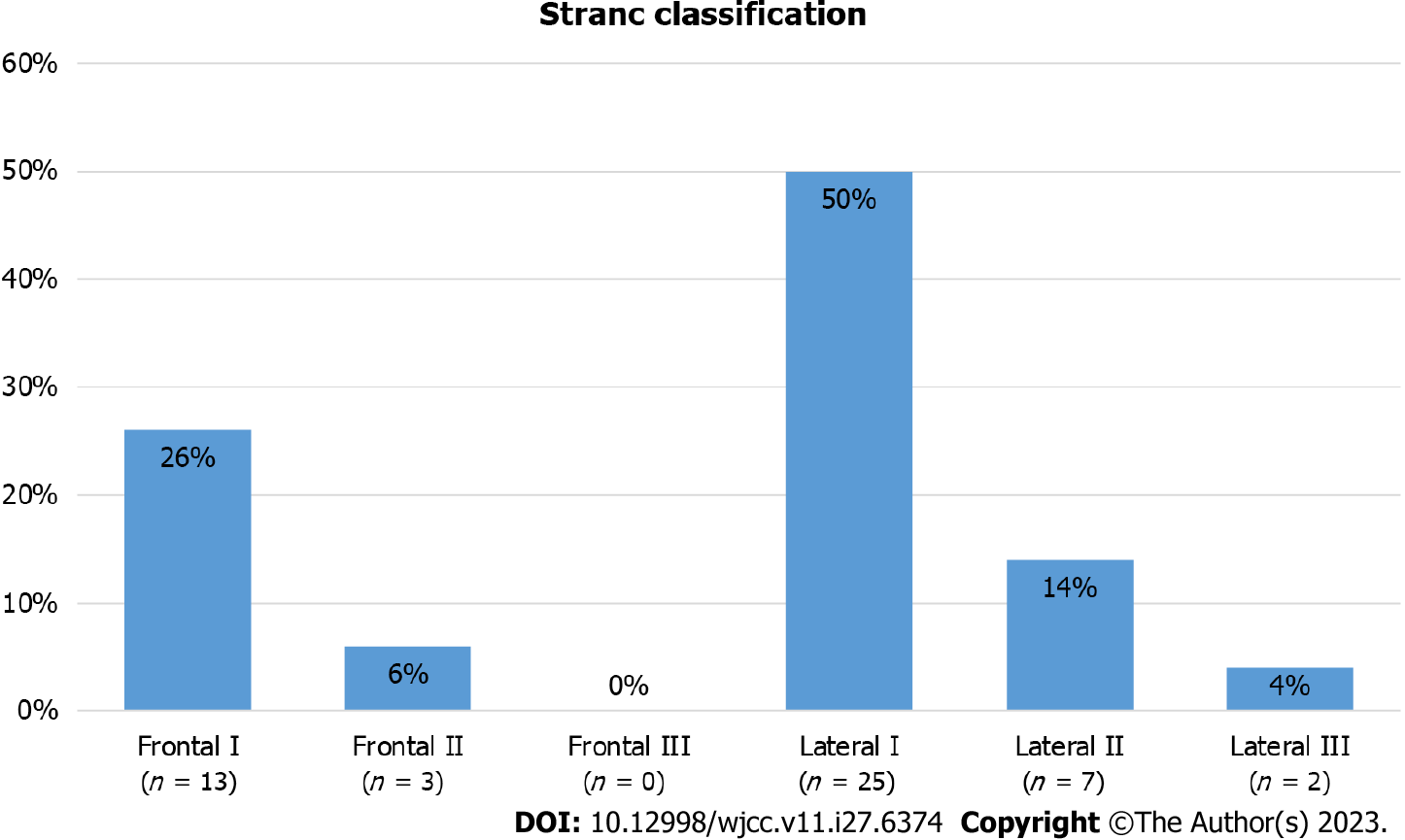
Nasal bone fractures were classified according to the Stranc classification system using CT performed for diagnosis. The Stranc classification simultaneously reflects the direction of impact and the degree of damage, enabling a comprehensive and practical classification of nasal bone fractures, and consideration of the direction of impact[6]. The fractures were categorized as frontal impact and lateral impact, and later subdivided into type 1, type 2, and type 3. The degree of nasal obstruction was later evaluated according to the type of nasal bone fracture.
Nasal obstruction was objectively measured using an acoustic rhinometry (Eccovision Acoustic Rhinometer, Model AR-1003 Hood Laboratories, Pembroke, MA, United States). The test was performed by the same operator, and epinephrine was used administrated in the nasal cavity before the test to reduce bias in the variability of patients’ nasal mucosa.
The acoustic air permeability test was conducted three times for each patient, and the average minimal cross-sectional area (MCA) of each nasal passage was determined based on the three trials. The degree of nasal obstruction of the control group was determined by the average minimum cross-sectional value in Korean adults, which is 0.68cm2[2].
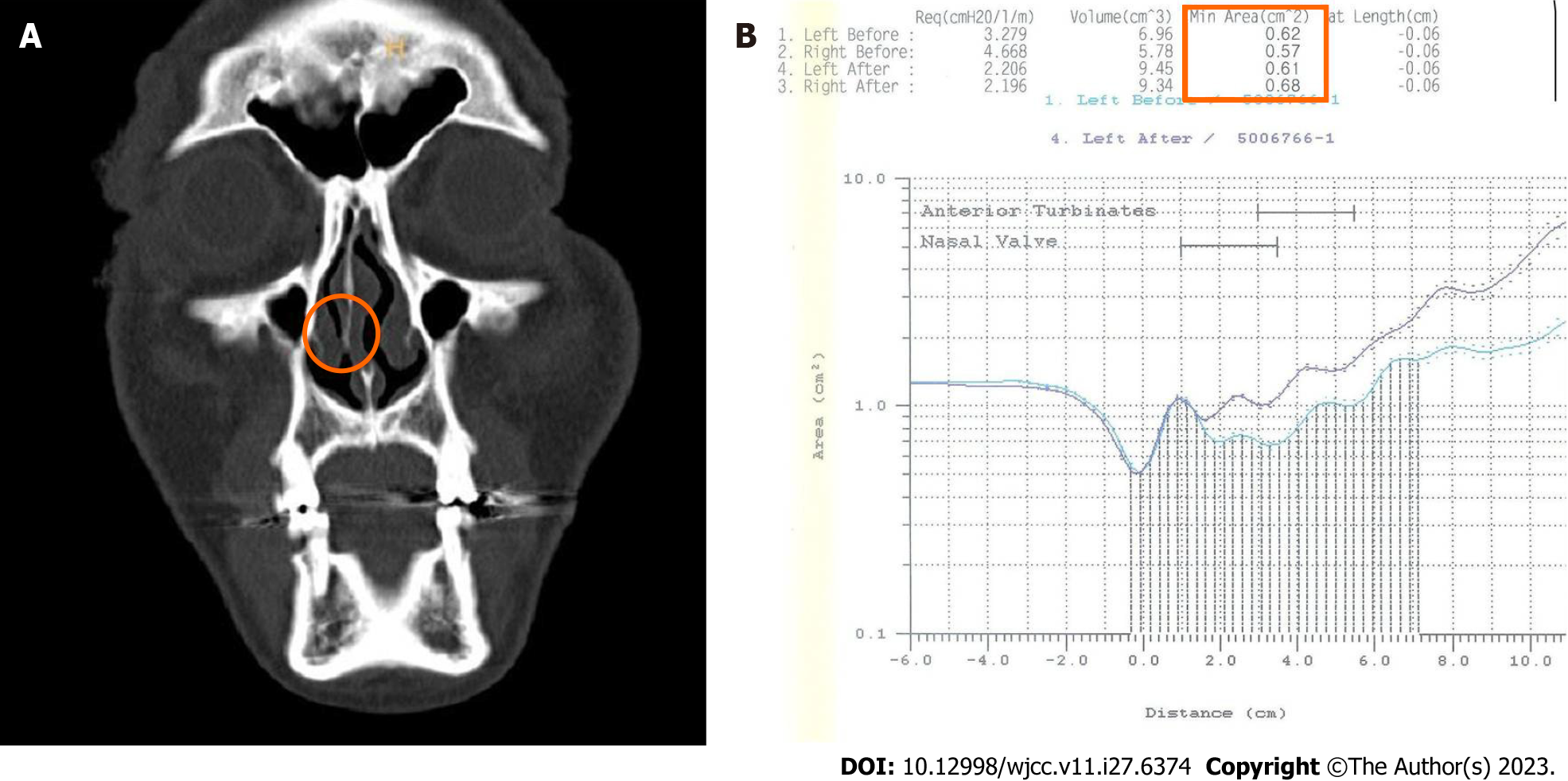
Surgery was performed within 14 d after injury in all patients under general anesthesia. After the nasal cavity was filled with cotton balls soaked with epinephrine(bosmin®) and Proparacaine Hydrochloride(alcaine®) more than five minutes, closed reduction was performed. An outward osteotomy of the inferior turbinate followed, selectively on areas of narrowed nasal cavity of the inferior turbinate, according to the pre-operative CT analyses, due to the accompanying damage to the septum or due to thickening of the inferior turbinate (Figure 1). For out-fracture of the inferior turbinate, a long and wide- bladed nasal speculum was positioned on and carefully widened the inferior turbinate, while applying pressure to the septum[8] (Figures 2 and 3).
Each measurement value was expressed as mean ± SD. SPSS (Statistical Product and Serviced Solutions, version 11.0; SPSS Inc., Chicago, IL, United States) was utilized for statistical analysis, and comparative analysis was performed using the paired t-test. The significance level was set to 0.05 or less.
A total of 50 patients, 43 males and seven females, were included, ranging in age from 21 to 53 years old (Table 1, mean ± SD: 27.7 ± 18.9 years). Among the 50 nasal bone fracture patients with nasal obstruction symptoms, 48 exhibited improvement in nasal obstruction symptoms within eight weeks after surgery. When the patients were classified into a frontal impact group and a lateral impact group, 14 of the 16 patients in the frontal impact group exhibited improvement in symptoms within two weeks, and the remaining two patients showed improvement within four weeks. Of the 34 patients in the lateral impact group, 26 showed improvement in symptoms within two weeks, and six of the remaining eight showed improvement within four weeks; however, in two patients, symptoms continued even after eight weeks (Figure 4). Symptom scores decreased in all 16 patients within four weeks after surgery in the frontal impact group and in 32 patients within eight weeks in the lateral impact group. In the frontal impact group, the symptom score, which was 5.2 ± 1.52 before surgery, decreased to 1.8 ± 1.01 at two weeks after surgery and improved to 0.8±0.76 at four weeks. In the side impact group, the score was 7.1 ± 0.82 before surgery, later decreasing to 3.5 ± 1.02 after two weeks and improving up to 1.89 ± 1.1 at four weeks. Both groups showed a statistically significant improvement in symptom scores two weeks after surgery compared with the scores before surgery (P < 0.05). On acoustic rhinometry performed in patients with nasal obstruction, the minimum cross-sectional area of all patients before surgery was 0.59 ± 0.06 cm2, resulting in an 11% reduction compared to the average value of 0.65 ± 0.03 cm2 in Korean adults. After surgery, the minimum cross-sectional area was measured as 0.67 ± 0.02 cm2, which represents a 13% increase compared to the value prior to surgery (P < 0.05).
| Characteristics | Value |
| Sex, n (%) | |
| Male | 43 (86.0) |
| Female | 7 (14.0) |
| Age | 27.7 ± 18.9 |
| Main causes of nasal bone fracture, n (%) | |
| Direct trauma | 14 (28.0) |
| Human trouble | 6 (12.0) |
| Slip of fall down | 11 (22.0) |
| Traffic accident | 15 (30.0) |
| Others | 4 (8.0) |
| Total | 50 |
The patients were categorized based on the location of the fracture using the Stranc classification system: There were 13 patients in the frontal impact group type 1, three patients in the frontal impact group type 2, 25 patients in the lateral impact group type 1, seven patients in the lateral impact group type 2, and two patients in the lateral impact group type 3 (Figure 5). The mean preoperative minimum cross-sectional area in the frontal impact group was 0.60 ± 0.02 cm2, and the mean value of the lateral impact group was 0.58 ± 0.03 cm2. After non-invasive reduction and outward osteotomy, the nasal cavity was expanded to 0.66 ± 0.04 cm2 in the frontal impact group, and 0.68 ± 0.02 cm2 in the side impact group, exhibiting a more notable increase in the side impact group (Figure 6 and Table 2).
| Mean value from minimal cross-sectional area (cm2) | |||
| Preoperative | Postoperative | Change (P value) | |
| Total (n = 50) | 0.59 ± 0.06 | 0.67 ± 0.03 | < 0.05 |
| Frontal impact (n = 16) | 0.60 ± 0.02 | 0.66 ± 0.04 | < 0.05 |
| Lateral impact (n = 34) | 0.58 ± 0.03 | 0.68 ± 0.02 | < 0.05 |
The nose plays a significant role as an organ in breathing, and the turbinate inside the nose is the area where the highest air resistance occurs[18]. The turbinate is consisted of a thin, semicircular cartilage, and a highly vascular mucosal periosteum that controls the humidity inside the nose and the mucus covering the cilia[19]. In particular, the inferior turbinate, the structure positioned most anteriorly, occupies the largest area among the three turbinates and plays the most crucial role in the symptoms of nasal obstruction[20]. The enlarged mucous membrane increases air resistance in the nose, causing nasal obstruction. A method that can objectively determine nasal obstruction is acoustic rhinometry that measures airway resistance in the nasal cavity. Acoustic rhinometry is an airway test that measures various airway resistances and is a method commonly used to measure nasal obstruction in Rhinology[21-23]. Using the sound wave from the spark generator, the reflected wave generated by the difference in the cross-sectional area of the space, in which the sound wave travels, is collected by a microphone, calculated by a computer, and displayed in a distance-area graph. In this acoustic rhinometry test, two notches appear on the normal distance-cross-sectional area curve. According to Lenders et al[24], the first isthmus notch (I-notch), which corresponds to the nasal isthmus, is located 1.3 cm from the anterior nostril, and has a cross-sectional area of 0.73 cm2. The second notch, which corresponds to the anterior end of the inferior turbinate, is located 3.3 cm from the anterior nostril, and has a cross-sectional area of 1.1 cm2[24]. The most meaningful value in the acoustic rhinometry is the minimum cross-sectional area, which has the greatest airway resistance. Since this test has a possibility of bias, a representative graph is selected among several test values. However, it is one of the most widely used tests in clinical practice; thanks to its non-invasiveness, simplicity, facility and sensitivity, it can measure the volume of the nasal cavity multiple times[25,26]. In order to reduce bias, one inspector measured the test error, and the minimum cross-sectional area value with the greatest effect on nasal occlusion was the only value measured among various variables. The average values of the minimum cross-sectional area before and after surgery were utilized. Symptom relief was assessed using a VAS. The VAS comprises a 10 cm horizontal line with word anchors at each extremity representing the range of extreme feelings. The patients were instructed to mark the point on the line that best corresponded to their current status concerning the specific characteristics under evaluation. Owing to its high sensitivity, reliability, and reproducibility, the VAS is straightforward for patients and healthcare providers. Because it does not require training, the VAS serves as an invaluable tool not only for routine clinical practice but also for real-world studies[27]. As demonstrated in the symptom questionnaires using VAS administered before and after surgery, it was confirmed that the cross-sectional areas increased as the symptoms improved.
In addition, the nasal obstruction symptoms were analyzed according to the type of nasal bone fracture using the Stranc classification method. The Stranc classification method offers an all-encompassing and pragmatic approach to categorizing nasal bone fractures, considering both the direction of impact and extent of injury concurrently. By factoring in the direction of impact, it is possible to predict specific classifications based on the cause. In addition, this method assesses the value of each subgroup depending on the severity of damage. This approach generates valuable insights for devising treatment principles and yields objective data for anticipating and clarifying treatment prognoses[28]. The frequency in the side impact group was 68% (34 cases), which was higher than that in the frontal impact group, which was 32% (16 cases). This is consistent with the results of the study by Daw and Lewis[29], which also showed high frequency in the side impact group. In this study, the side impact group showed a greater degree of nasal obstruction than that in the frontal impact group, as confirmed by the reduction of the minimum cross-sectional area and questionnaire. It is thought that the lateral impact group affected the damage to the nasal septum and the mucosa, thereby reducing the minimum cross-sectional area. Kim et al[4] reported that 80% of patients with nasal bone fractures with nasal septal displacement complained of subjective nasal obstruction symptoms, and that 20% of patients still had occlusion symptoms after surgery. Park et al[28] also reported that nasal septal curvature was the most common complication in patients with nasal bone fractures, and that nasal obstruction was affected by not only nasal bone fractures, but also nasal septum and mucosal damage.
Inferior turbinate surgery widens the nasal airway to facilitate breathing, which is essential to prevent complications such as bleeding, irreversible nasal dryness, crust formation, and bad odor following surgery[30,31]. Outward osteotomy performed on the nasal bone is a minimally invasive method and does not affect the function of intranasal mucinous cilia. In a previous study, Kim et al[4] reported that the intranasal airway improved after a simple nasal bone fracture reduction operation, but the direction of the fracture and septal damage were not evaluated. While another study by Kim et al[32] suggested that the occurrence of nasal obstruction decreases after correction of the nasal septum, but did not explain the difficulty in performing the operation due to edema or complications such as nasal obstruction without damage of the septum. In this study, narrowed areas of the nasal cavity of the inferior turbinate were identified in patients with nasal bone fracture using preoperative CT. After reduction surgery, the inferior turbinate outward osteotomy was performed on the narrowed side. It was evident that the nasal obstruction was improved by the outward osteotomy of the inferior turbinate.
This study has limitations in that it was not possible to discriminate congenital septal curvature due to the lack of data prior to fracture in each individual patient. However, in patients with nasal bone fractures, the degree of nasal obstruction was determined objectively by a numerical value using acoustic rhinometry. In addition, through the classification of nasal bone fractures by the Stranc method, it was confirmed that nasal obstruction was more likely to occur in the lateral impact group. Therefore, in nasal bone fractures accompanied by nasal obstruction and classified as lateral impact on CT, inferior turbinate outward osteotomy can be performed with an easy and few complications. With such procedure, complications of nasal obstruction after nasal bone fracture can be reduced. Another limitation of this study is the relatively short follow-up period of 8 wk, compared to the typical follow-up duration after reduction of nasal bone fracture is usually set at 12 wk. However, our study successfully demonstrated statistically significant improvements in nasal obstruction symptoms within the 8-week follow-up timeframe, confirming the efficacy of inferior turbinate outward osteotomy in alleviating nasal obstruction.
Although non-invasive reduction of the nasal bone fracture may be useful in resolving symptoms of nasal obstruction, our study proved that a simple and easy inferior turbinate outward osteotomy is more advantageous in improving the symptoms of nasal obstruction at an early stage. Also, according to the classification of fracture sites, the occlusion pattern caused by the lateral impact group was relatively more severe than that of the frontal septum group. Moreover, the incidence of nasal septal displacement was high in the lateral impact group, which may lead to persistent symptoms of nasal obstruction.
In conclusion, inferior turbinate outward osteotomy at an early stage helps to increase patient satisfaction after surgery.
Among facial bones, the nasal bone is located at the center of the facial bones. It is the most protruding and thus, the weakest bone. It has a high frequency of damage, which often leads to secondary deformation, as well as dysfunction of the nose due to fracture and dislocation of the septum. The current practices have had little consideration towards anatomical structures such as the nasal cavities, which often involve airway obstruction and olfactory disturbances due to fractures or efforts to objectify patient's subjective or temporary symptoms.
In order to improve functional problems, inferior turbinate outward osteotomy and septal curvature have been mainly performed in the field of otolaryngology, while studies involving such structures have been rare in the field of plastic surgery. Therefore, our study investigated the effect of the anatomical structure of the inferior turbinate on the function of the nose in nasal bone fractures through the changes of the nasal cavity, determined by subjects’ pre- and post-operative symptoms, computed tomography (CT) analysis, and pre- and postoperative acoustic nasal airway examination.
The article demonstrates a satisfactory result in the appearance and function of the nose, subjective and objective, after inferior turbinate outward osteotomy and a concurrent closed reduction in patients with nasal bone fractures.
From January to December 2010, pre-operative radiological examination and acoustic rhinometry were performed on nasal bone fracture patients with nasal obstruction symptoms prior to receiving closed reduction. Questionnaires on the patients’ symptoms were conducted before surgery, and two weeks, four weeks, and eight weeks after surgery. Nasal bone fractures were classified according to the Stranc classification system using CT performed for diagnosis and nasal obstruction was objectively measured using an acoustic rhinometry. Closed reduction and out-fracture of both inferior turbinates performed by the same surgeon. Treatment outcomes were assessed by comparing changes in the nasal airway volume measured using acoustic rhinometry before and after surgery. The minimal cross-sectional area (MCA) was also analyzed based on the fracture classification.
The mean MCA for all cases before reduction was 0.59 ± 0.06 cm2, which was a 11% decrease compared to that in the average of a Korean adult (0.65 ± 0.03 cm2). The MCA were 0.60 ± 0.02 cm2 for frontal impact, and 0.58 ± 0.03 cm2 for lateral impact. The MCA improved up to 0.64 ± 0.04 cm2 after reduction with inferior turbinoplasty.
The results of this study suggest that out-fracture of the inferior turbinoplasty is more helpful to prove nasal obstruction.
Our study proved that a simple and easy inferior turbinate outward osteotomy is more advantageous in improving the symptoms of nasal obstruction at an early stage. Out-fracture of the inferior turbinate is an effective and durable technique, which can be performed easily to enlarge the nasal airway with minimal morbidity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lin L, China; Liu L, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Mondin V, Rinaldo A, Ferlito A. Management of nasal bone fractures. Am J Otolaryngol. 2005;26:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Rohrich RJ, Adams WP Jr. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106:266-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 156] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Choi HJ, Lee YS, Choi CY, Tark MS. A clinical study of nasal synechiae causing by closed reduction for nasal bone fractures. J Korean Soc Plast Reconstr Surg. 2009;36:188-193. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Kim SB, Han SK, Kim WK. Airway improvement after reduction of nasal bone fracture. J Korean Soc Plast Reconstr Surg. 2005;32:49-54. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Harrison DH. Nasal injuries: their pathogenesis and treatment. Br J Plast Surg. 1979;32:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Kim SW, Park B, Lee TG, Kim JY. Olfactory Dysfunction in Nasal Bone Fracture. Arch Craniofac Surg. 2017;18:92-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Hwang K, Yeom SH, Hwang SH. Complications of Nasal Bone Fractures. J Craniofac Surg. 2017;28:803-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Haight JS, Cole P. The site and function of the nasal valve. Laryngoscope. 1983;93:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 210] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Bridger GP. Physiology of the nasal valve. Arch Otolaryngol. 1970;92:543-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 127] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Kasperbauer JL, Kern EB. Nasal valve physiology. Implications in nasal surgery. Otolaryngol Clin North Am. 1987;20:699-719. [PubMed] |
| 11. | Thomas PL, John DG, Carlin WV. The effect of inferior turbinate outfracture on nasal resistance to airflow in vasomotor rhinitis assessed by rhinomanometry. J Laryngol Otol. 1988;102:144-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Aksoy F, Yıldırım YS, Veyseller B, Ozturan O, Demirhan H. Midterm outcomes of outfracture of the inferior turbinate. Otolaryngol Head Neck Surg. 2010;143:579-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 13. | Buyuklu F, Cakmak O, Hizal E, Donmez FY. Outfracture of the Inferior Turbinate: A Computed Tomography Study. Plast Reconstr Surg. 2009;123:1704-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ketcham AS, Han JK. Complications and management of septoplasty. Otolaryngol Clin North Am. 2010;43:897-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Dinis PB, Haider H. Septoplasty: long-term evaluation of results. Am J Otolaryngol. 2002;23:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 108] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Fuat B, Ozcan C, Evren H, Fuldem YD. Out fracture of the inferior turbinate: A Computed tomography study. Plast Reconstr Surg. 2009;123:1704-1709. [RCA] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Doulaptsi M, Prokopakis E, Seys S, Pugin B, Steelant B, Hellings P. Visual analogue scale for sino-nasal symptoms severity correlates with sino-nasal outcome test 22: paving the way for a simple outcome tool of CRS burden. Clin Transl Allergy. 2018;8:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 18. | Leong SC, Eccles R. Inferior turbinate surgery and nasal airflow: evidence-based management. Curr Opin Otolaryngol Head Neck Surg. 2010;18:54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Rohrich RJ, Krueger JK, Adams WP Jr, Marple BF. Rationale for submucous resection of hypertrophied inferior turbinates in rhinoplasty: an evolution. Plast Reconstr Surg. 2001;108:536-44; discussion 545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Chen XB, Leong SC, Lee HP, Chong VF, Wang DY. Aerodynamic effects of inferior turbinate surgery on nasal airflow--a computational fluid dynamics model. Rhinology. 2010;48:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Roithmann R, Cole P, Chapnik J, Shpirer I, Hoffstein V, Zamel N. Acoustic rhinometry in the evaluation of nasal obstruction. Laryngoscope. 1995;105:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 107] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Lal D, Corey JP. Acoustic rhinometry and its uses in rhinology and diagnosis of nasal obstruction. Facial Plast Surg Clin North Am. 2004;12:397-405, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Reber M, Rahm F, Monnier P. The role of acoustic rhinometry in the pre- and postoperative evaluation of surgery for nasal obstruction. Rhinology. 1998;36:184-187. [PubMed] |
| 24. | Lenders H, Pirsig W. Diagnostic value of acoustic rhinometry: patients with allergic and vasomotor rhinitis compared with normal controls. Rhinology. 1990;28:5-16. [PubMed] |
| 25. | Djupesland P, Pedersen OF. Acoustic rhinometry in infants and children. Rhinol Suppl. 2000;16:52-58. [PubMed] |
| 26. | Fisher EW, Scadding GK, Lund VJ. The role of acoustic rhinometry in studying the nasal cycle. Rhinology. 1993;31:57-61. [PubMed] |
| 27. | Klimek L, Bergmann KC, Biedermann T, Bousquet J, Hellings P, Jung K, Merk H, Olze H, Schlenter W, Stock P, Ring J, Wagenmann M, Wehrmann W, Mösges R, Pfaar O. Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care: Position Paper of the German Society of Allergology (AeDA) and the German Society of Allergy and Clinical Immunology (DGAKI), ENT Section, in collaboration with the working group on Clinical Immunology, Allergology and Environmental Medicine of the German Society of Otorhinolaryngology, Head and Neck Surgery (DGHNOKHC). Allergo J Int. 2017;26:16-24. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 175] [Cited by in RCA: 275] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 28. | Park WY, Kim YH. A clinical study of the nasal bone fracture according to Stranc classification. J Korean Soc Plast Reconstr Surg. 2008;35:289-294. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Daw JL, Lewis VL. Lateral force compared with frontal impact nasal fractures: need for reoperation. J Craniomaxillofac Trauma. 1995;1:50-55. [PubMed] |
| 30. | Bhandarkar ND, Smith TL. Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 2010;18:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 31. | Joshi RR, Riley CA, Kacker A. Complication Rates Following Septoplasty With Inferior Turbinate Reduction. Ochsner J. 2019;19:353-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Kim JH, Shin DW, Choi TH, Son DG, Han KH. The importance of septoplasty in the treatment of nasal bone and grade I septal fracture: Estimation with acoustic rhinometry. J Korean Soc Plast Reconstr Surg. 2010;37:626-632. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |