Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6363
Peer-review started: April 9, 2023
First decision: June 15, 2023
Revised: July 18, 2023
Accepted: August 21, 2023
Article in press: August 21, 2023
Published online: September 26, 2023
Processing time: 164 Days and 0.9 Hours
Severe proximal humerus comminuted fractures are often accompanied by medial calcar comminuted fractures and loss of medial support, which are important factors that lead to internal fixation failure. The appropriate treatment for proximal humerus comminuted fractures has not been established. Therefore, this study assessed the outcomes of using a fibular autograft with locking plates to treat severe proximal humerus comminuted fractures.
To investigate the outcomes of using a fibular autograft with locking plates to treat severe proximal humerus comminuted fractures.
This retrospective, comparative cohort study included two groups of patients. Group 1 comprised 22 patients and group 2 comprised 25 patients with complete follow-up data. Group 1 was treated with a fibular autograft with open reduction and locking plates to enable internal fixation. Group 2 was treated with open reduction and locking plates to enable internal fixation. The intraoperative blood loss volume from the shoulder wound, operative time, shoulder wound pain, bone fracture healing time, Constant-Murley score of the shoulder joint, preoperative Holden walking function score, Mallet score of the shoulder joint, and humeral neck-shaft angle during surgery of the two groups were compared, and the differences were analysed using an independent sample t-test.
Group 1 had a shorter mean operative time than group 2 (2.25 ± 0.30 h vs 2.76 ± 0.44 h; P = 0.000). Group 1 had a lower shoulder wound pain score on the first day after surgery than group 2 (7.91 ± 1.15 points vs 8.56 ± 1.00 points; P = 0.044). Group 1 had a shorter fracture healing time than group 2 (2.68 ± 0.48 mo vs 3.64 ± 0.64 mo; P = 0.000). Group 1 had higher Constant-Murley scores of the shoulder joint at 3, 6, and 12 mo after surgery than group 2 (76.64 ± 4.02 points vs 72.72 ± 3.02 points, 86.36 ± 3.53 points vs 82.96 ± 3.40 points, and 87.95 ± 2.77 points vs 84.68 ± 2.63 points, respectively; P = 0.000, 0.002, and 0.000, respectively). Group 1 had higher Mallet scores of the shoulder joint at 3, 6, and 12 mo after surgery than group 2 (10.32 ± 0.57 points vs 9.96 ± 0.54 points, 13.36 ± 1.00 points vs 12.60 ± 0.87 points, and 13.91 ± 0.75 points vs 13.36 ± 0.70 points, respectively; P = 0.032, 0.007, and 0.013, respectively).
Using locking plates with a fibular autograft can recreate medial support, facilitate fracture healing, and improve shoulder function; therefore, this may be an effective treatment option for severe proximal humerus comminuted fractures.
Core Tip: Fibula autograft for the treatment of severely comminuted proximal humeral fractures can reconstruct the medial support of the proximal humerus and increase the strength of fixation just like the combination of the extramedullary and intramedullary fixation. We took autogenous fibula segments for the treatment of severe comminuted proximal humeral fractures, and achieved satisfactory results. This is a pioneer treatment for increasing stability because the operation is easy and the cost is low. This study also for the first time applied fibula autograft to the treatment of proximal humeral fractures.
- Citation: Liu N, Wang BG, Zhang LF. Treatment of proximal humeral fractures accompanied by medial calcar fractures using fibular autografts: A retrospective, comparative cohort study. World J Clin Cases 2023; 11(27): 6363-6373
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6363.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6363
Proximal humeral fractures are the third most common fractures among elderly individuals with osteoporosis, accounting for approximately 26% of all humeral fractures[1]. Proximal humeral fractures are likely to occur during high-energy or low-energy trauma, such as falling from a standing height, among patients older than 50 years of age. Good reduction and stable fixation are difficult to achieve with severe proximal humeral comminuted fractures, and this difficulty results in negative effects on the normal rehabilitation of patients and leads to the loss of shoulder function[2]. In 1970, Neer proposed a four-part classification for proximal humeral fractures that is the most commonly used tool for classifying proximal humeral fractures in clinical settings[3]. Most physicians prefer open reduction and internal fixation for Neer type III and type IV fractures with severe comminution. Most internal fixation materials are proximal humeral locking plates or proximal humeral intramedullary nails[4]. According to recent studies, locking plates are widely used and recommended for the treatment of limb fractures. Furthermore, locking plate fixation is the most widely used technique for the treatment of proximal humeral fractures. However, 30% of reoperations are attributable to fixation failure, avascular necrosis of the humeral head, and postoperative infections. These complications are caused by the lack of appropriate medial column structural support[5,6]. Medial calcar comminuted fractures are often accompanied by the loss of medial support, which is an important factor that leads to internal fixation failure. However, appropriate treatment for comminuted fractures has not been identified[7].
The autogenous fibula is a source of bone grafts for the treatment of bone defects. Its advantages include easy access, absence of immune rejection, and considerable strength. However, its disadvantages include the requirement of an additional surgical incision, postoperative pain in the harvested bone area, and the risks of bleeding, infection, and nerve injury. Using structural bone grafts comprising autogenous fibula for the treatment of severe proximal humeral comminuted fractures can re-establish medial support of the proximal humerus and increase fixation strength[8]. Fibular allograft and artificial shoulder joint replacement are also effective treatments for proximal humerus comminuted fractures among elderly individuals[8]. However, these procedures cannot be performed in all regions. Compared to the aforementioned treatments, the use of the autologous fibular segment is more convenient and less expensive. We hypothesised that a fibular autograft could increase the fixation strength of severe proximal humeral comminuted fractures by rebuilding medial support and achieve better treatment outcomes. Therefore, we evaluated relevant studies conducted since 2018 to confirm the efficacy of a fibular autograft combined with open reduction and internal fixation with locking plates for the treatment of proximal humerus comminuted fractures in elderly individuals.
The inclusion criteria were as follows: Severe comminuted fracture of the proximal humerus accompanied by a comminuted fracture of the medial calcar classified as Neer type III or type IV; fracture that occurred within 3 wk; and age older than 60 years.
The exclusion criteria were as follows: Clear surgical contraindications, infection in the surgical area, or severe medical diseases; shoulder joint disease, such as periarthritis of the shoulder, and rotator cuff injury; and incomplete follow-up data or follow-up time less than 1 year.
This was a retrospective, comparative cohort study. From January 2018 to December 2020, among the patients with proximal humeral fractures who required hospitalisation, we selected the following based on the inclusion criteria: Elderly patients; those with a Neer type III or type IV fracture; those with osteoporosis and medial calcar comminution fractures; and those with loss of medial support. These 52 patients were divided into two groups according to whether a fibular autograft was used. The surgical methods and risks were explained to the patients. Group 1 comprised 22 patients who were treated with open reduction and locking plate fixation using a fibular autograft and underwent complete follow-up. Group 2 comprised 25 patients who were treated with open reduction and locking plate fixation and underwent complete follow-up. Group 2 was not treated with a fibular autograft. Five patients were lost to follow-up. Of the patients in group 1, 16 had a right proximal humerus fracture, 6 had a left proximal humerus fracture, 16 were female, 6 were male, 8 had hypertension, 3 had diabetes, and 5 had a cerebral infarction. The mean age of the patients was 65.86 years (SD, ± 7.00 years). The patients were also classified according to fracture type. Twelve and ten patients had Neer type III and type IV fractures, respectively. The mean height was 163.09 cm (SD, ± 7.83 cm), and the mean body weight was 63.55 kg (SD, ± 10.87 kg). Four patients smoked and four consumed alcohol. Fourteen patients experienced a walking injury, one experienced a collision involving an electric bicycle and tricycle, six experienced trauma caused by cycling, and one experienced a collision with an electric bicycle while walking. The mean hospital stay was 14.14 d (SD, ± 3.03 d). The average preoperative time was 5.45 d (SD, ± 1.60 d). The mean follow-up time was 20.45 mo (SD, ± 2.46 mo).
Of the patients in group 2, 16 had a right proximal humerus fracture, 9 had a left proximal humerus fracture, 17 were female, 8 were male, 8 had hypertension, 5 had diabetes, and 4 had a cerebral infarction. The mean patient age was 64.80 years (SD, ± 4.66 years). These patients were also classified according to fracture type. Fifteen and ten patients had Neer type III and type IV fractures, respectively. The mean height was 164.60 cm (SD, ± 6.83 cm), and the mean body weight was 64.36 kg (SD, ± 6.93 kg). Six patients smoked and five consumed alcohol. Seventeen patients experienced a walking injury, one experienced a collision involving an electric bicycle and a bicycle, four experienced trauma caused by cycling, and three experienced a collision with an electric bicycle while walking. The mean hospital stay was 14.16 d (SD, ± 3.00 d). The mean preoperative time was 6.08 d (SD, ± 1.73 d). The mean follow-up time was 20.72 mo (SD, ± 2.23 mo). There were no significant differences in the sex, age, injury location, injury type, injury cause, complications, smoking, alcohol consumption, hospitalisation time, preoperative waiting time, or follow-up time between the two groups (Table 1). Furthermore, there was no statistical difference in the clinical data of the two groups (P > 0.05).
| Group | Quantity | Gender | Age (Yr) | Left or right | Neer type | Body height (cm) | Body weight (kg) | Cause of injury | Preoperative time (d) | Hospital stay (d) | Follow-up time (d) | Lost to follow-up | Refuse treatment | Complication |
| Group 1 | 22 | Male: 6 | 65.86 ± 7.00 | Left: 6 | Neer type Ⅲ: 12 | 163.09 ± 7.83 | 63.55 ± 10.87 | Walking injury: 14 | 5.35 ± 2.75 | 12.35 ± 4.21 | 18.55 ± 3.33 | 1 | 3 | Hypertension: 8 |
| Female: 16 | Right: 16 | Neer type Ⅳ: 10 | Collision: 2 | Diabetes: 3 | ||||||||||
| Trauma due to cycling: 6 | Cerebral infarction: 5 | |||||||||||||
| Group 2 | 25 | Male: 8 | 64.80 ± 4.66 | Left: 9 | Neer type Ⅲ: 15 | 164.60 ± 6.83 | 64.36 ± 6.93 | Walking injury: 17 | 6.08 ± 1.73 | 14.16 ± 3.00 | 20.72 ± 2.23 | 1 | 0 | Hypertension: 8 |
| Female: 17 | Right: 16 | Neer type Ⅳ: 10 | Collision: 4 | Diabetes: 5 | ||||||||||
| Trauma due to cycling: 4 | Cerebral infarction: 4 |
The ethics committee of the authors’ affiliation approved this study. All patients provided signed informed consent before surgery.
Before treating the proximal humerus comminuted fractures of patients in group 1, iodine and alcohol were used to disinfect the skin of the surgical field, and a sterile surgical sheet was placed after successful general anaesthesia. Before surgery was started, 1.0 g of tranexamic acid was administered intravenously. A deltopectoral approach was used for the injured shoulder, and layer-by-layer dissection of the subcutaneous tissue and fascia was performed. The cephalic vein was exposed and protected. The muscle space was entered and the proximal humerus was exposed. The intertubercular groove, which was used as the reduction landmark, was identified, and the greater and lesser tubercles of the humerus were discovered. The insertion points of the supraspinatus and teres major of the greater and lesser tubercles were sutured using the figure-of-8 technique (Vicryl 1-0 suture; Johnson & Johnsonon). This suture was reserved for traction reduction. Subsequently, the fractured ends were cleaned. The fibular segment was inserted in the humeral medullary cavity, and the humeral head was reduced. Then, the greater and lesser tuberosities were reset and fixed temporarily with Kirschner wires. The proximal humerus was fixed with a locking titanium plate (Shandong Weigao proximal humerus locking plate) under C-arm fluoroscopy if fracture reduction was considered good. The greater and lesser tuberosities were sutured to strengthen the fixation. The wound was thoroughly washed to stop the bleeding. Fracture reduction and internal fixation positions were examined using radiography. After evaluating the gauze instruments and confirming that reduction and fixation were satisfactory, the wound debris was washed with sterile saline, bleeding was completely stopped by electrocautery, and the wound was closed using the layer-by-layer technique.
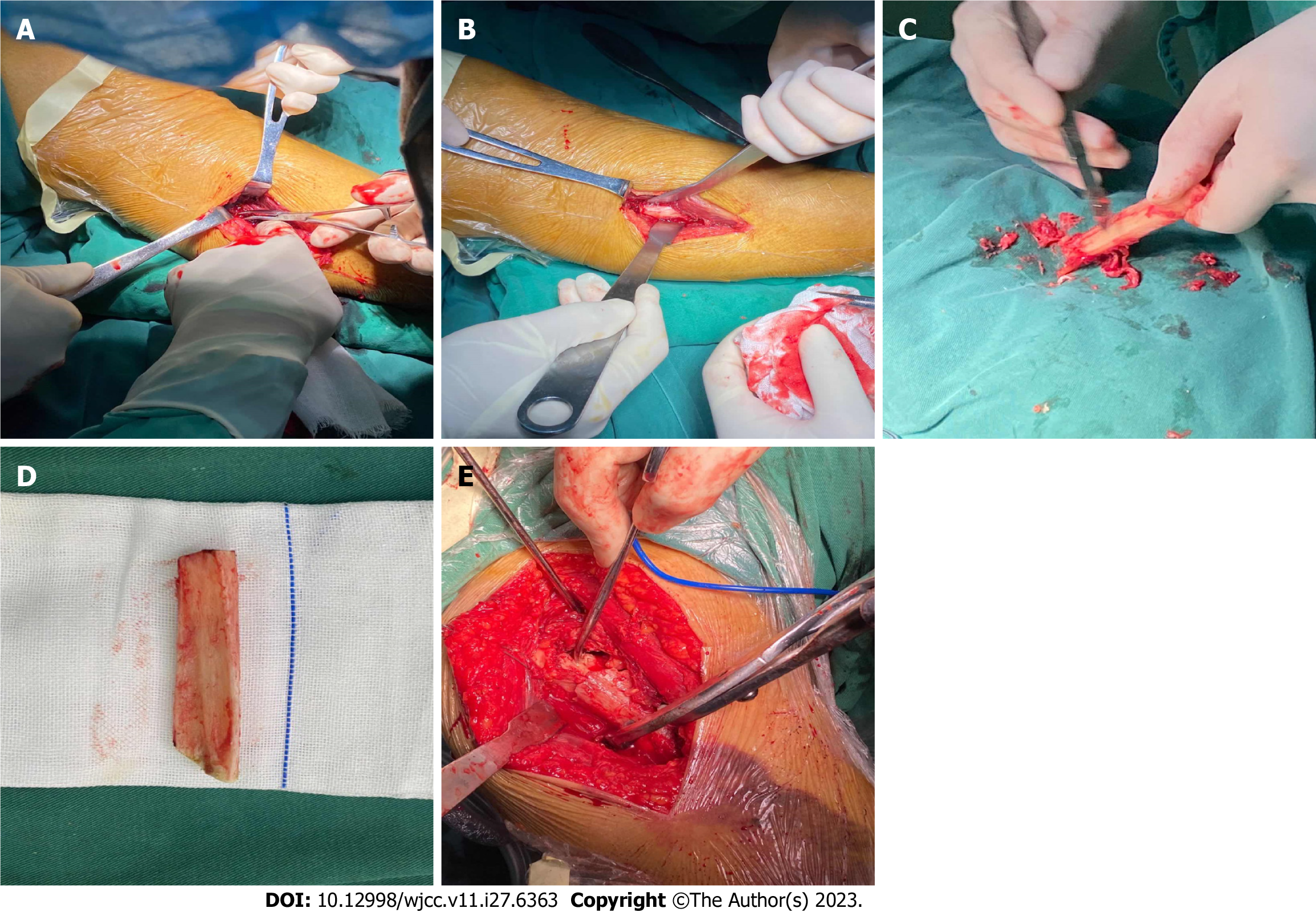
Before performing fibula removal for patients in group 1, the fibula length was determined through preoperative measurements of the radiograph. Approximately 7 to 8 cm can provide sufficient support and can be inserted in the longest length of the medullary cavity. Hence, the required fibular segment was measured and estimated using radiography before surgery. After successful general anaesthesia, the airbag tourniquet of the ipsilateral lower limb was inflated at 50 kPa. The skin of the surgical field was disinfected with iodine and alcohol, and a sterile surgical sheet was placed. A longitudinal incision was made at the middle and upper lateral sides of the ipsilateral leg, and the skin and subcutaneous fascia were incised. The fibula was exposed along the extensor flexor muscle space. Additionally, the superficial peroneal nerve was exposed and protected, and the fibula length was measured with a sterile ruler. A fibular segment with a length of approximately 7 to 8 cm was located in the proximal fibula and removed with a swing saw. The periosteum and other soft tissues on the surface of the fibular segment were cleaned. The tourniquet was slowly loosened. The wound was washed and bleeding was thoroughly stopped. The wound was sutured using the layer-by-layer technique (Figure 1). Insertion of a drainage tube in the wound was not necessary after surgery.
The surgical technique used to treat proximal humerus comminuted fractures of patients in group 2 was identical to that used for patients in group 1. However, a fibular autograft was not used for patients in group 2.
Patients were administered antibiotics once per hour before surgery; these antibiotics were continued for 24 h after surgery. Low-molecular-weight heparin was administered for 1 wk after surgery. Patients were allowed to leave their beds within 1 d of surgery. Use of the upper limb to lift any weight was not allowed for 8 wk. Passive pendulum movements were allowed within 6 wk of surgery. Active movement was allowed 6 wk after surgery. The rehabilitation training time and intensity of the two groups were adjusted appropriately based on the adaptability of the patients. Patients underwent routine dressing changes, and the sutures were removed 2 wk after surgery.
Patients were re-examined at 1, 2, 3, 6, and 12 mo after surgery, and their radiographs were re-examined regularly. The intraoperative blood loss volume from the shoulder wound, mean intraoperative blood loss volume from the leg wound, mean fibular length, shoulder wound pain score, leg wound pain score, fracture healing time, Constant-Murley scores of the injured joints at 3, 6, and 12 mo after surgery, Mallet scores of the injured joints at 3, 6, and 12 mo after surgery, and humeral neck-shaft angles during surgery and 12 mo after surgery were recorded. Constant-Murley shoulder function scores of the injured joints at 3, 6, and 12 mo after surgery were recorded as described previously[9]. We used a visual analogue scale to assess shoulder wound pain and leg wound pain on the first postoperative day[10]. The Mallet scores of the shoulder range of motion at 3, 6, and 12 mo after surgery were recorded[11]. The humeral neck-shaft angle 12 mo after surgery was measured and recorded[10]. The Holden walking function scores before and after surgery were also recorded[12].
There was no tenderness around the fracture and no percussion pain along the longitudinal axis of the limbs. The affected limb could be raised without discomfort. The upper limbs could be rotated with appropriate force without abnormal activity. Radiography showed a fuzzy fracture line and a continuous fracture line passing through the fracture end. Deformation at the fracture site was not observed during 2 wk of continuous observation. The injured limb could horizontally lift a weight of 1 kg for 1 min.
SPSS software (version 20.0) was used to analyse the data. The mean intraoperative blood loss volume from the shoulder wound, mean operative time (including shoulder surgery time and autogenous bone grafting time), shoulder wound pain, fracture healing time, Constant-Murley score of the shoulder joint, Mallet score of the shoulder joint, and humeral neck-shaft angle during surgery of the two groups were analysed using an independent sample t-test with α = 0.05.
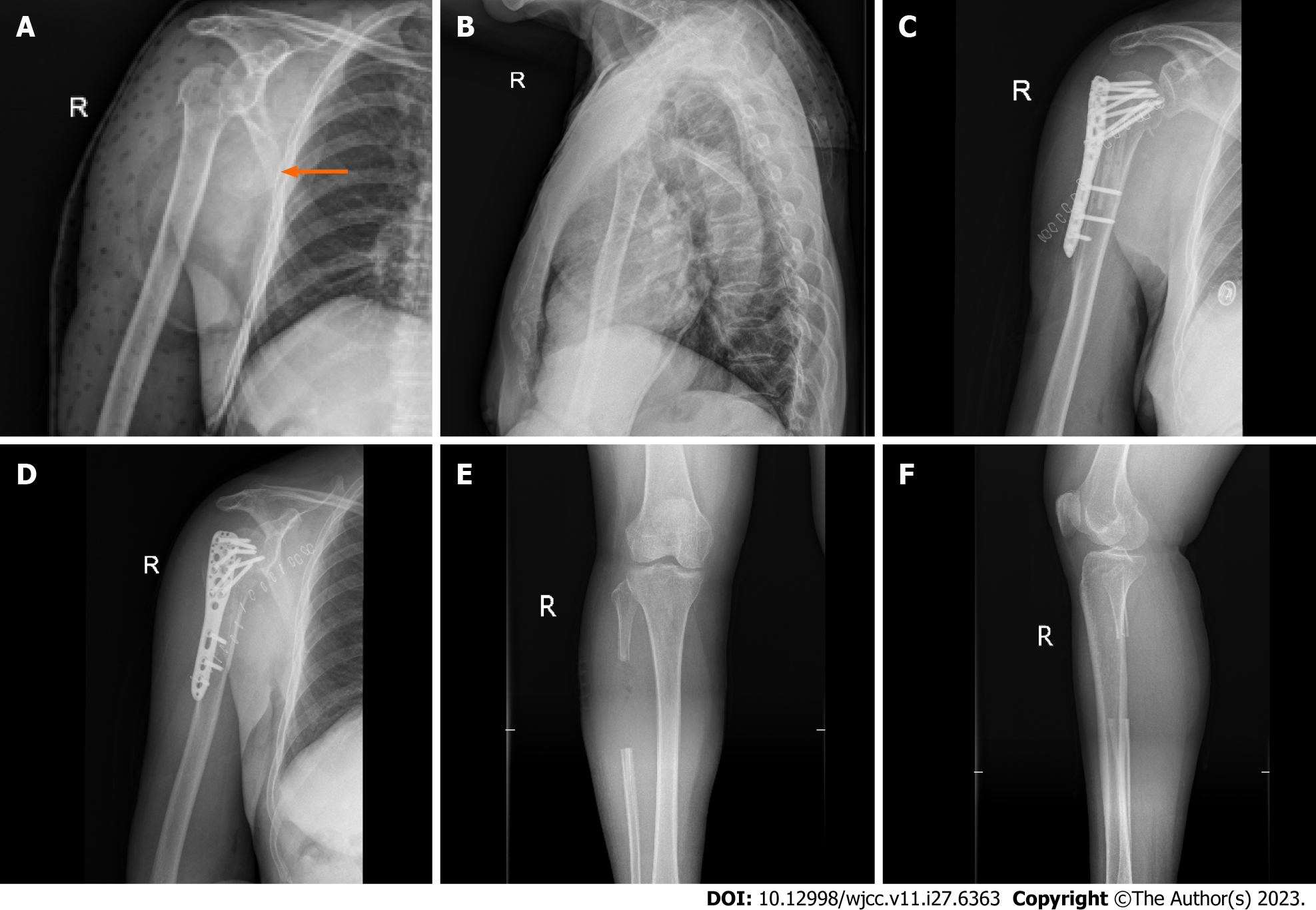
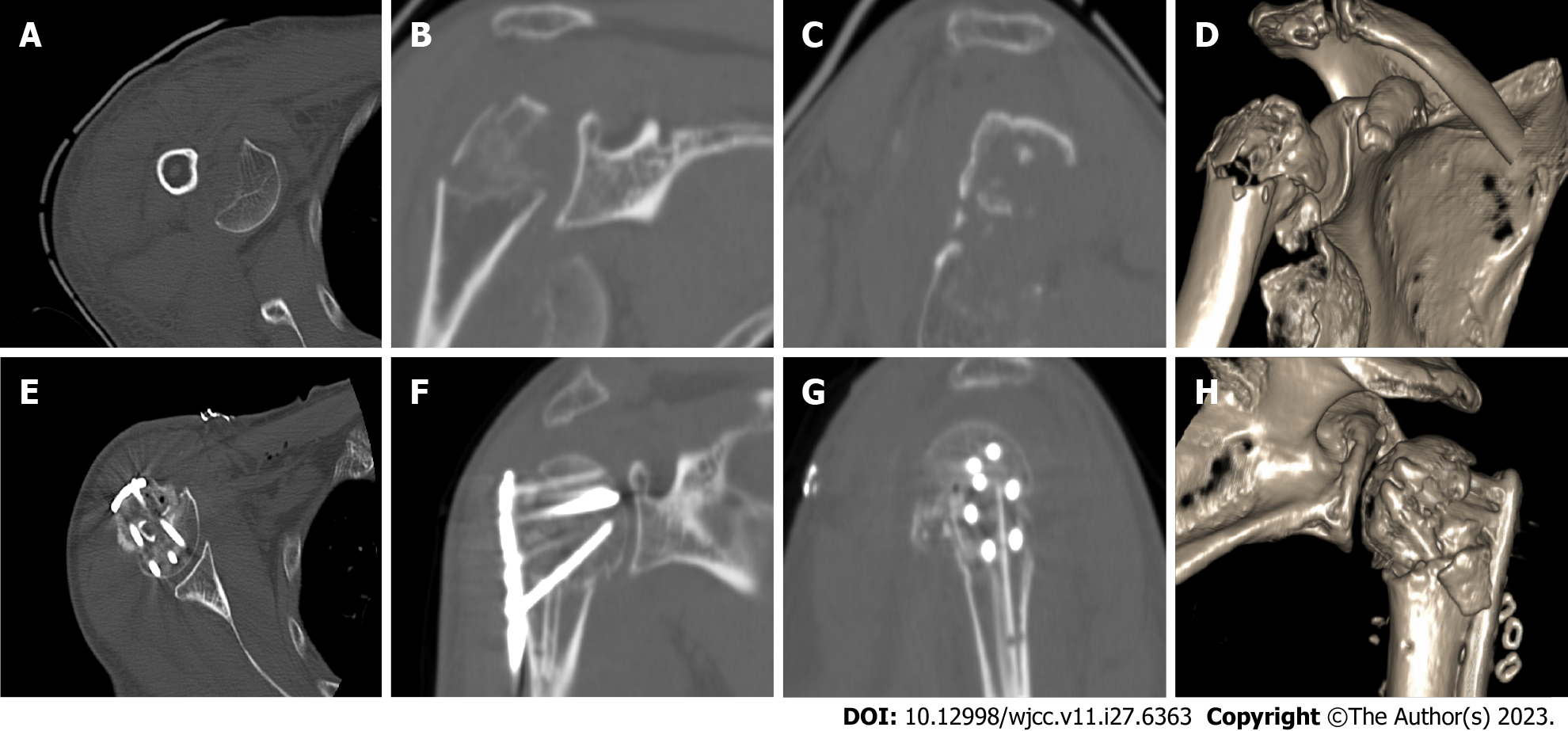
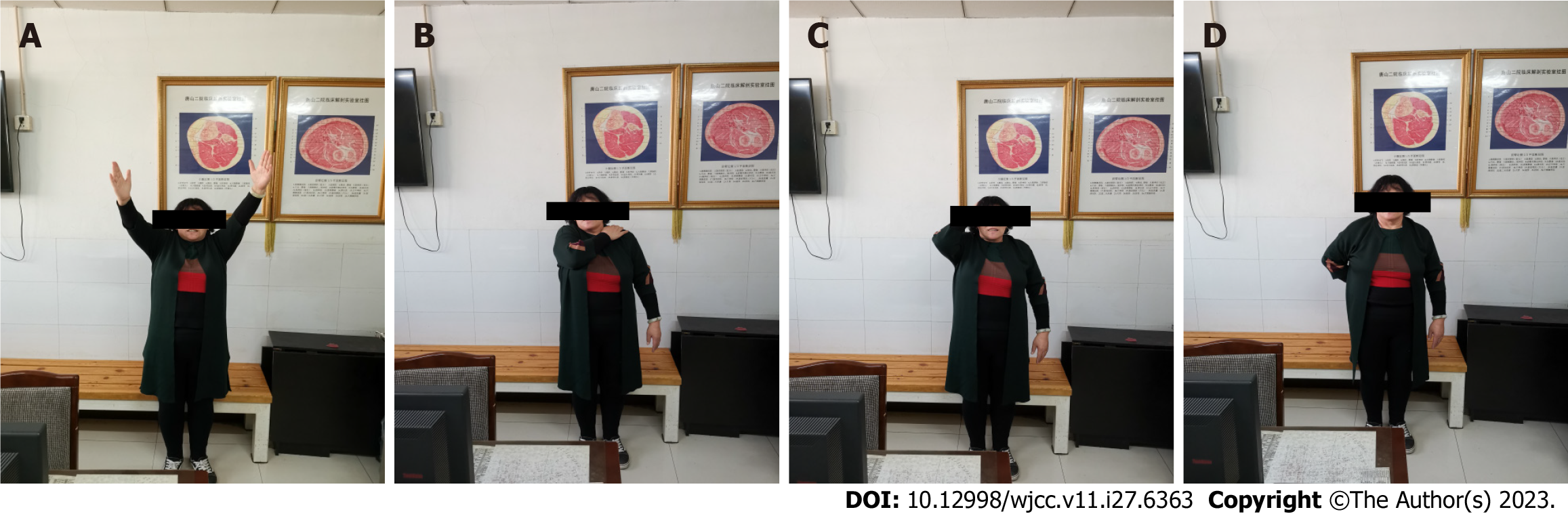
This study included 47 patients with complete follow-up data. No statistical difference in the mean intraoperative blood loss volume from the shoulder wound was observed between groups (Table 2). In group 1, the mean intraoperative blood loss volume from the leg wound was 37.27 mL (SD, ± 13.86 mL), and the mean fibula length was 7.64 cm (SD, ± 1.53 cm). Group 1 had a shorter mean operative time than group 2. Group 1 had a lower shoulder wound pain score on the first day after surgery than group 2. The leg wound pain score on the first day after surgery was 5.68 points (SD, ± 0.78 points). Group 1 had a shorter fracture healing time than group 2. Group 1 had higher Constant-Murley scores of the shoulder joint at 3, 6, and 12 mo after surgery than group 2. The preoperative and postoperative Holden walking function was grade V for patients in both groups. Group 1 had higher Mallet scores of the shoulder joint at 3, 6, and 12 mo after surgery than group 2. There was no difference in the humeral neck-shaft angles during surgery of groups 1 and 2. However, group 1 had larger humeral neck-shaft angles at 12 mo after surgery than group 2 (Table 2). The shoulder and calf wounds healed completely without infection or necrosis. Figures 2-4 are representative patient images.
| Parameter | Group 1 (n = 22) | Group (n = 25) | t value | P value | |
| Bloold loss from the shoulder wound (mL) | 390.91 ± 199.78 | 412.00 ± 148.10 | 0.414 | 0.681 | |
| Mean operation time (h) | 2.25 ± 0.30 | 2.76 ± 0.44 | 4.614 | < 0.001 | |
| Shoulder wound pain score (points) | 7.91 ± 1.15 | 8.56±1.00 | 2.072 | 0.044 | |
| Fracture healing time (mo) | 2.68 ± 0.48 | 3.64 ± 0.64 | 5.768 | < 0.001 | |
| Constant-Murley score of the shoulder (points) | At 3 mo | 76.64 ± 4.02 | 72.72 ± 3.02 | 3.804 | < 0.001 |
| At 6 mo | 86.36 ± 3.53 | 82.96 ± 3.40 | 3.367 | 0.002 | |
| At 12 mo | 87.95 ± 2.77 | 84.68 ± 2.63 | 4.159 | < 0.001 | |
| Holden walking function score (points) | Preoperation | V | V | ||
| Postoperation | V | V | |||
| Mallet score of the shoulder (points) | At 3 mo | 10.32 ± 0.57 | 9.96 ± 0.54 | 2.218 | 0.032 |
| At 6 mo | 13.36 ± 1.00 | 12.60 ± 0.87 | 2.803 | 0.007 | |
| At 12 mo | 13.91 ± 0.75 | 13.36 ± 0.70 | 2.595 | 0.013 | |
| Humeral neck-shaft angles (°) | Preoperation | 126.32 ± 4.91 | 126.72 ± 2.32 | 0.351 | 0.728 |
| Postoperation | 125.64 ± 4.63 | 122.96 ± 2.23 | 2.572 | 0.013 |
During this retrospective comparative cohort study, we observed better postoperative shoulder function scores among patients in group 1 with complete follow-up data. The mean operative time for proximal humeral comminuted fractures could be decreased by using locking plates with a fibular autograft because this approach can easily facilitate fracture reduction. A fibular autograft requires additional operative time; however, it decreases the proximal humeral fracture reduction time, thus shortening the overall operative time. The shoulder wound pain score of group 1 was lower, possibly because of the mild trauma and shorter operative time. Better postoperative scores were observed because stronger fixation can be achieved through fibular bone grafting, which could be beneficial for rehabilitation and maintaining the reduction position after surgery. Furthermore, a fibular autograft reduces postoperative reduction loss. Removal of the fibular segment had no significant effect on the walking function. The activity and function of the shoulder joint greatly improved within 6 mo after surgery. Functional improvement was not obvious 6 mo after surgery.
The autogenous fibular bone grafting method performed during this study decreased the surgical difficulty and increased the medial support of the proximal humerus. Additionally, it increased the fixed strength, allowed for insertion of the fibula in the medullary cavity, enabled closure of the greater and lesser tuberosities and humeral head of the fibular segment, simplified surgery, and facilitated fracture healing and postoperative recovery of function[13-15]. During a biomechanical study, Osterhoff et al[16] discovered that intramedullary fibula implantation could increase the fixation strength of fractures that cannot be easily shifted. Furthermore, Zhao et al[10] discovered that a fibular autograft combined with Philos titanium plate fixation resulted in satisfactory short-term support and maintenance of humeral head reduction of three-part and four-part proximal humeral fractures in elderly patients, and that it may decrease the complication rate associated with fixation using the Philos titanium plate alone. Proximal humeral fractures are more likely to cause loss of medial support of the humerus and affect fixation after reduction among elderly patients. A fibular autograft can recreate medial support and provide humeral head support. The screw is fixed on the fibular segment, resulting in more secure and reliable fixation[17]. The fibular segment is in the medullary cavity, which allows intramedullary fixation that is equivalent to a combination of intramedullary and extramedullary fixation. As a result, screw control is greatly enhanced and fixation strength is increased; therefore, this approach is suitable for elderly patients with osteoporosis[18]. Furthermore, it is beneficial to the performance of early rehabilitation exercises after fracture repair and avoids screw loosening and fracture displacement.
Indications for the use a fibular autograft are as follows: Elderly age; Neer type III or type IV fracture; osteoporosis accompanied by medial calcar comminution fractures; and lack of medial support. A fibular autograft is especially suitable when institutions do not have the resources to obtain a fibular allograft or perform artificial shoulder joint replacement. When removing the fibular segment, a length of 7 to 8 cm and a good preoperative plan are necessary. Furthermore, it is important to estimate the width and length of the medullary cavity. Additionally, the surgeon must ensure the length of the fibular segment because it may not be conducive to fracture reduction if it is too long or short. The autogenous fibula does not elicit rejection reactions and, compared with the ilium, it is long and strong. Moreover, it provides good support for the humeral head that is equivalent to that of allogeneic fibular segments[19]. Immune rejection has not been observed, and the source is convenient. Furthermore, removal of the fibular segment has no significant effect on walking.
Severe comminuted fractures are often accompanied by many fracture defects and a lack of medial support, which are important factors that lead to internal fixation failure[20-22]. Some patients agree to receive iliac bone grafts, which can promote fracture healing and fill some spaces; however, the amount of bone associated with such fractures is often too large, usually because of the lack of medial humeral head support, resulting in unstable fixation. The removed iliac bone does not fill the defect, and defect support and the recreation of medial support are difficult. However, a structural fibular bone graft with a suitable length can only recreate medial support[23]. Therefore, some surgeons attempt to implant an allogeneic fibula graft because these segments can provide support and produce satisfactory effects. However, fibular materials are limited, their cost is relatively high, immune rejection occurs, and some hospitals do not have the resources to perform these procedures[24]. Compared to the allogeneic fibular segment, the source of the autogenous fibular segment is more convenient and it can be harvested using a simple procedure without incurring additional or excessive medical expenses. Thus, patients are likely to consent to receiving autogenous fibular segments[25,26]. The disadvantage of autogenous fibular segments is that an additional incision is required, which might increase pain. Therefore, this surgery is not recommended for young patients. Surgery is mainly indicated for severe proximal humeral comminuted fractures lacking medial support. The long-term effects should be studied further because the number of patients in this study was small and the follow-up period was short. After outpatient follow-up, we maintained regular telephone contact with the patients. The longest follow-up period was 3 years. Patients maintained therapeutic effects that were the same of those experienced during outpatient follow-up, without new symptoms of discomfort.
The cost of surgery comprising locking plates with a fibular autograft is slightly more expensive than that of surgery involving traditional techniques. Furthermore, the pain experienced early after the use of locking plates with a fibular autograft is stronger than that associated with traditional treatment because of the wound resulting from bone removal. This pain is an inevitable side effect, however. The use of locking plates with a fibular autograft also has advantages, such as the ability to fill defects, reconstruction of medial support, increased fixation strength, decreased operative time, reduced surgical complexity, and earlier ability to function, resulting in better shoulder function recovery. In our region, fibular allograft materials are scarce and expensive[27]. Our description of this treatment method may have positive implications for proximal humeral fracture treatment in other regions with situations similar to ours.
An autologous fibula can be safely and easily obtained and is effective for bone grafting. It can recreate medial support, reduce postoperative reduction loss, facilitate fracture healing, and improve shoulder function. Furthermore, it does not impair the walking function. Therefore, it may be an effective treatment for severe proximal humerus comminuted fractures.
With the intensification of population aging, there are more and more patients with proximal humeral fractures. Elderly fractures are often accompanied by osteoporosis, which can easily lead to the loss of medial support and fixation failure. In recent years, research has shown that fibula resection is one of the methods for treating osteoarthritis in the elderly. Removing the fibula does not affect walking function, and allogeneic fibula material transplantation is a commonly used method to increase the fixation strength of proximal humeral fractures. However, allograft fibula materials are scarce and cannot be used in some areas. Autologous fibula transplantation is reliable and safe.
This study is to observe the therapeutic effect of autologous fibula graft and prove its effectiveness and safety, so as to improve the basis for autologous fibula graft in the treatment of proximal humeral fracture.
The purpose of this study is, on the one hand, to prove that autograft fibula transplantation can increase the fixation strength of humeral fracture, reconstruct the medial support, and obtain better surgical treatment effect; on the other hand, to prove that fibula resection has no impact on walking function, and to prove the safety of fibula bone extraction.
This retrospective, comparative cohort study comprised two groups of patients. Group 1 comprised 22 patients and group 2 comprised 25 patients with complete follow-up data. Group 1 was treated with a fibular autograft with open reduction and locking plates to enable internal fixation. Group 2 was treated with open reduction and locking plates to enable internal fixation. The intraoperative blood loss volume from the shoulder wound, operative time, shoulder wound pain, bone fracture healing time, Constant-Murley score of the shoulder joint, preoperative Holden walking function score, Mallet score of the shoulder joint, and humeral neck-shaft angle during surgery of the two groups were compared, and the differences were analysed using an independent sample t-test.
The use of autologous fibular bone grafting simplifies surgery, reduces surgical trauma, reconstructs the medial support of the humerus, increases fixation reliability, and achieves better postoperative shoulder joint function without affecting walking function. It is an effective treatment for comminuted proximal humeral fractures in the elderly.
Using locking plates with a fibular autograft may be an effective treatment option for severe proximal humerus comminuted fractures.
Our description of this treatment method may have positive implications for proximal humeral fracture treatment in other regions with situations similar to ours.
We are grateful for the support of all medical staff in the Fifth Ward of Orthopedic Trauma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Malkova TA, Russia; Rusimov L, Bulgaria; Salimi M, Iran S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M. The PHILOS plate for proximal humeral fractures--risk factors for complications at one year. J Trauma Acute Care Surg. 2012;72:783-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996;18:209S-213S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 169] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 219] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 4. | Lin T, Xiao B, Ma X, Fu D, Yang S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord. 2014;15:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Oppebøen S, Wikerøy AKB, Fuglesang HFS, Dolatowski FC, Randsborg PH. Calcar screws and adequate reduction reduced the risk of fixation failure in proximal humeral fractures treated with a locking plate: 190 patients followed for a mean of 3 years. J Orthop Surg Res. 2018;13:197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Omid R, Trasolini NA, Stone MA, Namdari S. Principles of Locking Plate Fixation of Proximal Humerus Fractures. J Am Acad Orthop Surg. 2021;29:e523-e535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Lenze U, Pohlig F, Knebel C, Lenze F, Harrasser N, Mühlhofer H, Toepfer A, Rechl H, von Eisenhart-Rothe R. [Autologous fibula transplantation for reconstruction of bone defects]. Orthopade. 2017;46:648-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Simovitch RW, Roche CP, Jones RB, Routman HD, Marczuk Y, Wright TW, Zuckerman JD. Effect of Tuberosity Healing on Clinical Outcomes in Elderly Patients Treated With a Reverse Shoulder Arthroplasty for 3- and 4-Part Proximal Humerus Fractures. J Orthop Trauma. 2019;33:e39-e45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Buchbinder R, Ramiro S, Huang H, Gagnier JJ, Jia Y, Whittle SL. Measures of Adult Shoulder Function. Arthritis Care Res (Hoboken). 2020;72 Suppl 10:250-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Zhao L, Qi YM, Yang L, Wang GR, Zheng SN, Wang Q, Liang B, Jiang CZ. Comparison of the Effects of Proximal Humeral Internal Locking System (PHILOS) Alone and PHILOS Combined with Fibular Allograft in the Treatment of Neer Three- or Four-part Proximal Humerus Fractures in the Elderly. Orthop Surg. 2019;11:1003-1012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Yilmaz V, Umay E, Tezel N, Gundogdu I. Timing of rehabilitation in children with obstetric upper trunk brachial plexus palsy. Childs Nerv Syst. 2018;34:1153-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Holden MK, Gill KM, Magliozzi MR. Gait assessment for neurologically impaired patients. Standards for outcome assessment. Phys Ther. 1986;66:1530-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22:195-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 14. | Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ. Proximal humeral fracture fixation: locking plate construct ± intramedullary fibular allograft. J Shoulder Elbow Surg. 2012;21:894-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M. Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech (Bristol, Avon). 2010;25:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Osterhoff G, Baumgartner D, Favre P, Wanner GA, Gerber H, Simmen HP, Werner CM. Medial support by fibula bone graft in angular stable plate fixation of proximal humeral fractures: an in vitro study with synthetic bone. J Shoulder Elbow Surg. 2011;20:740-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Hsiao CK, Tsai YJ, Yen CY, Lee CH, Yang TY, Tu YK. Intramedullary cortical bone strut improves the cyclic stability of osteoporotic proximal humeral fractures. BMC Musculoskelet Disord. 2017;18:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Schliemann B, Wähnert D, Theisen C, Herbort M, Kösters C, Raschke MJ, Weimann A. How to enhance the stability of locking plate fixation of proximal humerus fractures? An overview of current biomechanical and clinical data. Injury. 2015;46:1207-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 19. | Xing F, Duan X, Liu M, Huang F, Xiang Z. [Research progress in treatment of proximal humeral fracture with fibular allograft and locking plate]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Padhye KP, Kulkarni VS, Kulkarni GS, Kulkarni MG, Kulkarni S, Kulkarni R, Patil MD, Ravi PY. Plating, nailing, external fixation, and fibular strut grafting for non-union of humeral shaft fractures. J Orthop Surg (Hong Kong). 2013;21:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Lee SH, Han SS, Yoo BM, Kim JW. Outcomes of locking plate fixation with fibular allograft augmentation for proximal humeral fractures in osteoporotic patients: comparison with locking plate fixation alone. Bone Joint J. 2019;101-B:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 22. | Tuerxun M, Tuxun A, Zeng L, Wang Q, Chen Y. Locking Plate Combined With Endosteal Fibular Allograft Augmentation for Medial Column Comminuted Proximal Humeral Fracture. Orthopedics. 2020;43:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Jang Y, Kim D. Biomechanical study of Proximal humeral fracture fixation: Locking plate with medial support screw vs. locking plate with intramedullary fibular graft. Clin Biomech (Bristol, Avon). 2021;90:105510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Hudgens JL, Jang J, Aziz K, Best MJ, Srikumaran U. Three- and 4-part proximal humeral fracture fixation with an intramedullary cage: 1-year clinical and radiographic outcomes. J Shoulder Elbow Surg. 2019;28:S131-S137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Kim YG, Park KH, Kim JW, Oh JK, Yoon JP, Kim HJ, Oh CW. Is minimally invasive plate osteosynthesis superior to open plating for fixation of two-part fracture of the proximal humerus? J Orthop Surg (Hong Kong). 2019;27:2309499019836156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Chen H, Ji X, Zhang Q, Liang X, Tang P. Clinical outcomes of allograft with locking compression plates for elderly four-part proximal humerus fractures. J Orthop Surg Res. 2015;10:114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Kashayi-Chowdojirao S, Vallurupalli A, Chilakamarri VK, Patnala C, Chodavarapu LM, Kancherla NR, Khazi Syed AH. Role of autologous non-vascularised intramedullary fibular strut graft in humeral shaft nonunions following failed plating. J Clin Orthop Trauma. 2017;8:S21-S30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |