Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6304
Peer-review started: July 5, 2023
First decision: August 10, 2023
Revised: August 16, 2023
Accepted: August 21, 2023
Article in press: August 21, 2023
Published online: September 16, 2023
Processing time: 65 Days and 9 Hours
Dislocation of the long head of biceps tendon (LHBT) usually involves rotator cuff injury, and isolated dislocation with an intact rotator cuff is rare. Some cases of isolated dislocation have been reported. However, to the best of our knowledge, there has been no report of bilateral dislocation of the LHBT without rotator cuff pathology.
A 23-year-old male presented to our outpatient clinic with left side dominant pain in both shoulders. The patient had no history of trauma or overuse. The patient underwent intra-articular injection and physical therapy, but his symptoms aggra
This study describes a rare case of bilateral dislocations of the LHBT without ro
Core Tip: The long head of biceps tendon (LHBT), which has been regarded as a significant cause of anterior shoulder pain, often occurs with other shoulder pathologies. Trauma and repetitive mechanical wear can lead to development of biceps subluxation and dislocations. Association of sports activity and injury with LHBT pathology has also been reported. The subscapularis fiber function as the medial and proximal portion of the soft tissue sling and subscapularis lesions are almost always accompanied by dislocation. This report describes a rare case of bilateral dislocation of the LHBT without rotator cuff pathology.
- Citation: Sohn HJ, Cho CH, Kim DH. Bilateral dislocation of the long head of biceps tendon with intact rotator cuff tendon: A case report. World J Clin Cases 2023; 11(26): 6304-6310
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6304.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6304
The long head of biceps tendon (LHBT), which has been regarded as a significant cause of anterior shoulder pain, often occurs with other shoulder pathologies[1,2]. LHBT, which originates from the supraglenoid tubercle, runs within the intracapsular space, making a 30-degree turn into the bicipital groove. The bicipital groove is located between the greater and lesser tuberosities; this osseous component of the bicipital groove provides stability to the LHBT. The soft tissue system, including the coracohumeral ligament (CHL), superior glenohumeral ligament (SGHL), and interwoven fibers of the subscapularis and supraspinatus tendon, are the most important stabilizers[3-5]. Trauma and repetitive mechanical wear can lead to development of biceps subluxation and dislocations. Association of sports activity and injury with LHBT pathology has also been reported[6]. These cases usually involve pulley lesions. The SGHL/CHL complex and subscapularis fiber function as the medial and proximal portion of the soft tissue sling and subscapularis lesions are almost always accompanied by dislocation[7-11].
This report describes a rare case of bilateral dislocation of the LHBT without rotator cuff pathology. Some authors have reported on cases of isolated dislocation of the LHBT with an intact rotator cuff tendon[7,8,10,12,13]. However, to the best of our knowledge, there have been no reports of bilateral isolated dislocation of the LHBT without any event including trauma or overuse.
A 23-year-old male presented to our clinic with left side dominant pain in both shoulders.
Gradual aggravation of the patient’s symptoms occurred over the last year, even after physical therapy and intra-articular injection. The patient reported that raising his arm was difficult. The pain was more severe on the left side and became aggravated when lifting heavy objects.
The patient first visited our hospital four years ago, complaining of left side dominant pain in both shoulders. He was then diagnosed with impingement syndrome in both shoulders and visited another local hospital to undergo physical therapy and receive conservative management. After four years of conservative management, the patient returned to our clinic with aggravated pain in both shoulders.
The patient was a college student with no history of heavy loading activity or overuse, and there was no history of trau
On physical examination, the patient’s pain was localized to the bicipital groove area and lesser tuberosity in both shoulders. O’Brien test, Speed’s test, and Yegarson test showed a positive result in both shoulders. The patient’s range of motion (ROM) was in nearly normal range in both shoulders. The results of manual muscle testing showed no muscle weakness.
The results of preoperative laboratory tests were normal.
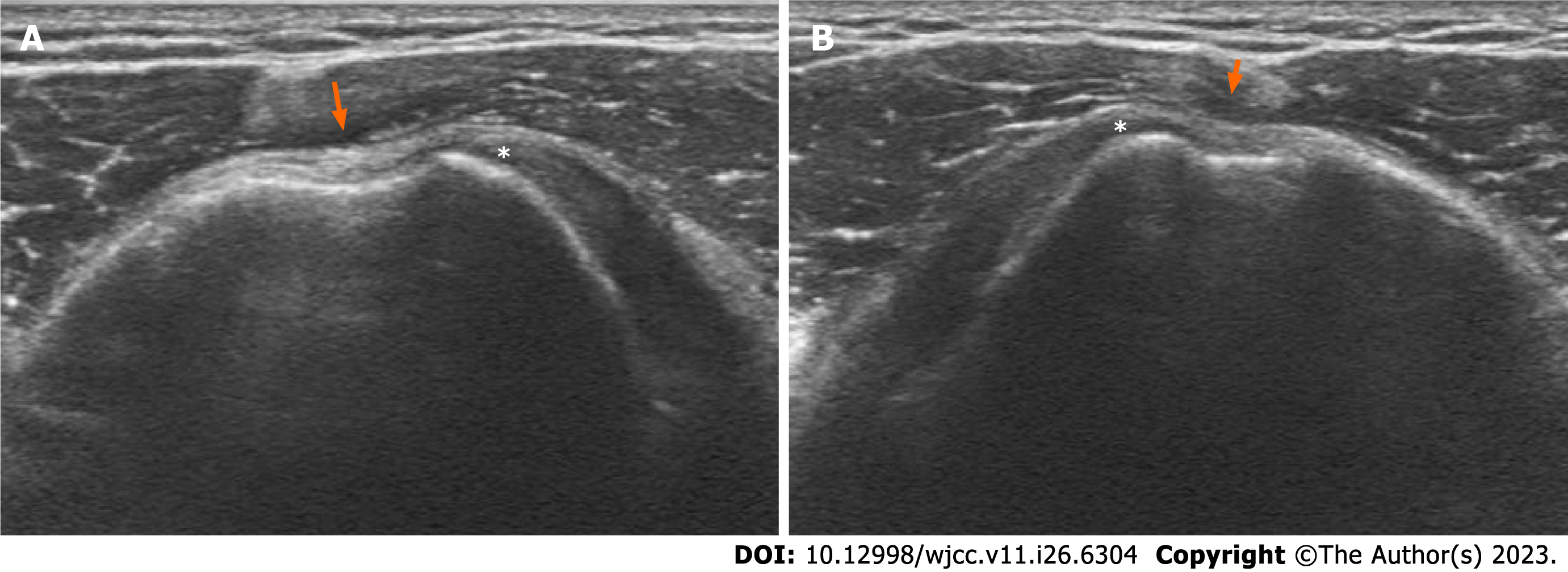
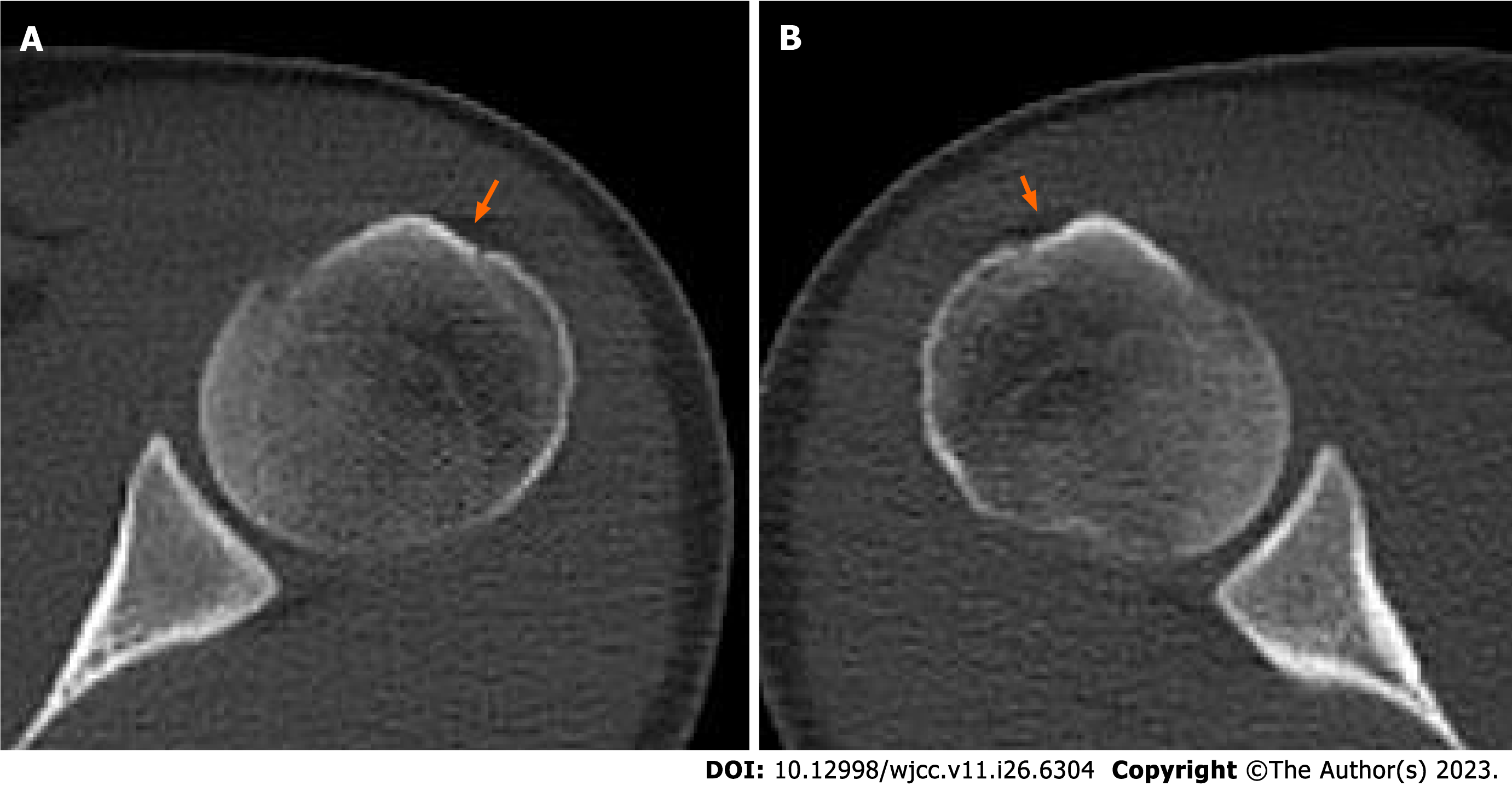
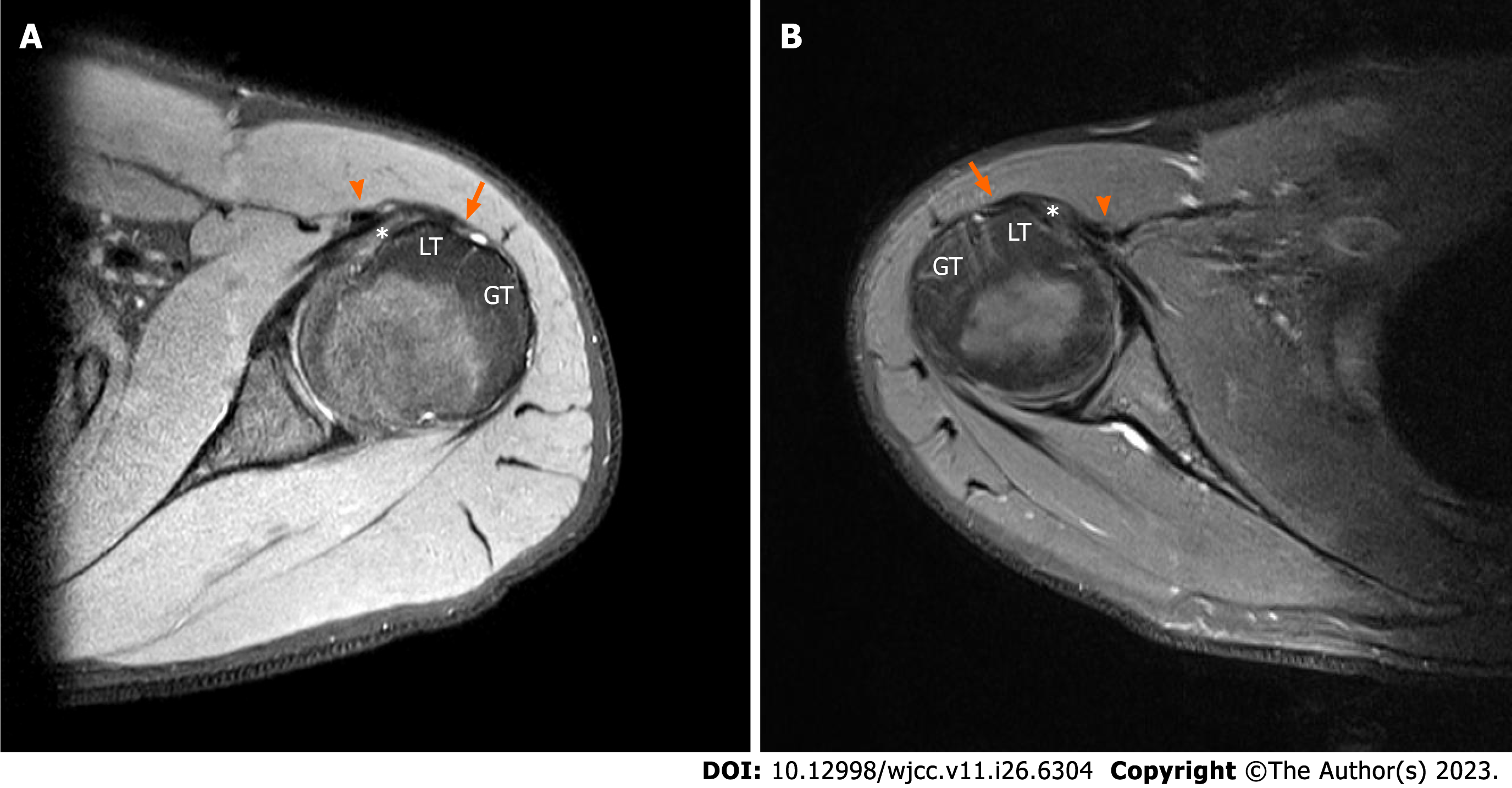
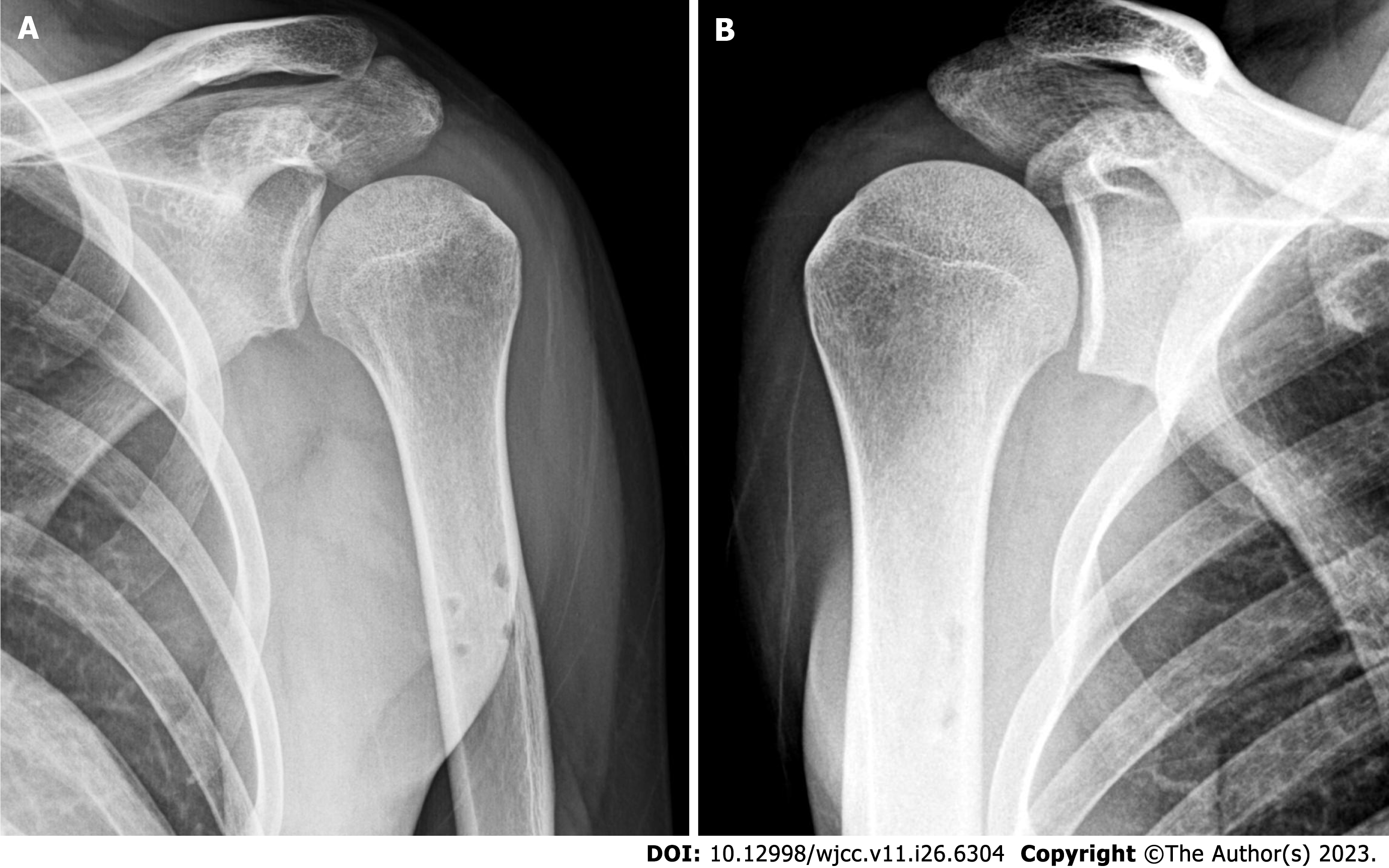
A simple radiograph showed no signs of bony anomaly. Shoulder ultrasonography showed a shallow bicipital groove with an intact subscapularis tendon in both shoulders (Figure 1). Computed tomography scan showed a dysplastic bicipital groove along with flattening of the medial wall of the groove (Figure 2). Preoperative magnetic resonance imaging (MRI) showed that the LHBT was medially dislocated in both shoulders. LHBT distance was 17.9 mm on left shoulder and 20.9 mm on right shoulder[14]. The subscapularis tendon and the supraspinatus tendon were intact on both sides (Figure 3). The morphology of the bicipital groove was examined using the technique introduced by Yoo et al[15]. The opening angle of the bicipital groove was 124.6 degrees on the right side and 137.0 degrees on the left side. The medial wall angle was 25.7 degrees on the right side and 21.4 degrees on the left side. The depth of each bicipital groove was 2.41 mm in the right shoulder, and 1.34 mm in the left shoulder. The bicipital groove in both shoulders was consi
The final diagnosis for the presented case was bilateral dislocations of the long head of bicep tendon (Walch classification type I, Bennett type 4) with dysplasia of both bicipital grooves.
Diagnostic shoulder arthroscopy was first performed on the left shoulder because the patient had left side dominant pain. A partial tear and synovitis of the LHBT were observed on the initial inspection. When the LHBT was pulled medially, active dislocation of the LHBT over the intact subscapularis tendon was detected (Figure 4A, Video). An asse
Surgical treatment of the right shoulder was administered after functional recovery had been achieved, four months after treatment of the left shoulder. Fraying of the biceps tendon pulley was detected by diagnostic arthroscopy. The LHBT was actively dislocated to the anterior side of the subscapularis tendon with application of medial traction (Figure 4B). As with the left shoulder, pulley release and subpectoral tenodesis were performed using a suture anchor (Figure 5B). The supraspinatus and subscapularis tendons were also intact. The patient started immediate postoperative continuous passive motion therapy with restriction of active elbow flexion. There were no complications in either shou
The patient’s symptoms showed significant improvement after subpectoral tenodesis. Before the surgery, the visual analogue scale (VAS) score was 5 and the score for subjective shoulder value (SSV) was 50%. The UCLA score was 21 for both shoulders and the American Shoulder and Elbow Surgeons (ASES) score was 58.33 prior to the surgery. Three months after left biceps tenodesis, the VAS score had improved to 2 with nearly full ROM, the UCLA score improved to 32, SSV improved to 60%, and the ASES score improved to 86.67. At the last follow-up, which was post-operative 22 mo on the left side and 18 mo on the right side, the VAS score was 1 with full ROM, and the UCLA score was 33 for both shoulders. The SSV score was 85%, and the ASES score had improved to 85. The patient returned to his ordinary life within three months after surgery, and he was satisfied with the functional improvement without pain at six months after surgery.
Many authors have reported that dislocation of the LHBT often involves rotator cuff pathology[7,9-11]. Desai and Mata[9], who reviewed 141 shoulders with full-thickness rotator cuff tear, asserted that the incidence of LHBT pathology was significantly greater for tears involving subscapularis. In addition, an increase in the size of the rotator cuff tear was statistically related to increased incidence of LHBT pathology. Walch et al[10] also emphasized that subluxation of the LHBT is always associated with minor lesions of subscapularis, and dislocation over a completely intact subscapularis is rare.
However, other authors have maintained that isolated dislocation of the LHBT might occur without rotator cuff injury. Ayoubi et al[17] reported on a case of bilateral dislocation without detection of any subscapularis tears. The patient’s symptoms were remarkably similar to those of our patient. However, our case did not involve the bifid subscapularis tendon, which is a rare congenital anomaly. The LHBT was located inside the substance of the subscapularis tendon. Instability of the biceps tendon with an intact rotator cuff due to injury in other stabilizing factors has also been noted. According to Gambill et al[8] and Vopat et al[12], isolated dislocation of the LHBT may occur as a result of injury in capsu
The stability of the LHBT can also be attributed to the osseous dimensions of the bicipital groove[3]. Yoo et al[15], who measured the depth of the bicipital groove, medial angle, and opening angle on shoulder MRI in order to examine the influence of bony morphology of the bicipital groove on the stability of the LHBT, concluded that bony morphology characterized by a shallow groove was associated with increased prevalence of LHBT instability. Levinsohn and Santelli[18] reported comparable results; a dislocated biceps tendon was detected on bicipital groove view on plain radiography in 58% of patients with a flattened bicipital groove and dysplasia of the lesser tuberosity. Because the medial wall of the bicipital groove functions as a trochlea about which the biceps tendon glides, the dysplasia of the medial wall and flat
In this study, the patient experienced pain in both shoulders caused by bilateral dislocation of the LHBT. Unlike a typical case, the dislocation was not associated with rotator cuff pathology or a traumatic event. Isolated dislocation of the LHBT was triggered by dysplasia of the bicipital groove in each shoulder. The patient underwent biceps tenodesis on both sides and satisfactory clinical and functional outcomes were finally achieved.
We have described a rare case of bilateral dislocation of the LHBT without previous trauma and rotator cuff injury. To the best of our knowledge, this is the first reported case to demonstrate that bilateral dislocation of the biceps tendon may occur as a result of dysplasia of the bicipital groove without rotator cuff pathology. Physical examination and evaluation of the bicipital groove should be emphasized in patients with anterior shoulder pain of unknown cause even in cases where it occurs bilaterally and without trauma or repetitive overhead activity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koumantakis GA, Greece; Oommen AT, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Dines D, Warren RF, Inglis AE. Surgical treatment of lesions of the long head of the biceps. Clin Orthop Relat Res. 1982;165-171. [PubMed] |
| 2. | Kim TM, Shin MH, Baek S, Lee DR, Chung SW. Can a Two Simple Stitches Method Provide Secure Fixation Strength in Biceps Tenodesis?: Biomechanical Evaluation of Various Suture Techniques. Clin Orthop Surg. 2022;14:426-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Varacallo M, Seaman TJ, Mair SD. Biceps Tendon Dislocation and Instability. 2022 Sep 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 4. | Park HB, Gwark JY, Na JB. Risk factors of chronic subscapularis tendon tear. Clin Shoulder Elb. 2022;25:257-264. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Kim JH, Min YK, Park MJ, Huh JW, Park JH. Postoperative clinical outcomes and radiological healing according to deep and superficial layer detachment in first facet involving subscapularis tendon tear. Clin Shoulder Elb. 2022;25:93-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Oh JH, Kim JY, Nam KP, Kang HD, Yeo JH. Immediate Changes and Recovery of the Supraspinatus, Long Head Biceps Tendon, and Range of Motion after Pitching in Youth Baseball Players: How Much Rest Is Needed after Pitching? Sonoelastography on the Supraspinatus Muscle-Tendon and Biceps Long Head Tendon. Clin Orthop Surg. 2021;13:385-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Ditsios K, Agathangelidis F, Boutsiadis A, Karataglis D, Papadopoulos P. Long head of the biceps pathology combined with rotator cuff tears. Adv Orthop. 2012;2012:405472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Gambill ML, Mologne TS, Provencher MT. Dislocation of the long head of the biceps tendon with intact subscapularis and supraspinatus tendons. J Shoulder Elbow Surg. 2006;15:e20-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Desai SS, Mata HK. Long Head of Biceps Tendon Pathology and Results of Tenotomy in Full-Thickness Reparable Rotator Cuff Tear. Arthroscopy. 2017;33:1971-1976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Walch G, Nové-Josserand L, Boileau P, Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998;7:100-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 228] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 11. | Farshad-Amacker NA, Jain Palrecha S, Farshad M. The primer for sports medicine professionals on imaging: the shoulder. Sports Health. 2013;5:50-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Vopat ML, Yang SY, Gregor CM, Kallail KJ, Saunders BM. Medial Dislocation of the Long Head of the Biceps without Concomitant Subscapularis Tear: A Case Report. J Orthop Case Rep. 2020;9:6-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Khazzam M, George MS, Churchill RS, Kuhn JE. Disorders of the long head of biceps tendon. J Shoulder Elbow Surg. 2012;21:136-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Zappia M, Ascione F, Di Pietto F, Fischetti M, Romano AM, Castagna A, Brunese L. Long head biceps tendon instability: diagnostic performance of known and new MRI diagnostic signs. Skeletal Radiol. 2021;50:1863-1871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Yoo JC, Iyyampillai G, Park D, Koh KH. The influence of bicipital groove morphology on the stability of the long head of the biceps tendon. J Orthop Surg (Hong Kong). 2017;25:2309499017717195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Abboud JA, Bartolozzi AR, Widmer BJ, DeMola PM. Bicipital groove morphology on MRI has no correlation to intra-articular biceps tendon pathology. J Shoulder Elbow Surg. 2010;19:790-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Ayoubi R, Darwish M, Nassour N, Aouad D, Maalouly J, Kanj V, El Rassi G. A rare case of an anatomical variation of bilateral long head of the biceps brachii tendons identified within the substance of bifid subscapularis tendons. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2021;23:18-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Levinsohn EM, Santelli ED. Bicipital groove dysplasia and medial dislocation of the biceps brachii tendon. Skeletal Radiol. 1991;20:419-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |