Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6246
Peer-review started: May 26, 2023
First decision: July 4, 2023
Revised: July 17, 2023
Accepted: August 21, 2023
Article in press: August 21, 2023
Published online: September 16, 2023
Processing time: 104 Days and 18.2 Hours
Congenital hepatic cysts are relatively rare but are now diagnosed earlier and more frequently with a routine prenatal ultrasound. Solitary liver cysts are divi
A 3-mo-old female infant was admitted to Mogadishu Somali Training and Resea
Congenital liver cysts are usually followed without complications. They rarely reach gigantic dimensions and may cause respiratory distress, intestinal obstruc
Core Tip: Liver simple cysts are a common disease; however, neonatal congenital ones are very rare and are usually followed without complications. Our patient presented with a giant simple liver cyst that caused serious complications. Unfortunately, for some of these patients surgical treatment is not curative, and deaths as a result of ongoing bile leakage are reported. Our patient, who underwent the appropriate surgical procedure, did not experience bile leakage and experienced definitive reco
- Citation: Küçük A, Mohamed SS, Abdi AM, Ali AY. Intestinal obstruction due to giant liver cyst: A case report. World J Clin Cases 2023; 11(26): 6246-6251
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6246.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6246
Simple liver cysts are the most common benign disease of the liver. Usually retention cysts originate from the biliary tract. In general, simple liver cysts are four times more common in women and seen in approximately 3%-4% of the population. The cysts are filled with clear fluid and do not contain bile, cells, or bacteria (i.e., sterile). The color of the cyst fluid can vary from clear, light yellow to brown[1]. The thin capsule of the simple liver cyst consists of dense fibrous tissue on the outside and the inside is lined with a single layer of columnar or cuboidal epithelium. The epithelial layer is present in most simple liver cysts but absent in a few. There is no mesenchymal stroma nor cellular atypia in the cyst wall. Characteristically, simple liver cysts are usually located in the right lobe of the liver and they do not open into the biliary tract. Size can range from a few millimeters to several decimeters. Very large (giant) simple liver cysts may cause atrophy in one lobe and hypertrophy in another[2].
Congenital hepatic cysts are relatively rare but are now diagnosed earlier and more frequently with a routine prenatal ultrasound. Solitary liver cysts are divided into simple and solitary intrahepatic biliary cysts, depending on the biliary connection. While some solitary liver cysts are symptomatic in childhood, even in newborns, they are often discovered incidentally in adults[3].
Simple liver cysts (especially small ones) are usually asymptomatic. When symptoms do occur, however, they can be elaborated as abdominal pain and/or a feeling of fullness in the abdomen along with nausea. The larger the cyst, the more likely it is to cause complaints. Case reports of spontaneous hemorrhage, infection, compression of the inferior vena cava, rupture, and biliary obstruction have been reported; although, these reports are rare among the literature, reflecting the rare nature of the cases themselves. The complications themselves are mainly observed in cases wherein the simple liver cysts reach large size. Most adult congenital liver cysts are asymptomatic and detected incidentally at autopsy or laparotomy. However, congenital liver cysts are extremely rare in infants and children. Usually, simple liver cysts in pediatric patients are treated (surgically) without complications[4]. Here, we present a 3-mo-old infant with a giant (10 cm × 10 cm × 14 cm) liver cyst leading to intestinal obstruction, vomiting and respiratory problems.
A 3-mo-old female infant was admitted to Mogadishu Somali Training and Research Hospital with recurrent vomiting, respiratory problems, and abdominal bloating complaints.
The patient was born at-home in Somalia via spontaneous vaginal delivery to a 22-year-old mother who had no prenatal care. The parents had 2 prior children, a male and a female, both of whom were also born at-home and reported as healthy. The parents were unable to provide data on the patient’s birth weight, first urination, first stool, time from birth to first cry, or time of first flatulence. The parents reported that the infant had not attended any other clinical visit, as they did not have the resources for such.
The parents reported witnessing no other issues since birth.
There was no relevant personal or family history.
The abdomen was greatly distended and extremely tight (Figure 1A). The patient had experienced repeated vomiting for 3 d, no stool output, and decreased urine.
At admission, the infant’s lab values were as follows: sodium: 128 mEq/L; potassium: 4.15 mEq/L; calcium: 8.1 mg/dL; albumin: 2.8 g/dL; white blood cell count: 21300/mL; C-reactive protein: 11.97 mg/L; platelets: 353000 mc/L; hemog
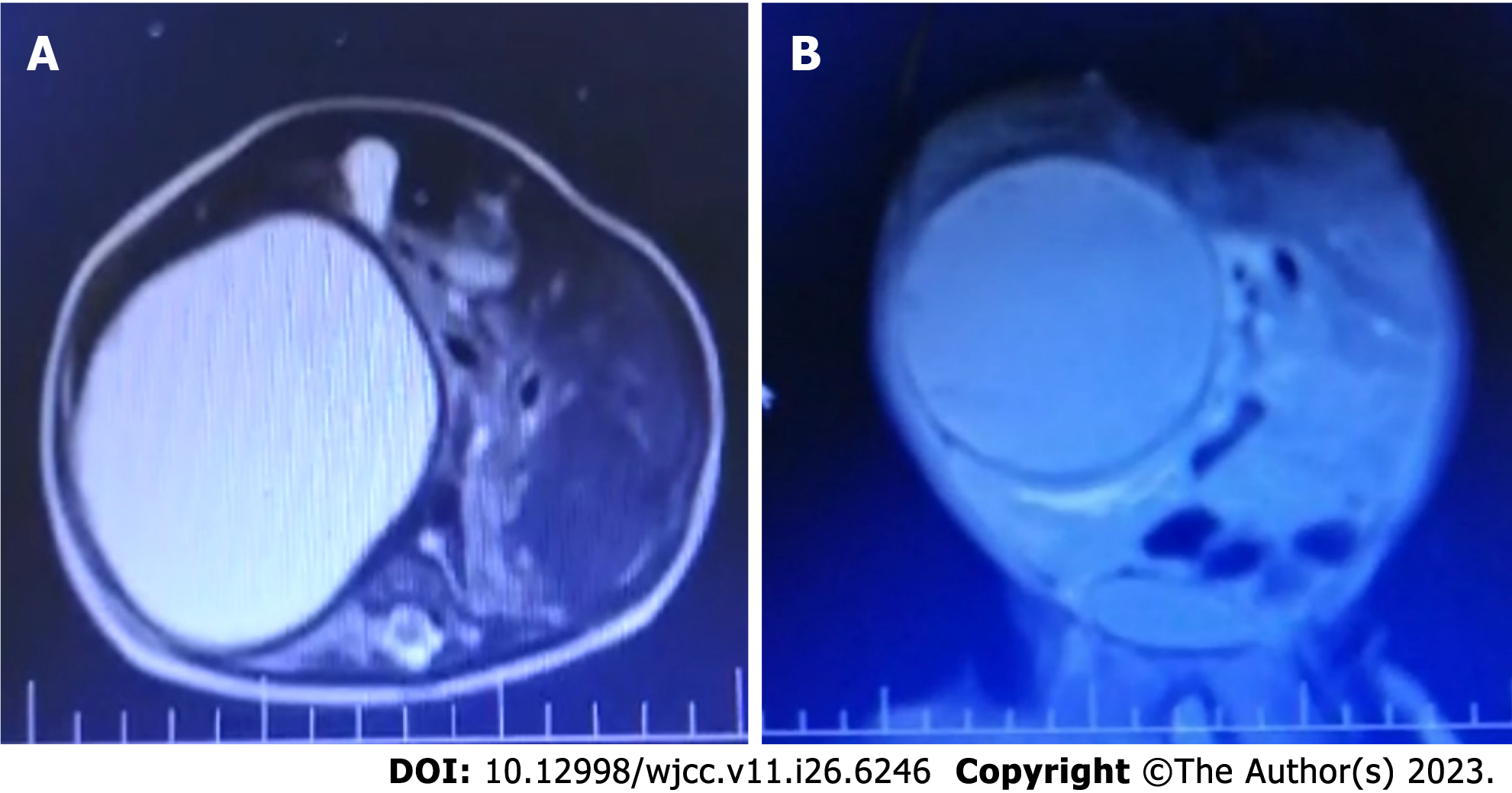
In standing direct abdominal X-ray (Figure 1B), it was observed that there was no intestinal gas passage. A complete obstruction was detected due to possible cystic pressure, and the intestines were shifted to the left lateral region of the abdomen. Abdominal ultrasonography (USG) detected a solitary cystic lesion measuring 10 cm × 10 cm × 14 cm, extend
Giant-size simple liver cyst.
Operation was decided as an emergency intervention. The patient was given standard treatment for fluid and elec
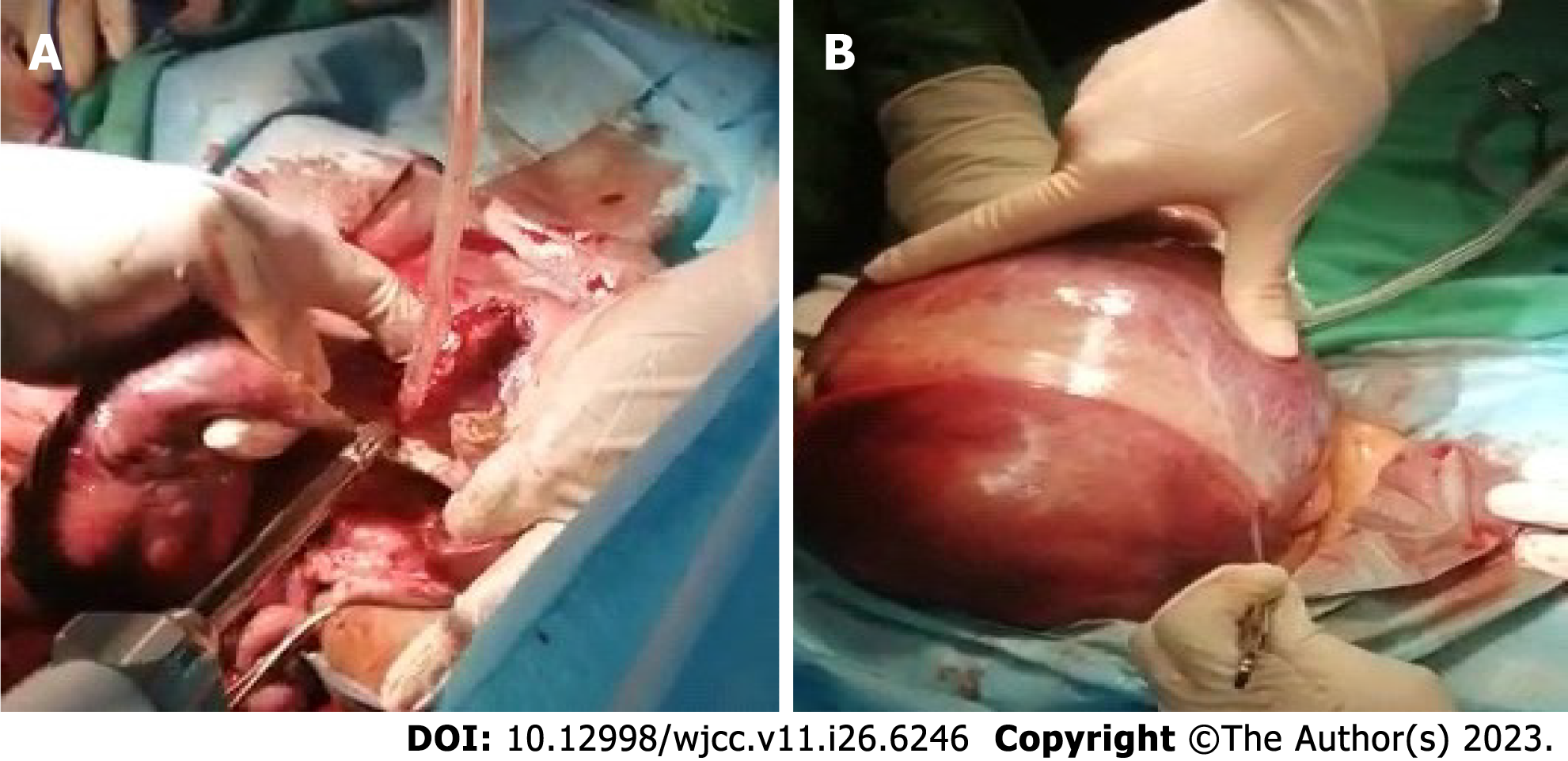
The cystic structure was opened by scalpel incision, and approximately 500 ccs of amber-colored liquid were aspirated. The cystic fluid did not change when exposed to atmospheric air. The liver-associated wall of the cyst was smooth. The sac wall adhering to the liver parenchymal structure and hilar structures was left intact, and the excised sac was turned with the help of LigaSure Retractable L-hook Laparoscopic Sealer/Divider, 44 cm (LF5644; Covidien, Dublin, Ireland) and sent to pathology. During the operation, there was approximately 50 ccs of blood loss, and the procedure was terminated by placing a drain.
Oral nutrition was initiated on the 2nd postoperative day, and the drain was removed on the 5th postoperative day. The patient visited the outpatient clinic control 1 mo later with no clinical complaints.
In USG, simple liver cysts appear as round or oval, unilocular (one piece), anechoic (black) fluid-filled lesions. The cyst wall is very thin and is difficult to detect in USG. Acoustic enhancement is seen behind the cyst (white glow). In Doppler USG, there is no bleeding in the cyst. A simple liver cyst is observed on computerized tomography (CT) as a smooth and sharply circumscribed water density. When intravenous contrast is given, it does not accumulate in the cyst. The cysts are usually uncomplicated (without bleeding or infection). On MRI, simple liver cysts are recognized by water intensity. The cyst reflects hypointensity on T1-weighted images and hyperintensity on T2-weighted images. There is no increase in intensity after intravenous contrast (gadolinium) administration[5].
Hydatid cysts, liver abscesses, biliary cystadenoma, choledochal cysts, and necrotic hepatic metastasis should be consi
Growing simple liver cysts should be evaluated for treatment, as enlarged cysts may not be simple liver cysts (they may be mucinous cystic carcinomas, benign or malignant). Aspiration of the cyst is rarely used for diagnostic purposes, but rather more so for therapeutic ones. When the cyst is drained percutaneously with a needle, the patient’s symptoms disappear, but they almost always relapse quickly. Sclerotherapy aims to damage the cyst’s epithelium and prevent fluid production. PAIR (percutaneous aspiration, installation of absolute alcohol) can be performed as a first-line treatment, and is safe and effective. However, the amount of alcohol (95% ethanol) administered into the cyst should be 100-120 mL. Alcohol intoxications have been reported following 240-3500 mL ethanol injections. Minocycline hydrochloride is also a good alternative to ethanol[8].
Laparoscopic removal of a part of the cyst (e.g., wide unroofing, wide fenestration) is another treatment alternative. Laparoscopic wide-opening of the cyst, or better complete removal of its free edges, is easy, safe and highly effective, and recurrence rate is low. The removed cyst wall is sent to pathology, and the liver surface is examined for signs of tumor formation. Fluid continues to be produced from the remaining cyst wall (epithelium) but is reabsorbed by the peritoneal cavity. Some authors recommend cauterizing the remaining cyst wall in the liver with argon laser or electrocautery. Com
Fenestration is appropriate treatment for very large hepatic cysts, as in our patient. This approach involves removing the cystic wall to establish a contact area. Close proximity of the cyst to the liver tissue and of the cyst wall to the paren
According to the European Association for the Study of the Liver 2022 Guideline, ultrasound is the imaging modality of choice to diagnose a simple hepatic cyst. If the cyst is diagnosed via USG, then CT and MRI might be unnecessary. Congenital hepatic cysts rarely induce compression of bile ducts. The peripheral bile duct dilatation-inducing cyst is usually centrally located (i.e., in liver segment 4). These patients may present with elevated alkaline phosphatase level and even jaundice[9].
Congenital liver cysts are usually followed without complications. They rarely reach gigantic dimensions, at which point they may cause respiratory distress, intestinal obstruction and recurrent vomiting. Surgery can provide quite successful outcomes in the treatment of giant sized simple liver cysts.
The editorial support of this article has been conducted by QA Executive Consultancy, Ozan Batigun MD, MBA in 2023.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fernandez-Portilla E, Mexico; Liu K, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Du CX, Lu CG, Li W, Tang WB. Congenital hepatic cyst: Eleven case reports. World J Clin Cases. 2022;10:9112-9120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Sharbidre K, Zahid M, Venkatesh SK, Bhati C, Lalwani N. Imaging of fibropolycystic liver disease. Abdom Radiol (NY). 2022;47:2356-2370. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Sakakibara S, Yamaguchi K, Hosokawa Y, Kohashi N, Ueda I, Sakamoto Y. Purification and some properties of rat liver cysteine oxidase (cysteine dioxygenase). Biochim Biophys Acta. 1976;422:273-279. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Bhosale M, Singh D. Giant congenital solitary nonparasitic cyst of the liver causing respiratory distress in a neonate. J Indian Assoc Pediatr Surg. 2016;21:72-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Alshaikhli A, Al-Hillan A. Liver Cystic Disease. 2023 Apr 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 6. | Cullen N, Alagtal MA, Byrne AT, Antao B. Surgical Dilemma: Exomphalos Major with Accessory Liver Lobe and Congenital Liver Cysts. J Indian Assoc Pediatr Surg. 2022;27:485-487. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Garcea G, Rajesh A, Dennison AR. Surgical management of cystic lesions in the liver. ANZ J Surg. 2013;83:E3-E20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Phancharoenkit N, Thienhiran A, Burasakarn P, Fuengfoo P, Hongjinda S. Acute cholangitis caused by a huge hepatic simple cyst: a case report. J Surg Case Rep. 2023;2023:rjad056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines on the management of cystic liver diseases. J Hepatol. 2022;77:1083-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |