Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6194
Peer-review started: May 27, 2023
First decision: July 23, 2023
Revised: August 2, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: September 16, 2023
Processing time: 104 Days and 3.4 Hours
Since fat does not transmit electrical energy well, delayed perforation and post-polypectomy syndrome due to electrical thermal injury are concerns in the endoscopic removal of colonic lipoma. The endoscopic submucosal dissection (ESD) technique concentrates electrical energy conducts to the submucosa, not the adipose tissue. This helps to minimize electrical thermal injury, especially in the case of large colonic lipomas. In rare cases, such as colonic lipomas accompanied by mucosal lesions, it is difficult for endoscopists to decide how to safely remove them.
A 78-year-old man underwent colonoscopy for colorectal cancer screening. During colonoscopy, a yellowish submucosal tumor with positive cushion sign was observed in the ascending colon measuring about 4.5 cm. A nodular mucosal lesion of about 2.5 cm was observed on the mucosal surface of the lipoma. The lipoma was so large that it occupied much of the inside of the colon, making it difficult to see the entire laterally spreading tumor (LST) at once. The LST was confined to the surface of the lipoma, which had a semipedunculated shape with a wide neck. The margin of the LST was not observed at the neck of the lipoma. ESD was performed and the colonic lipoma with the LST was successfully removed without complications. After 3 d of hospitalization, the patient was discharged without any symptoms. The final pathology report showed that the lesion consisted of submucosal lipoma and tubulovillous adenoma with low-grade dysplasia.
ESD is effective and safe for treating a large colonic lipoma with an LST by minimizing electrical thermal injury.
Core Tip: Most colonic lipomas are asymptomatic and do not require removal. Mucosal lesions of colorectal lipomas are rarely observed, but removal is necessary if there is a precancerous mucosal lesion such as tubular adenoma or tubulovillous adenoma. Due to the poor electrical conductivity of fat, excessive electrical energy during the endoscopic removal can cause complications. Endoscopic submucosal dissection is a preferred technique to minimize electrical thermal injury, especially for large colonic lipomas with a mucosal lesion.
- Citation: Bae JY, Kim HK, Kim YJ, Kim SW, Lee Y, Ryu CB, Lee MS. Large colonic lipoma with a laterally spreading tumor treated by endoscopic submucosal dissection: A case report. World J Clin Cases 2023; 11(26): 6194-6199
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6194
Colon cancer has the 3rd incidence and 2nd mortality rate in the overall population in a report on 36 cancers in 185 countries in 2020[1]. In Republic of Korea, colorectal cancer ranks 4th in incidence among all malignancies in the overall population, 3rd in males and 3rd in females, for both genders[2]. The fecal occult blood test is performed as a national screening program for colorectal cancer in Republic of Korea. In addition, the cases of colonoscopy have increased as well for the resection of colon polyps for more active prevention[3]. The increase in colonoscopy has led to the discovery of colon polyps in various forms and situations. This has challenged endoscopists as to whether to select and apply an appropriate endoscopic technique for polyp removal. Therefore, the authors report a rare case of treatment of a large colonic lipoma with a laterally spreading tumor (LST) and describe a safe and appropriate treatment strategy for it.
A 78-year-old man underwent colonoscopy for colorectal cancer screening.
The patient did not have any gastrointestinal symptoms or signs prior to colonoscopy.
The patient was diagnosed with a stroke 10 years ago.
The patient denied any family medical history.
The patient had no abnormalities in physical examination.
The patient had no abnormalities in blood and urine tests.
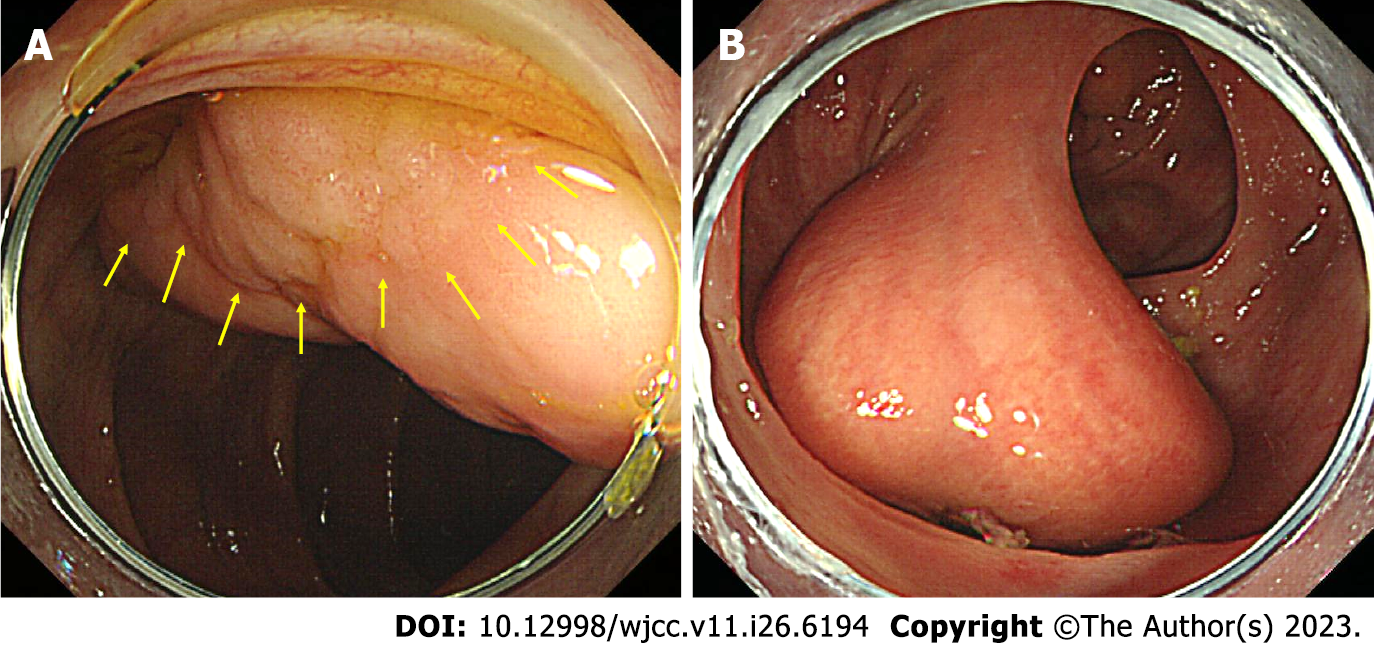
During colonoscopy, a yellowish submucosal tumor with positive cushion sign was observed in the ascending colon measuring about 4.5 cm. A nodular mucosal lesion measuring about 2.5 cm consisting of small nodules less than 3 mm in size was observed on the mucosal surface of the lipoma. Therefore, this lesion was diagnosed as a colonic lipoma with an LST of granular homogenous type. The LST was confined to the surface of the lipoma and the lipoma had a semipedunculated shape with a wide neck (Figure 1). A biopsy was performed and a tubular adenoma was diagnosed. The lipoma was so large that it occupied much of the inside of the colon, making it difficult to see the entire LST at once. It was considered difficult to remove using conventional endoscopic mucosal resection (EMR), and it seemed difficult to use an endoloop. But, the margin of the LST was not observed at the neck of the lipoma.
The diagnosis of the lesion was a large colonic lipoma with an LST of granular homogenous type.
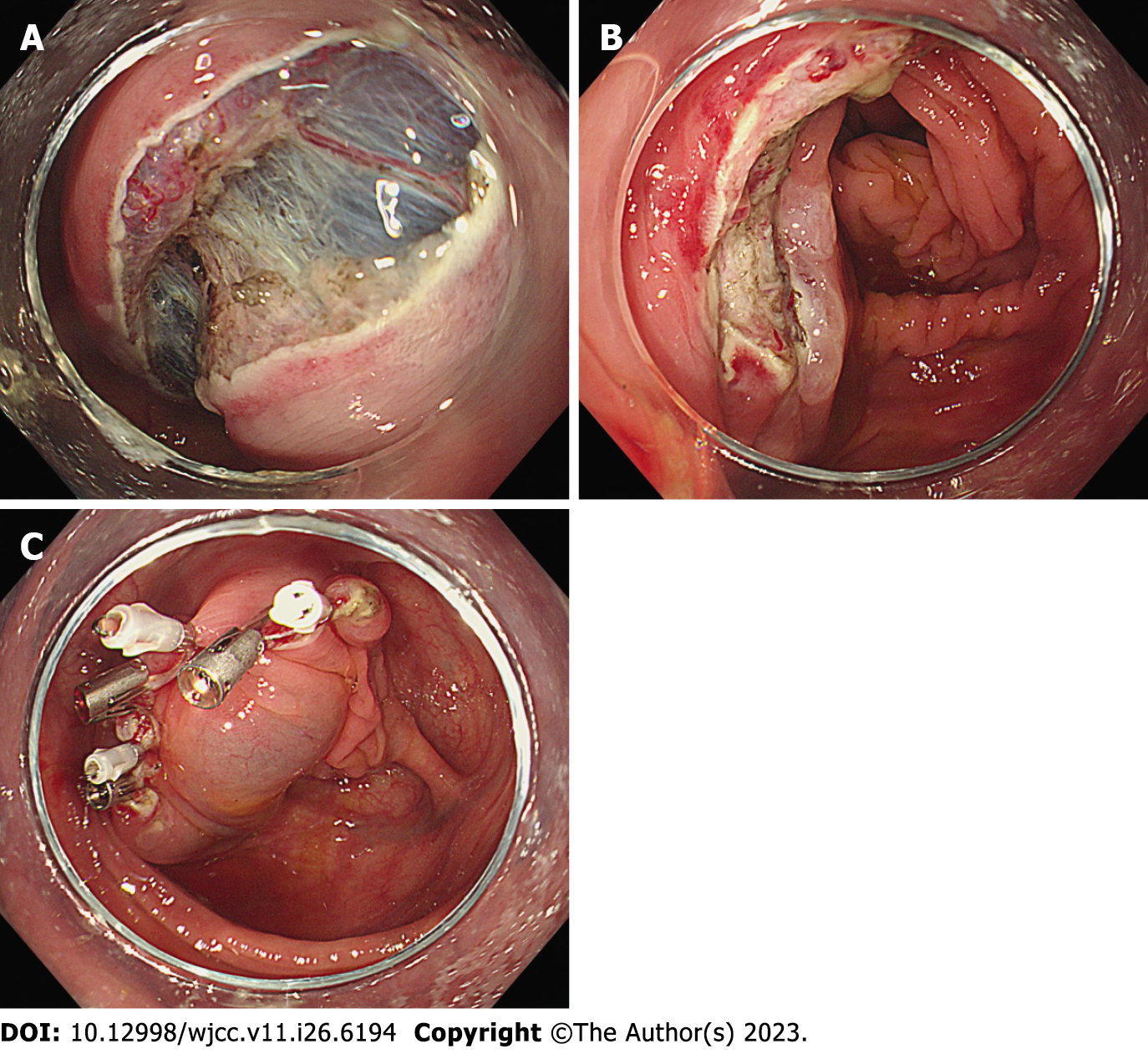
Endoscopic submucosal dissection (ESD) was planned to remove the lipoma with the LST. ESD was performed (procedure by Bae JY) using an HQ290 scope (Olympus, Tokyo, Japan), dual knife (Olympus, Tokyo, Japan), and IT nano knife (Olympus, Tokyo, Japan). As a submucosal injection solution, normal saline was mixed with indigo carmine dye. The patient’s posture was changed to the supine position during the procedure so that the lipoma was pulled in the direction of gravity and the neck of lipoma was well exposed. Complete closure was performed using six hemoclips to prevent delayed bleeding or perforation after the ESD procedure (Figure 2). The total procedure time was about 1 h.
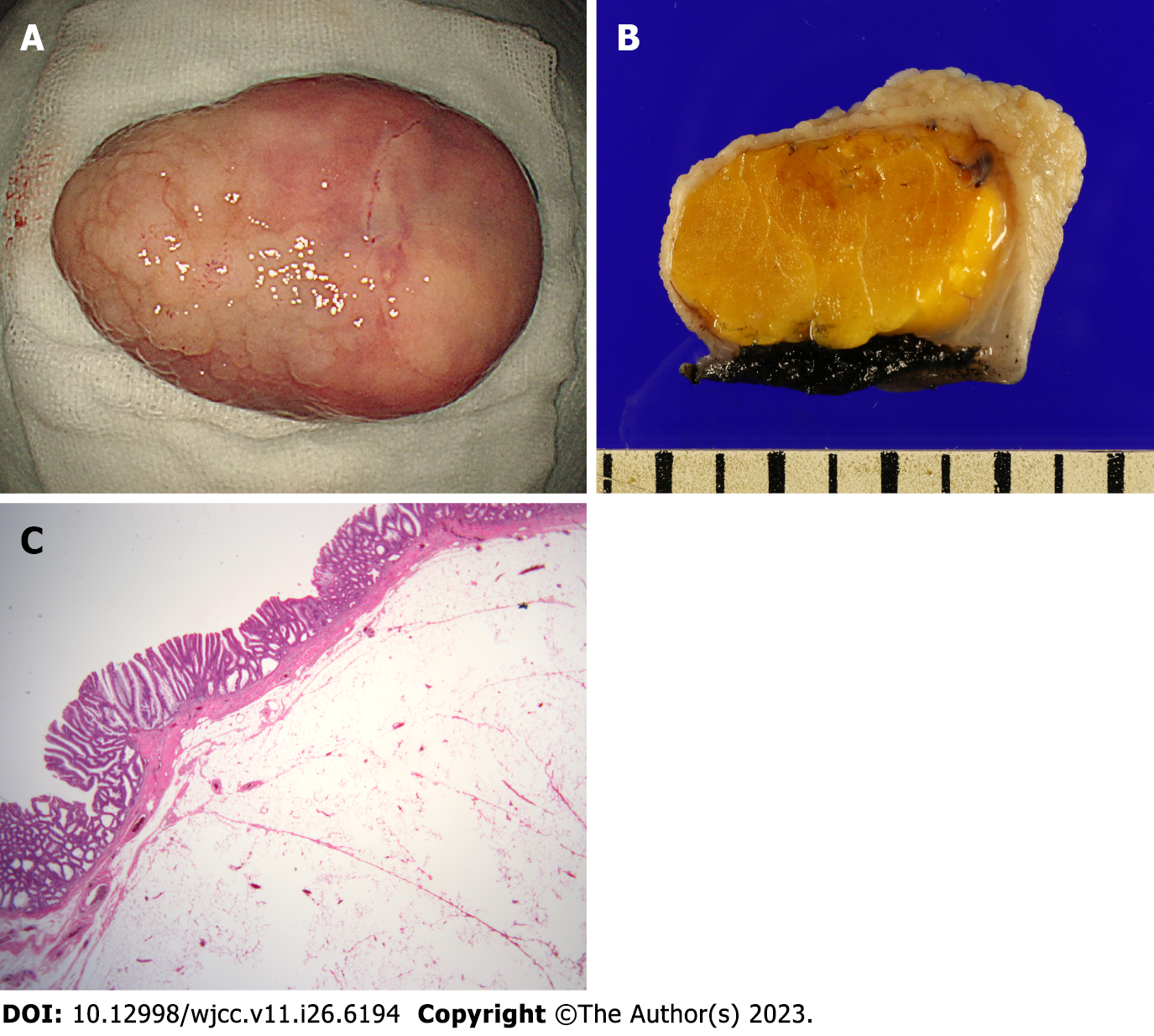
After 3 d of hospitalization, the patient was discharged without any symptoms. Final pathology report showed that the lesion consisted of submucosal lipoma and tubulovillous adenoma with low-grade dysplasia (Figure 3).
Colonic lipomas are discovered incidentally during abdominal ultrasound, abdominal computed tomography, or colonoscopy. Colonic lipoma shows a variable incidence of about 0.2% to 4.4%[4]. About 90% of colonic lipomas are located in the submucosal layer, showing a peduncle or sessile shape, and about 10% are located in the subserosal layer[4,5]. Symptomatic colonic lipomas are mainly related to size, and have been reported to vary in size from 0.35 cm to 10.00 cm, but are more likely to be symptomatic if they are larger than 2 cm[5]. There has been no established treatment method so far, and treatment is performed through endoscopic resection or surgical resection depending on the condition of the patient and lesion.
Colonic lipoma is mostly asymptomatic, but can sometimes be associated with complications. Reported complications included hemorrhage[6], obstruction[7], perforation[8], and intussusception[9]. All of these complications are caused by secondary colon damage to mechanical injury of the colonic lipoma. If the colonic lipoma is very large (more than 2 cm) or the patient’s symptoms and vital signs are unstable, surgical treatment should be considered first. However, due to the development of endoscopic techniques, endoscopic resection has been attempted in various colonic lipomas.
As the number of colonoscopies is increasing, there are rare reports of lesions found in the mucosa of colonic lipomas. Hyperplastic epithelium[10,11], tubular adenoma[12,13], and tubulovillous adenoma[14] have been reported on the mucosal surface of colonic lipoma (Table 1). In resection of these lesions, it is essential to minimize electrical thermal injury that may occur during removal of lipoma and to obtain a negative resection margin of mucosal lesion.
| Ref. | Sex/age | Location | Symptom/sign | Size of lipoma | Type of mucosal lesion | Size of mucosal lesion | Treatment |
| Yeom et al[10], 2013 | F/68 | Ascending colon | None | 9 mm | Hyperplastic and serrated epithelium | 9 mm | EMR |
| Radhi et al[11], 1997 | M/45 | Sigmoid colon | Abdominal pain, hematochezia/ diverticulitis, perforation | Not mentioned (estimated about 35 mm from the figure in the article) | Hyperplastic and serrated epithelium | Not mentioned | Surgery |
| Chu et al[12], 2009 | F/52 | Ascending colon | None | 30 mm | Tubular adenoma | 20 mm | EMR with endoloop |
| Nguyen et al[13], 2021 | M/71 | Hepatic flexure | None | Not mentioned (estimated about 33 mm from the figure in the article) | Tubular adenoma | 20 mm | EMR with 2 hemoclips |
| Moschetta et al[14], 2018 | M/49 | Transverse colon | Abdominal pain | 35 mm | Tubulovillous adenoma | Not mentioned | Surgery |
In general, the EMR technique can be applied for endoscopic removal of colonic lipoma. Since colonic lipomas often have a relatively wide base and have the characteristic of fat that does not conduct electrical energy well, the conventional EMR technique may have the risk of perforation or delayed perforation[15,16]. Therefore, an endoloop before procedure[12,17] or hemoclipping[7] after procedure may be helpful in the case of EMR. In order to avoid deep tissue damage or post-polypectomy syndrome, it may be better to avoid excessive coagulation and use a blended or pure cut[12]. Because removal of colonic lipomas using the EMR technique has these risks, there have been a report of removal using partial resection of the lipoma[18].
The ESD technique has also been reported to be used for endoscopic removal of colonic lipomas[19]. During ESD of colonic lipoma, electrical energy is concentrated only between the knife and the tissue and electrical energy is conducted to the submucosal layer, not the adipose tissue, so thermal injury can be minimized. In addition, the ESD technique has the advantage of being able to remove larger lesion than the EMR technique. In the case of colonic lipoma with a mucosal neoplasm, it is important to obtain a negative resection margin of the mucosal neoplasm. Compared to the EMR technique, the ESD technique can be performed by directly observing the marginal involvement of mucosal lesions, especially in large colonic lipomas.
It is thought that the ESD technique may be more helpful for endoscopic resection than the EMR technique in order to reduce tissue electrical thermal injury and obtain a negative resection margin in large colonic lipomas with a mucosal lesion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Andrejic-Visnjic B, Serbia; Batyrbekov K, Kazakhstan; Toyoshima O, Japan S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64132] [Article Influence: 16033.0] [Reference Citation Analysis (174)] |
| 2. | Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, Im JS, Seo HG; Community of Population-Based Regional Cancer Registries. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019. Cancer Res Treat. 2022;54:330-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 213] [Article Influence: 71.0] [Reference Citation Analysis (0)] |
| 3. | Cha JM, Kwak MS, Kim HS, Kim SY, Park S, Park GU, Lee JK, Kim SJ, Lee HH, Kim JS, Kim WH. Real-World National Colonoscopy Volume in Korea: A Nationwide Population-Based Study over 12 Years. Gut Liver. 2020;14:338-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Nallamothu G, Adler DG. Large colonic lipomas. Gastroenterol Hepatol (N Y). 2011;7:490-492. [PubMed] |
| 5. | Zhang H, Cong JC, Chen CS, Qiao L, Liu EQ. Submucous colon lipoma: a case report and review of the literature. World J Gastroenterol. 2005;11:3167-3169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Rodriguez DI, Drehner DM, Beck DE, McCauley CE. Colonic lipoma as a source of massive hemorrhage. Report of a case. Dis Colon Rectum. 1990;33:977-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Liyen Cartelle A, Uy PP, Yap JEL. Giant Colonic Lipoma Presenting as Intermittent Colonic Obstruction With Hematochezia. Cureus. 2020;12:e11434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Kumar L, Laksman TK. Giant submucosal lipomatous polyp causing perforation of sigmoid colon: a case report and review of literature. J Clin Diagn Res. 2015;9:PD22-PD24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Lee CS, Lee MJ, Kim KL, Kim YS, Baik GH, Kim JB, Kim DJ, Han SH. A case of giant lipoma causing chronic recurrent intussusception of the colon. Clin Endosc. 2012;45:165-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Yeom JO, Kim SY, Jang EC, Yu JY, Chang ED, Cho YS. Colonic lipoma covered by hyperplastic epithelium: Case report. World J Clin Cases. 2013;1:124-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Radhi JM, Haig TH. Lipoma of the colon with overlying hyperplastic epithelium. Can J Gastroenterol. 1997;11:694-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Chu SJ, Kim JS, Kim BW. Tubular adenoma overlying a colonic lipoma resected by endoscopic resection with use of a detachable endoloop. Gastrointest Endosc. 2019;89:894-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 13. | Nguyen N, Castano J, Rapoport G, Albustamy A, Zamir A. S1923 A Rare Case of Adenomatous Polyp Overlying a Colonic Lipoma. ACG. 2021;116:S844. [DOI] [Full Text] |
| 14. | Moschetta M, Virelli R, Laricchia F, Alberotanza V, Telegrafo M, Angelelli G, Stabile Ianora AA. Lipoma of the transverse colon covered by tubulovillous adenoma: a rare indication for surgical treatment. G Chir. 2018;39:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Bahadursingh AM, Robbins PL, Longo WE. Giant submucosal sigmoid colon lipoma. Am J Surg. 2003;186:81-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Chase MP, Yarze JC. "Giant" colon lipoma--to attempt endoscopic resection or not? Am J Gastroenterol. 2000;95:2143-2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Shi L, Zhao Y, Li W. Endoscopic resection of a giant colonic lipoma with endoloop-assisted unroofing technique: A case report. Medicine (Baltimore). 2018;97:e10995. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Kim GW, Kwon CI, Song SH, Jin SM, Kim KH, Moon JH, Hong SP, Park PW. Endoscopic resection of giant colonic lipoma: case series with partial resection. Clin Endosc. 2013;46:586-590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Lee JM, Kim JH, Kim M, Lee YB, Lee JH, Lim CW. Endoscopic submucosal dissection of a large colonic lipoma: Report of two cases. World J Gastroenterol. 2015;21:3127-3131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |