Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6170
Peer-review started: May 6, 2023
First decision: August 2, 2023
Revised: August 3, 2023
Accepted: August 11, 2023
Article in press: August 11, 2023
Published online: September 16, 2023
Processing time: 124 Days and 21.4 Hours
Fibrous dysplasia associated with aneurysmal bone cyst (ABC)-like changes in the right proximal femur has a low incidence. It is considered more difficult to make early diagnosis than for single fibrous dysplasia.
A 14-year-old woman was admitted because of persistent pain in the right hip and abnormal gait over the previous 2 mo. She had no history of present or past illness. Preoperative photography, enhanced computed tomography, and magnetic resonance imaging showed ground-glass appearance with cortical scalloping and expansion of the right proximal femur and femoral neck. Pathological examination by preoperative puncture biopsy revealed fibrous dysplasia of the right proximal femur. The patient was diagnosed with fibrous dysplasia based on medical history, physical examination, and results of laboratory, imaging and pathological examinations. According to final patho
We report a cases of fibrous dysplasia associated with ABC-like changes in the right proximal femur treated with curettage and allograft along with hip compression screws.
Core Tip: The incidence of fibrous dysplasia associated with aneurysmal bone cyst-like changes in the right proximal femur is low. It is considered more difficult to make early diagnosis than for single fibrous dysplasia. For fibrous dysplasia, curettage and allograft combined with internal fixation are the gold-standard treatments. The therapeutic options for aneurysmal bone cyst (ABC) include curettage with or without adjuncts, bone grafting or bone substitutes, image-guided sclerotherapy with various sclerosing agents, and monoclonal antibodies. We here report a case of fibrous dysplasia associated with ABC-like changes in the right proximal femur treated with curettage and allograft along with hip compression screws.
- Citation: Xie LL, Yuan X, Zhu HX, Pu D. Surgery for fibrous dysplasia associated with aneurysmal-bone-cyst-like changes in right proximal femur: A case report. World J Clin Cases 2023; 11(26): 6170-6175
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6170.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6170
Fibrous dysplasia is a mosaic disease of bone, with bone replaced by fibro-osseous tissue or irregular trabeculae of woven bone intermixed with mature collagenous tissue[1]. Surgery for fibrous dysplasia of the femoral neck consists of autogenous cancellous bone graft with or without allograft, fibular graft and fixation with hip compression screws, in addition to autogenous cancellous bone and allograft[2]. Aneurysmal bone cyst (ABC) is a true neoplasm with features of a benign but locally aggressive lesion that predominantly affects children and young adults, and it accounts for approximately 70% of cases. The therapeutic options for ABC include curettage with or without adjuncts, bone grafting or bone substitution, image-guided sclerotherapy with various sclerosing agents, and monoclonal antibodies. ABC-like changes associated with other bone neoplasms or secondary ABC accounts for the remaining 30% of cases[3]. Here, we report a rare case of fibrous dysplasia of the right proximal femur associated with ABC-like changes.
A young female patient aged 14 years complained of persistent pain in the right hip and abnormal gait during the previous 2 mo, but without any symptoms in her limbs or trunk, such as, numbness, fatigue or lameness.
The patient had no history of present or past illness.
No history of personal and family illness.
The patient had no history of present or past illness, and no history of personal and family illness.
Physical examination indicated that the right hip had pressing and tenderness pain. Sensation test, strengthening test, and tendon reflex test were normal in both lower limbs. No pathological signs were observed upon physical examination. Visual analog scale score was 4 points.
Laboratory examinations were normal.
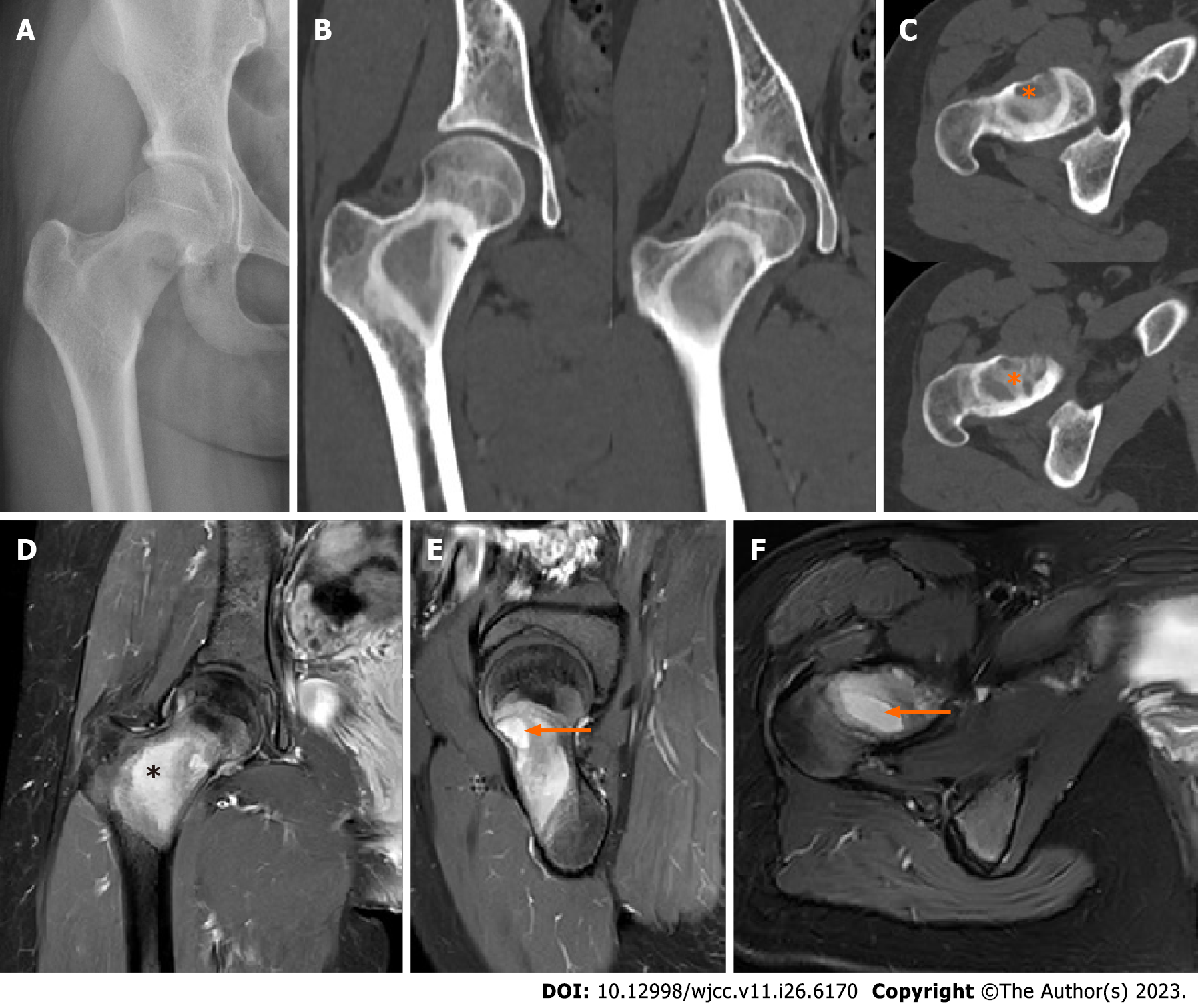
Preoperative photography, enhanced computed tomography (CT), and magnetic resonance imaging (MRI) showed ground-glass” appearance with cortical scalloping and expansion of the right proximal femur and femoral neck (Figure 1). No pathological fracture of the lesion site or classic shepherd crook deformity of the right proximal femur was observed.
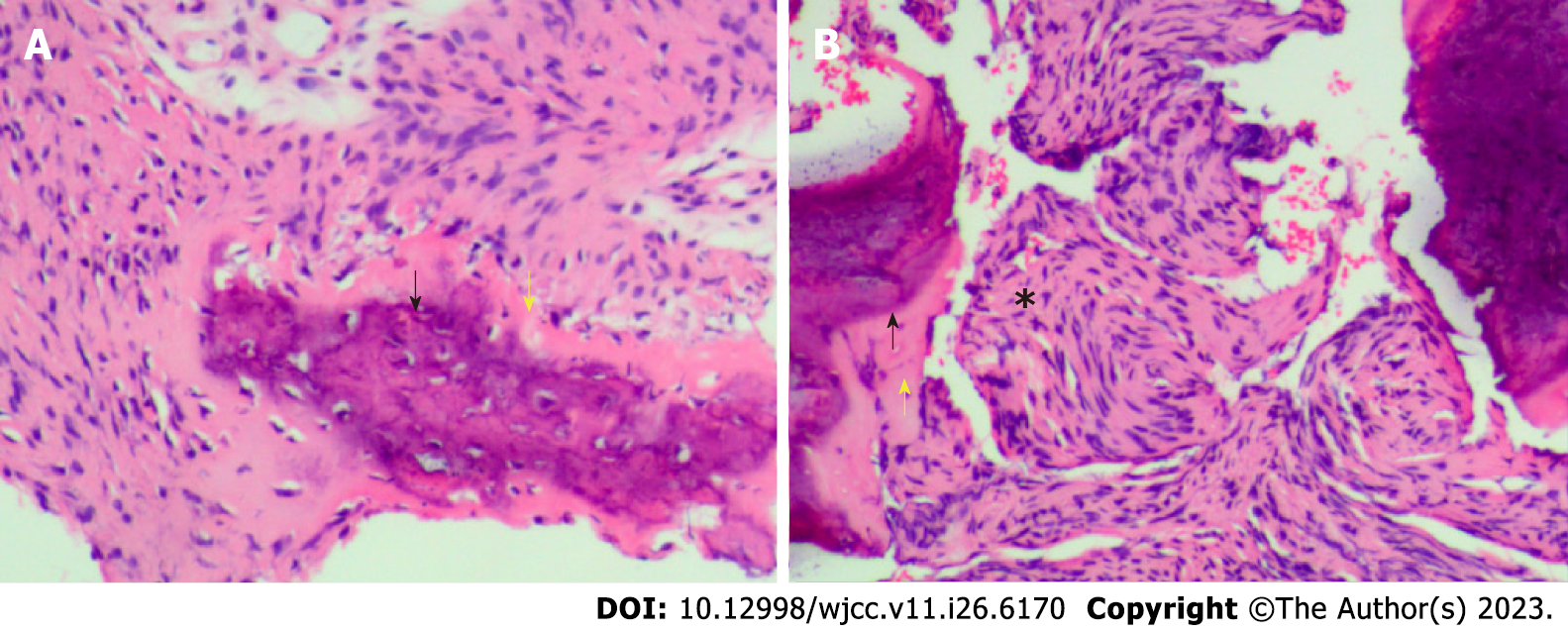
Pathological examination by preoperative puncture biopsy revealed fibrous dysplasia of the right proximal femur (Figure 2). The patient was diagnosed with fibrous dysplasia based on medical history, physical examination, and laboratory tests, imaging, and pathological examination. The patient was later diagnosed with fibrous dysplasia of the right proximal femur associated with ABC.
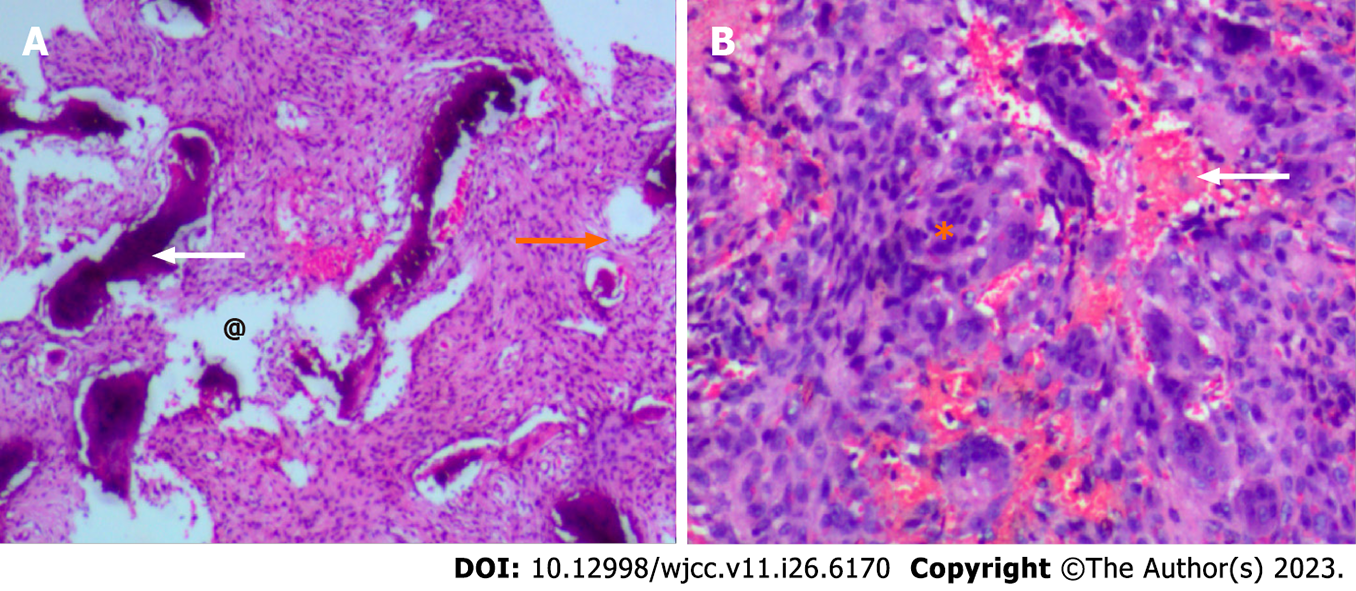
According to multidisciplinary expert consultation and professional discussion based on enhanced CT, MRI and primary pathological examination, the primary diagnosis and treatment methods were recommended to the patient. After communication with the patient, curettage and allograft, along with fixation with hip compression screws, were performed. The patient was placed in a supine position and a right straight lateral incision was made to expose the femoral neck, trochanter, and proximal femur. The femur was reached posteriorly from the vastus lateralis. A Kirschner wire was introduced in the fibrous dysplasia lesion under guidance of a C-arm by passing it through the lateral cortical bone from the center to the proximal border of the lesion. The drill and reamer were alternately used to create a tunnel for curettage of the defect. The local cortical bone at the surgical site was retained. The patient then underwent operation with curage of bone tumor tissue. Sterilized water was used to clean the cavity of the lesion. Under fluoroscopy, allograft and locking compression plate and hip screws were performed. An additional allogenic cancellous and cortical bone was inserted into the lesion to ensure adequate bone graft. The patient was encouraged to complete postoperative functional exercises in bed. After 1 mo, she was gradually mobilized using two crutches and partial weight-bearing. A gradual increase in weight-bearing was allowed after 6 wk based on evaluation by plain radiography that showed consolidation of the fixation and graft. Postoperative routine pathological examination revealed fibrous dysplasia associated with ABC-like changes of the right proximal femur (Figure 3).
After 6-months’ follow-up, the visual analog scale score was 1. Re-examination by plain radiography and CT showed no significant recurrence anywhere in the surgical site. No obvious allograft absorption or any loosening of fixation or secondary fracture were observed (Figure 4).
We reported a case of surgery for fibrous dysplasia of the right proximal femur associated with ABC. As a rare benign bone disease, fibrous dysplasia is usually caused by postzygotic, activating mutation of the GNAS gene[4]. In fibrous dysplasia, healthy bone is replaced by fibrous tissue produced by poor differentiation of osteoblasts, osteoclast activation, and local increase in bone turnover[5]. ABC is a true neoplasm that is neither an aneurysm nor a cyst[6]. As a benign pseudotumour-like lesions, ABC are composed of several expansive cystic compartments filled with blood derivatives, with few endothelial elements. The previous study has showed that in ABC there is a rearrangement of chromosomal bands 16q22 and 17p13, showing a deregulated expression of the USP6 genes[7]. They most commonly occur as primary lesions, and are very uncommon secondary to fibrous dyspepsia (FD). The above two bone diseases often affect children and young adults. There are no reports of fibrous dysplasia associated with ABC in young adults, although some studies have reported ABC-like changes associated with other bone neoplasms[3]. However, analogous clinical manifestations such as insidious onset of pain, deformities, and increased risk of fractures, may cause missed diagnosis and misdiagnosis of these, especially, as a concomitant disease for fibrous dysplasia or ABC. According to the 2020 World Health Organization classification of tumors of bone, there has been a shift in nomenclature, with the terms “ABC” and “ABC-like changes” replacing “primary ABC” and “secondary ABC”[8]. Benign tumors associated with aneurysmal changes reminiscent of ABC include chondroblastoma, fibrous dysplasia, giant cell tumor, osteoblastoma, and nonossifying fibroma[9]. The most common tumors associated with ABC-like changes are giant cell tumor and chondroblastoma[3,9]. Our case was diagnosed as fibrous dysplasia based on primary pathological results associated with medical history, physical and laboratory examination, and imaging. The patient was finally diagnosed with fibrous dysplasia of the right proximal femur associated with ABC-like changes.
With regard to therapy of fibrous dysplasia or ABC, curettage and bone grafting, with or without internal fixation, have been the mainstay for symptomatic and even asymptomatic lesions of fibrous dysplasia. In the literature reviewed with simultaneous presentation of FD and ABC. At present, the use of cancellous or cortical bone graft in addition to corrective osteotomy is still controversial[10]. The traditional therapeutic options for ABC have been intralesional curettage with or without bone grafting. At present, adjuncts including liquid nitrogen, phenol, argon laser, bone grafting or bone substitution, and sclerotherapy are used to enhance therapeutic efficacy. Our case was treated with curettage and allograft, associated with fixation with hip compression screws. Osteotomy and stabilization with a peripheral plate are usually used for isolated coxa vara, but multiple osteotomies and stabilization by cericodiaphyseal intramedullary nailing are used for treatment of isolated shepherd’s crook deformity in patients with fibrous dysplasia. Two-stage surgery is used for coxa vara associated with shepherd’s crook deformity[10].
Fibrous dysplasia associated with ABC-like changes in the proximal femur is rare and accurate diagnosis is important. The allograft and locking compression plate and hip screws are suitable therapeutic methods. After treatment, active follow-up and regular reviews should be also carried out.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hoveidaei AH, Iran S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Theng EH, German A, Pan KS, Isaac S, Boyce AM, Collins MT. Periorbital inflammation associated with craniofacial fibrous dysplasia: Report of three cases and review of the literature. Bone. 2021;153:116157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Florenzano P, Pan KS, Brown SM, Paul SM, Kushner H, Guthrie LC, de Castro LF, Collins MT, Boyce AM. Age-Related Changes and Effects of Bisphosphonates on Bone Turnover and Disease Progression in Fibrous Dysplasia of Bone. J Bone Miner Res. 2019;34:653-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 3. | Restrepo R, Zahrah D, Pelaez L, Temple HT, Murakami JW. Update on aneurysmal bone cyst: pathophysiology, histology, imaging and treatment. Pediatr Radiol. 2022;52:1601-1614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 53] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 4. | Nishida Y, Tsukushi S, Hosono K, Nakashima H, Yamada Y, Urakawa H, Ishiguro N. Surgical treatment for fibrous dysplasia of femoral neck with mild but prolonged symptoms: a case series. J Orthop Surg Res. 2015;10:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Duan C, Dai Q, Liu Q, Yu H. Characteristics of sinonasal fibrous dysplasia: experience from a single department. Acta Otolaryngol. 2018;138:50-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015;101:S119-S127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 154] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 7. | Burdiles A, Marín R, Klaber I, Solar A, Calderón M, Jara F, Kara F, Bazáes D. Polyostotic fibrous dysplasia (McCune-Albright) with rare multiple epiphyseal lesions in association with aneurysmal bone cyst and pathologic fracture. Radiol Case Rep. 2021;16:2719-2725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 8. | Choi JH, Ro JY. The 2020 WHO Classification of Tumors of Bone: An Updated Review. Adv Anat Pathol. 2021;28:119-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 188] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 9. | Matsuhashi A, Yoshimoto T, Yoshikawa G. Solitary fibrous tumor with aneurysmal bone cyst-like change in the middle cranial fossa: illustrative case. J Neurosurg Case Lessons. 2022;4:CASE22271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Yung D, Kikuta K, Sekita T, Asano N, Nakayama R, Nakamura M, Matsumoto M. Conservative surgical management of simple monostotic fibrous dysplasia of the proximal femur in a 19-year-old basketballer: a case report. J Med Case Rep. 2018;12:240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |