Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6165
Peer-review started: April 13, 2023
First decision: July 6, 2023
Revised: July 31, 2023
Accepted: August 11, 2023
Article in press: August 11, 2023
Published online: September 16, 2023
Processing time: 148 Days and 6.1 Hours
Left atrial flutter without prior cardiac interventions is uncommon, especially dual-loop macro-reentry atrial flutter. The critical step to ablate dual-loop macro-reentry atrial flutter is to identify the dominant loop and key isthmus. Although entrainment mapping could help identify the dominant loop and key isthmus, it may alter or terminate tachycardia. High-density mapping allows the generation of electroanatomic maps without altering or terminating tachycardia.
Here, we report a case of symptomatic left atrial flutter without prior intervention. In this case, high-density mapping revealed a dual-loop macro-reentry around the mitral annulus and central scar of the anterior wall. The propagation result showed that the dominant loop was around the mitral annulus, and the key isthmus was between the central scar and mitral annulus. The atrial flutter terminated successfully after ablation was performed.
In this case, we demonstrate that high-density mapping technology may help identify the dominant loop of dual-loop atrial flutter without entrainment, which makes ablation easier.
Core Tip: Identification of the dominant loop of a dual-loop macro-reentry left atrial flutter without prior intervention using high-density mapping technology without entrainment.
- Citation: Yu SD, Chu YP. Identification of the dominant loop of a dual-loop macro-reentry left atrial flutter without prior intervention using high-density mapping technology: A case report. World J Clin Cases 2023; 11(26): 6165-6169
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6165.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6165
Sustained left atrial flutter is common in patients with prior cardiac interventions. However, there are few patients presenting left atrial flutter without prior cardiac interventions. Several studies have reported that the incidence of this type of atrial flutter among patients suffering from left atrial flutter undergoing radiofrequency ablation is relatively low, among 4.4%-6.7%[1,2]. There is a subgroup of patients presenting with dual-loop macro-reentry atrial flutter. The incidence of dual-loop macro-reentry is even lower. The accurate identification of the dominant loop and key isthmus is important for ablation. Entrainment mapping can provide guidance for the identification of the dominant loop and key isthmus. However, tachycardia may be altered or terminated. The utilization of high-density mapping technology allows for the detailed characterization of atrial arrhythmias without altering or terminating tachycardia, which may help electrophysiologists determine the mechanisms involved in tachycardia. Here, we report a case using high-density mapping technology to identify the dominant loop of dual-loop macro-reentry left atrial flutter without prior cardiac intervention.
A 79-year-old female presented to the emergency department because of palpitations.
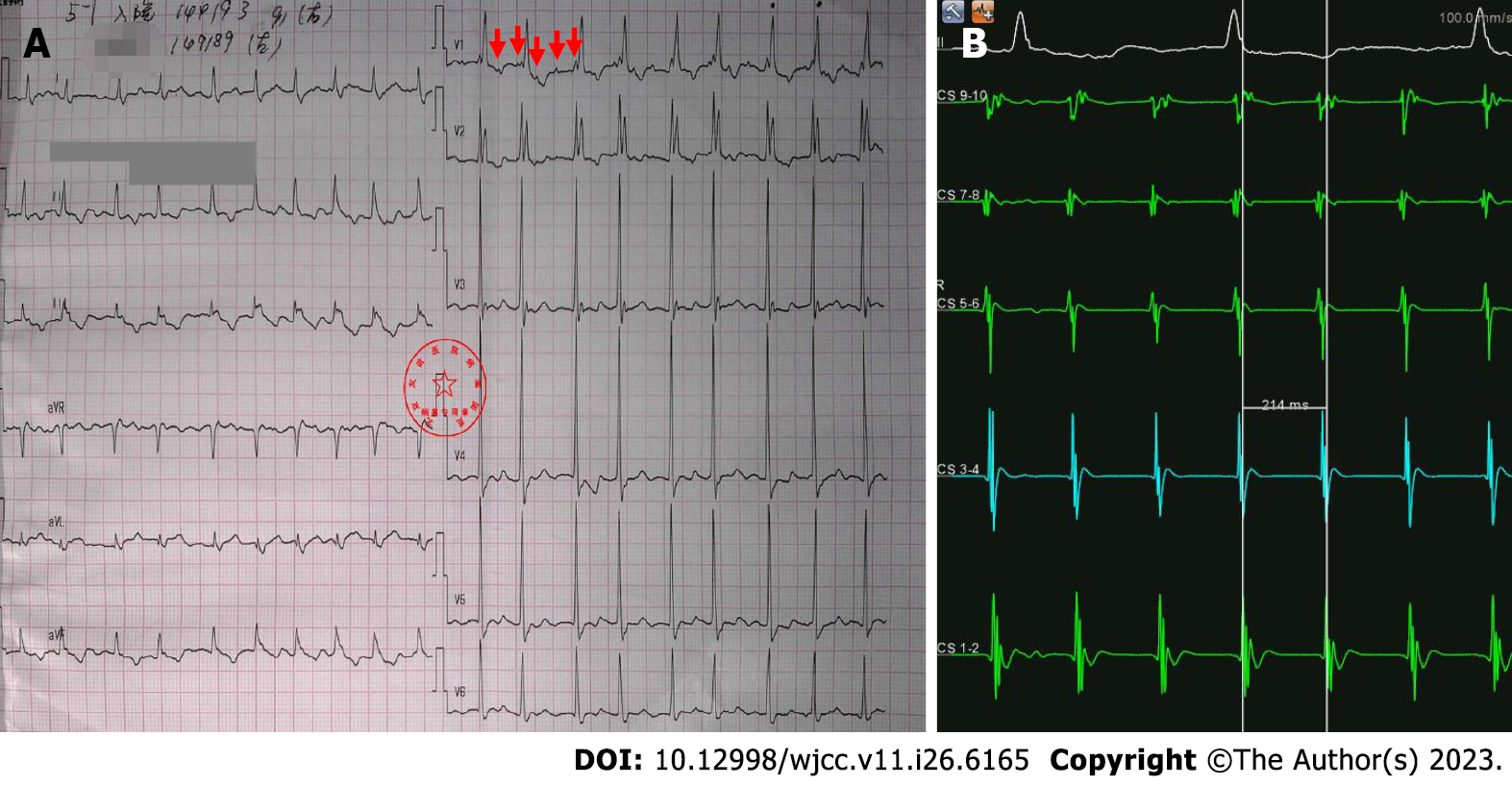
The baseline electrocardiogram showed a narrow QRS complex tachycardia with regular PP intervals and complete right bundle branch block (Figure 1A).
The past illness are coronary heart disease, hypertension, and hyperlipidemia.
Hypertension.
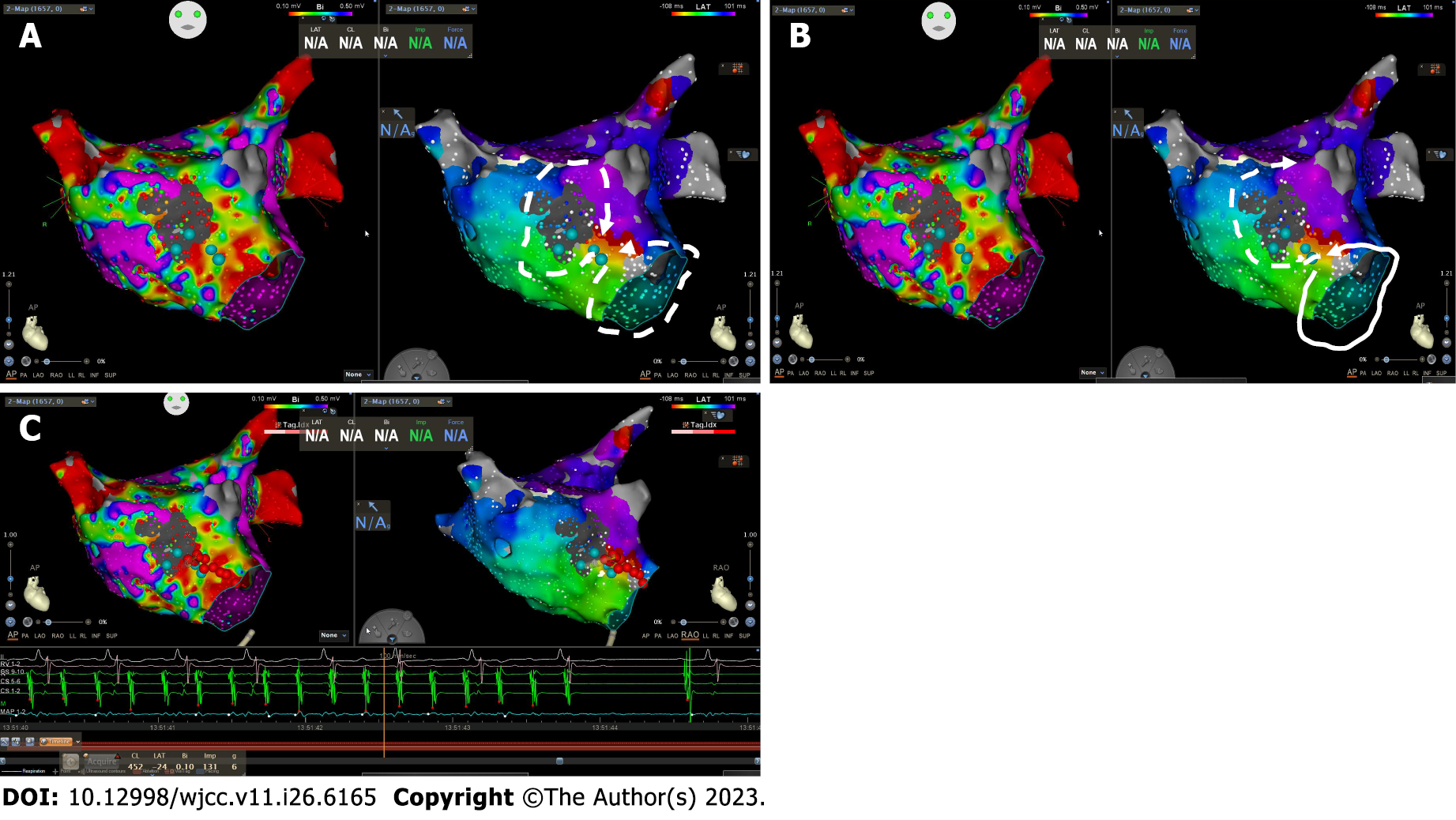
An echocardiogram showed an enlarged left atrium. Coronary angiography showed left anterior descending branch stenosis in 60% of patients. An electrophysiological study was performed after exclusion of contraindications. Intracardiac electrocardiogram of the coronary sinus showed that the cycle length of tachycardia was 214 ms (Figure 1B). Activation mapping of the right atrium by using an 8F, 3.5 mm irrigated-tip catheter ThermoCool© SmartTouch© Surround Flow catheter and Carto 3 system (Biosense Webster, Inc., Diamond Bar, CA, United States) showed the earliest activation site in the septum with a local activation time of 70 ms. Then, high-density mapping was performed in the left atrium after atrial septal puncture by using the Pentary and Carto 3 system. The voltage mapping revealed a high proportion of low voltage zones (< 0.5 mV) in the anterior wall and scars (no potential area) in the center of the anterior wall (Figure 2A). Activation mapping showed dual-loop macro-reentry around the mitral annulus and the central scar of the anterior wall (Figure 2A). The common channel was located between the central scar and mitral annulus. Propagation results showed that the wavefront of the mitral annulus loop entered the common conducting channel earlier (Supplementary material). According to the mapping results, we considered the loop around the mitral annulus to be the dominant loop (Figure 2B).
The patient was diagnosed as dual-loop left atrial flutter.
Because the lateral mitral isthmus is hard to block and may introduce arrhythmogenic channels, we designed an ablation line between the central scar and mitral annulus. Ablation was performed in power-controlled mode at 45 W and an ablation index of 450 by using an 8F, 3.5 mm irrigated-tip catheter ThermoCool© SmartTouch© Surround Flow catheter.
The atrial flutter terminated while ablation was performed (Figure 2C). During the 1-year follow-up, the patient did not report any symptoms without antiarrhythmic drugs, and there was no electrocardiogram evidence of tachycardia.
The incidence of left atrial flutter without prior cardiac intervention is fairly low. Several studies reported that the incidence of dual-loop macro-reentry around the mitral annulus and the central scar of the anterior wall was even lower, between 0.9%-3.1%[1]. Some researchers reported that the left atrial anterior wall low voltage zone was more frequent in perimitral atrial flutter without prior intervention. The anterior wall low voltage zone has a significant correlation with the left atrial-aorta contact area[2]. The left atrial-aorta aera is thinner than other areas of the left atrium, and scarring is more frequent in this area[3]. This area is more frequently an arrhythmogenic substrate for perimitral atrial flutter without prior intervention. The mitral isthmus may be only an anatomic isthmus, not an arrhythmogenic substrate[2]. Before ablation of dual-loop macro-reentry atrial flutter, the critical step is to identify the dominant loop and key isthmus. Entrainment is widely used to identify the dominant loop and key isthmus. However, it may terminate or alter tachycardia[4]. High-density mapping may help electrophysiologists determine the mechanisms involved in tachycardia. Schaeffer et al[1] reported a group of patients with nonfocal left atrial tachycardia without previous iatrogenic interventions. Voltage mapping showed there were low voltage areas (LVAs) in left atrial of these patients. These LVAs were arrhythmogenic, especially anterior wall LVA. Therefore, voltage mapping may give us some implications on reentry circuit through showing LVAs. In this case, voltage mapping indicated that there was a central scar in the anterior wall, and activation mapping revealed two reentry loops and common channels. Propagation results showed that the wavefront of the mitral annulus loop entered the common channel earlier than the anterior loop. Based on these results, we determined the dominant loop and key isthmus without entrainment mapping. The choice of a lesion set for ablating atrial flutter depends on a number of factors, including the length of the isthmus, catheter stability in that region, electroanatomical characteristics and potential complications[5]. Moreover, high-power (45-50 W) short-duration radiofrequency ablation can produce lesions from resistive heating rather than conductive heating, which may block the isthmus more easily[6]. In the present case, the lateral mitral isthmus might have required extensive ablation because of epicardial connections, but the anterior isthmus was short, easy to ablate and relatively safe.
In this case, we demonstrate that high-density mapping technology may help identify the dominant loop of dual-loop atrial flutter without entrainment, which makes ablation easier.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Conti S, Italy S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Schaeffer B, Akbulak RÖ, Jularic M, Moser J, Eickholt C, Schwarzl JM, Klatt N, Kuklik P, Meyer C, Willems S. High-Density Mapping and Ablation of Primary Nonfocal Left Atrial Tachycardia: Characterizing a Distinct Arrhythmogenic Substrate. JACC Clin Electrophysiol. 2019;5:417-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Fukamizu S, Sakurada H, Hayashi T, Hojo R, Komiyama K, Tanabe Y, Tejima T, Nishizaki M, Kobayashi Y, Hiraoka M. Macroreentrant atrial tachycardia in patients without previous atrial surgery or catheter ablation: clinical and electrophysiological characteristics of scar-related left atrial anterior wall reentry. J Cardiovasc Electrophysiol. 2013;24:404-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Yu J, Chen K, Yang B, Zhang F, Ju W, Chen H, Yang G, Li M, Wang B, Gu K, Ouyang F, Ho SY, Po S, Chen M. Peri-mitral atrial flutter: personalized ablation strategy based on arrhythmogenic substrate. Europace. 2018;20:835-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Ho SY, Sanchez-Quintana D, Cabrera JA, Anderson RH. Anatomy of the left atrium: implications for radiofrequency ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 1999;10:1525-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 288] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 5. | Latcu DG, Squara F, Massaad Y, Bun SS, Saoudi N, Marchlinski FE. Electroanatomic characteristics of the mitral isthmus associated with successful mitral isthmus ablation. Europace. 2016;18:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Markowitz SM, Thomas G, Liu CF, Cheung JW, Ip JE, Lerman BB. Approach to catheter ablation of left atrial flutters. J Cardiovasc Electrophysiol. 2019;30:3057-3067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |