Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.6005
Peer-review started: July 4, 2023
First decision: July 18, 2023
Revised: July 26, 2023
Accepted: July 31, 2023
Article in press: July 31, 2023
Published online: September 6, 2023
Processing time: 59 Days and 6.8 Hours
A carotid-cavernous fistula (CCF) is an abnormal connection between the internal carotid artery (ICA) and the cavernous sinus. Although direct CCFs typically result from trauma or as an iatrogenic complication of neuroendovascular procedures, they can occur as surgery-related complications after mechanical thrombectomy (MT). With the widespread use of MT in patients with acute ischemic stroke complicated with large vessel occlusion, it is important to document CCF following MT and how to avoid them. In this study, we present a case of a patient who developed a CCF following MT and describe in detail the characteristics of ICA tortuosity in this case.
A 60-year-old woman experienced weakness in the left upper and lower limbs as well as difficulty speaking for 4 h. The neurological examination revealed left central facial paralysis and left hemiplegia, with a National Institutes of Health Stroke Scale score of 9. Head magnetic resonance imaging revealed an acute cerebral infarction in the right basal ganglia and radial crown. Magnetic resonance angiography demonstrated an occlusion of the right ICA and middle cerebral artery. Digital subtraction angiography demonstrated distal occlusion of the cervical segment of the right ICA. We performed suction combined with stent thrombectomy. Then, postoperative angiography was performed, which showed a right CCF. One month later, CCF embolization was performed, and the patient’s clinical symptoms have significantly improved 5 mo after the operation.
Although a CCF is a rare complication after MT, it should be considered. Understanding the tortuosity of the internal carotid-cavernous sinus may help predict the complexity of MT and avoid this complication.
Core Tip: The occurrence of carotid-cavernous fistula (CCF) after mechanical thrombectomy (MT) is rare, with only five cases reported in PubMed. Herein we report a rare case of CCF occurring after MT in a patient with acute ischemic stroke. This paper describes the tortuosity of the cavernous internal carotid artery (ICA). We believe that future analysis of ICA tortuosity will help evaluate the complexity of the surgery and better predict and avoid CCF and other complications.
- Citation: Qu LZ, Dong GH, Zhu EB, Lin MQ, Liu GL, Guan HJ. Carotid-cavernous fistula following mechanical thrombectomy of the tortuous internal carotid artery: A case report. World J Clin Cases 2023; 11(25): 6005-6011
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/6005.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.6005
Carotid-cavernous fistula (CCF) is an abnormal connection between arteries and veins of the coronary sinus[1]. The symptoms include headache, nerve palsy and ocular symptoms, which lead to visual impairment, blindness, cerebral infarction and even intracranial haemorrhage[1,2]. Head trauma, ruptured aneurysm and idiopathic CCF represent the main causes of direct CCF[1]. The incidence of iatrogenic CCF in interventional radiology is approximately 0.8%; this includes its occurrence as a complication during neurointerventional procedures, including coil embolization of aneu
Speech impairment with weakness of the left upper and lower limbs for 4 h.
A 60-year-old female patient presented with poor speech and left upper and lower limbs movement for the last 4 h. The left upper limb could be lifted off the bed surface but with no resistance. The left lower limb could do moderate resistance. Further symptoms included lethargy, slurred speech, a drinking cough and no incontinence. Before coming to our hospital, a head CT was performed in a subordinate hospital with no sign of cerebral hemorrhage. She was then immediately transferred to our hospital.
The patient’s medical history included cerebral infarction and coronary heart disease. She had no history of hypertension, diabetes or hyperlipidemia.
The personal history included smoking twenty cigarettes daily for 40 years. Otherwise no further contributing factors in the remaining personal and family history.
Physical examination on admission: Lethargy, dysarthria, eye deviation to the right, partial facial paralysis left, left upper limb muscle strength level III, left lower limb muscle strength level IV, no pathological reflex. The National Institutes of Health Stroke Scale (NIHSS) score was 9 points (1 point for consciousness, 1 point for gazing, 2 points for dysarthria, 2 points for partial facial paralysis, and 3 points for left limb weakness). The modified Rankin Scale (mRS) score was 4.
The laboratory findings were within the normal range, glucose was 5.85 mmol/L, triglyceride was 1.66 mmol/L, with the exception of the low density lipoprotein cholesterol level measuring 4.3 mmol/L, higher than normal.
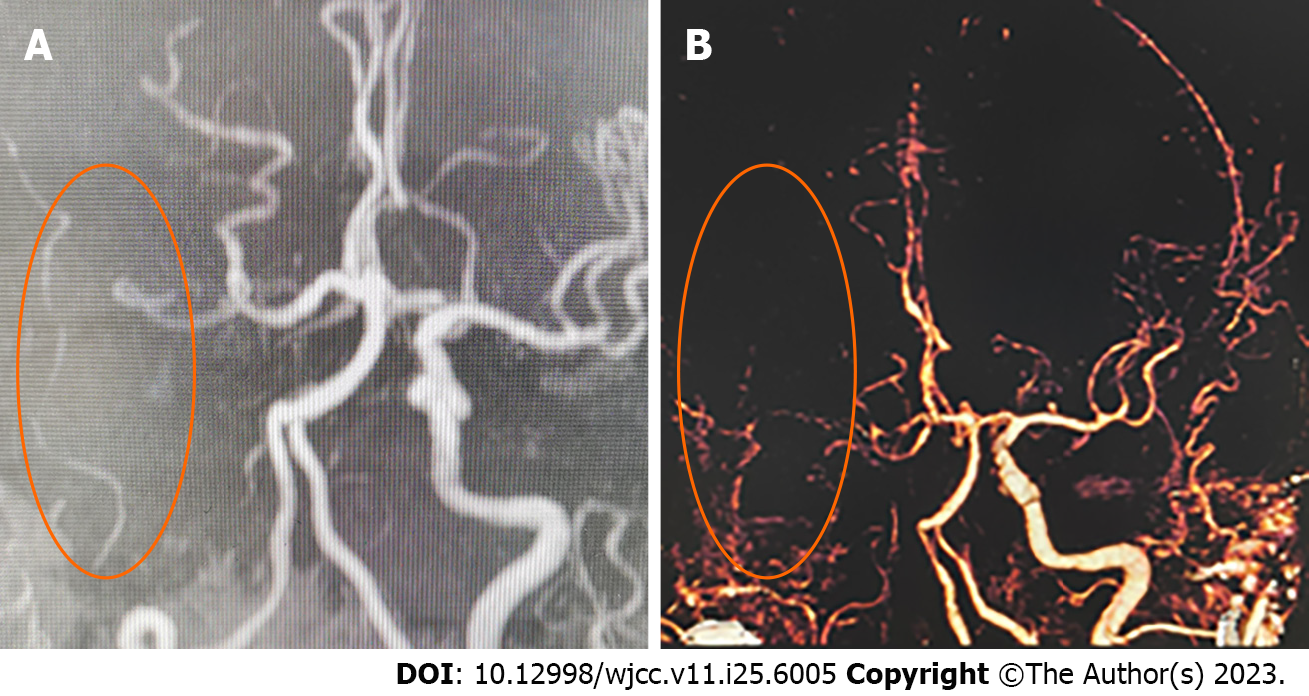
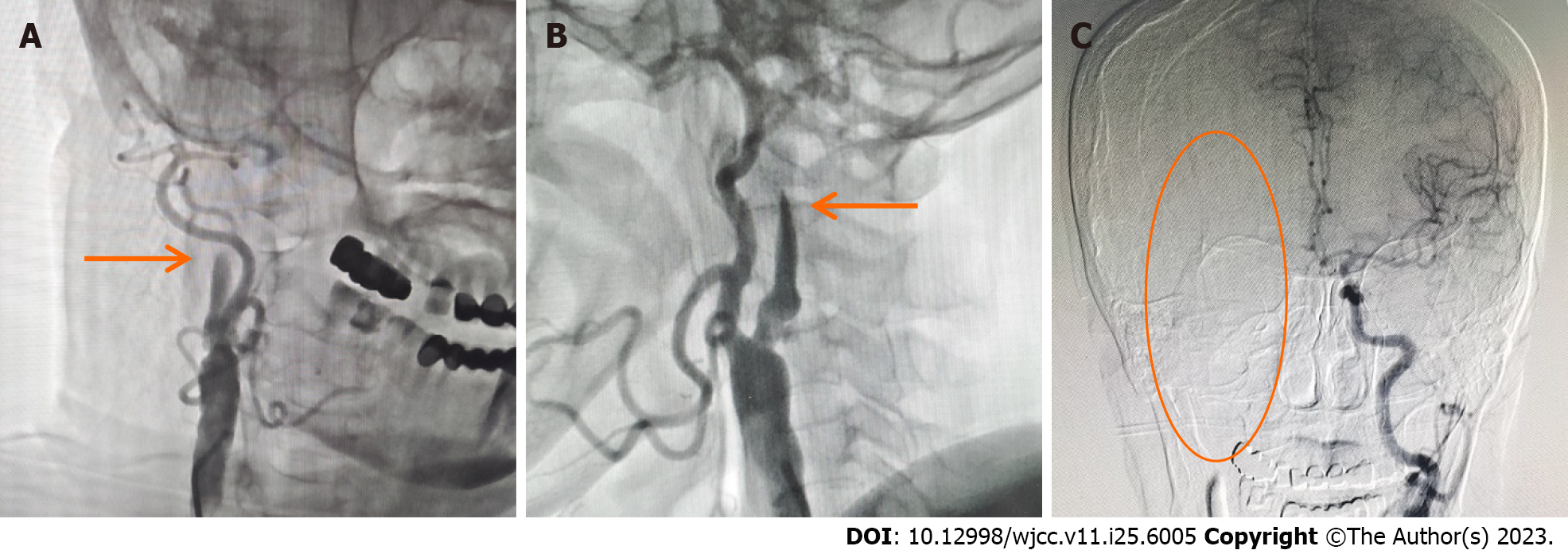
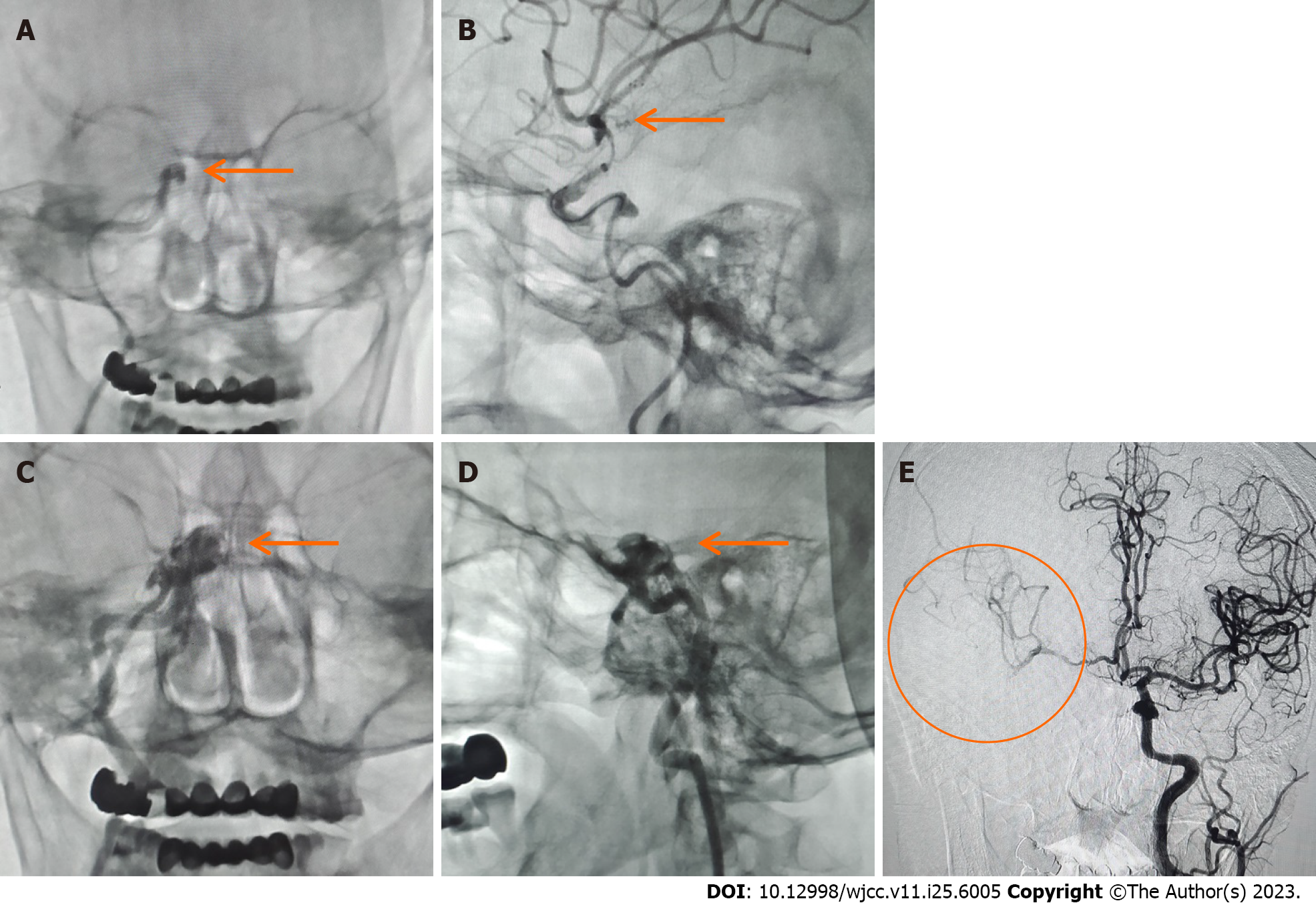
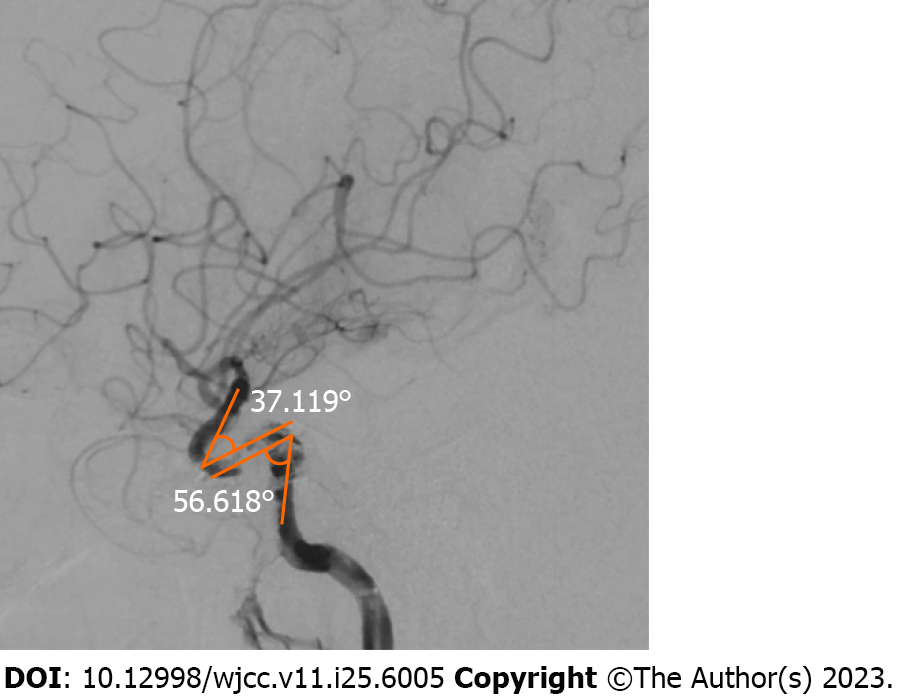
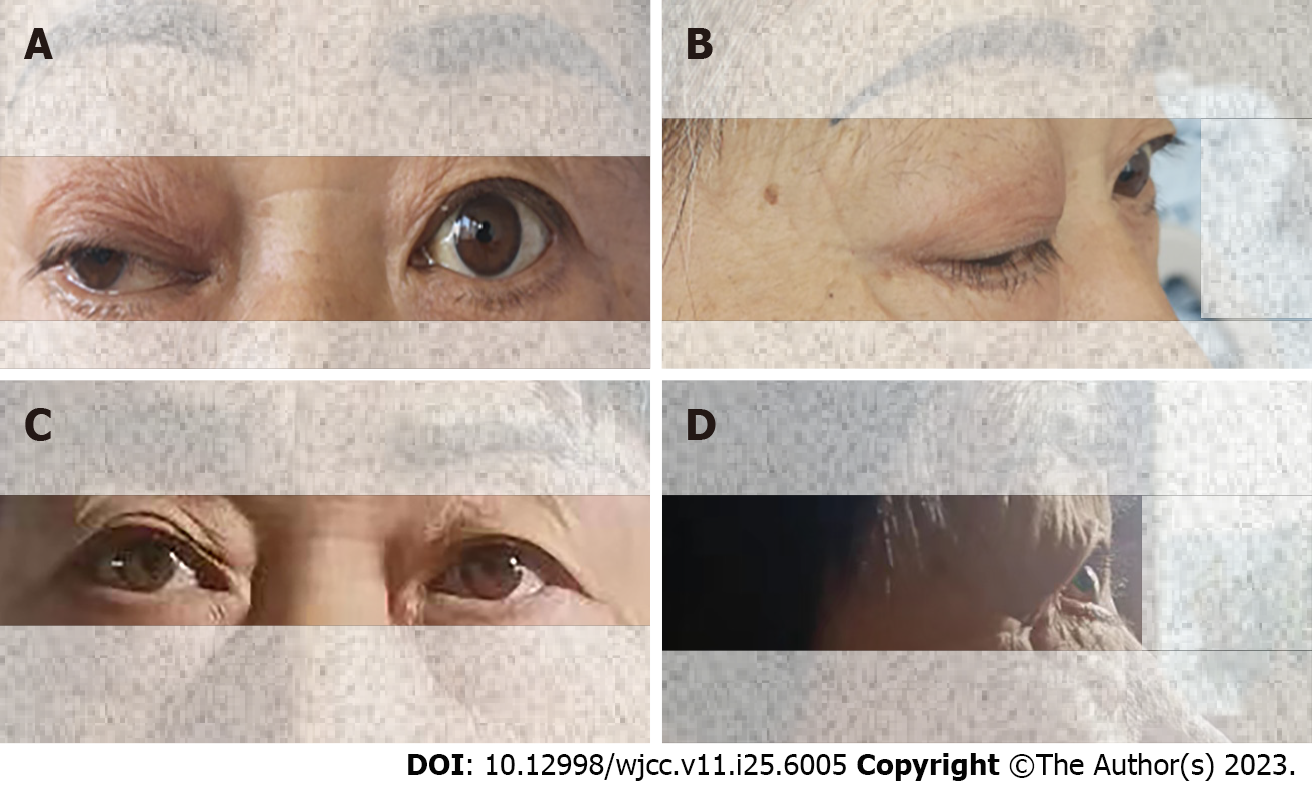
The result of magnetic resonance angiography and computed tomography angiography indicated the presence of occlusion in both the right ICA and middle cerebral artery (MCA) (Figure 1). MT was required. Digital subtraction angiography (DSA) demonstrated distal occlusion of the right ICA (Figure 2A and B). The A1 segment of the right anterior cerebral artery (ACA) was not developed, and there was no compensatory flow to the right MCA (Figure 2C). After performing the aspiration thrombectomy, the DSA showed occlusion of the terminal bifurcation of the right ICA (Figure 3A). After the first stent removal, the angiography showed poor right MCA reflow and no CCF (Figure 3B). After the second stent retriever thrombectomy, the DSA showed a right CCF (Figure 3C and D). The A1 segment of the right ACA was developed to supply blood to the supply area of the right MCA (Figure 3E). Cavernous ICA tortuosity was observed, with the acute angle of the anterior genu being 37.119°, and that of the posterior genu being 56.618° (Figure 4). Figure 5A and B show the clinical manifestations of the patient before the preoperative internal carotid-cavernous sinus embolization. After five months follow-up, the patient’s clinical symptoms were relieved (Figure 5C and D).
Carotid thrombosis complicated with intracranial arterial embolism; MT-caused right CCF.
The patient received aspiration thrombectomy with stent retriever thrombectomy. One month after thrombus removal, the patient underwent CCF embolization.
After 5 mo follow-up, the patient’s clinical symptoms showed significant improvement with no new stroke events. At 24 h after MT, the patient’s NIHSS score was 6, 1 mo after MT the patient’s NIHSS score was 2. After 5 mo follow-up, the patient’s NIHSS score was 1 and mRS score was 1. No exacerbation of the symptoms, no complications and no recorded adverse events. The patient expressed satisfaction with the treatment and is now able to resume their normal life. The patient’s clinical symptoms were significantly relieved and he was actively rehabilitated.
The present report documents a CCF that occurred after MT of the tortuous ICA. To the best of our knowledge, CCF following MT is an uncommon event[4]. A case of CCF caused by vessel injury during the withdrawal of a stent retriever during MT for acute ischemic stroke (AIS) was reported by Matsumoto et al[5], where it was suggested that the key mechanism contributing to the pull-out vessel injury was the mechanical stretching of the vessel while withdrawing the stent retriever due to vessel tortuosity. This was probably caused by pull-out vessel injury of the meningohypophyseal trunk branching from the cavernous segment of the ICA. The study of Miyamoto et al[3] reported that direct CCF is caused by ICA perforation by a microcatheter body during MT. Our case report suggests that the tortuosity of the ICA could be a potential predisposing factor for iatrogenic CCF[4]. In this case, the initial angiography showed distal occlusion of the right ICA at the beginning, stenosis of the patient’s proximal vessels, unclear distal vascular conditions and a large number of load thrombi, resulting in an unclear path and a significant increase in the risk of CCF. Meanwhile, the tortuous ICA would reduce the surgeon’s control level of the microcatheter or micro guide wire[6]. Hence, we considered that the CCF might have resulted from not performing a gentle manipulation by the operator. The tortuosity of the ICA leads to an increased risk of inadvertently damaging the apex in case of mistakenly inserting a guide wire[7]. Consequently, it is imperative for the neurointerventionist to proceed with caution and gentleness throughout the procedure.
Proptosis frequently manifests as a symptom of CCF. The CCF-associated symptoms are influenced by the direction of the venous drainage, speed of blood flow through the shunts and a thrombosis-caused obstruction of the venous outflow. Therefore, a range of clinical manifestations may arise, including but not limited to headache, nerve dysfunction and ocular symptoms. Amidst these symptoms, the most dreaded complications are visual impairment, blindness and intracranial haemorrhages[4]. Despite the growing use of MT in the treatment of AIS, limited cases of resulting CCF have been reported. Furthermore, CCFs due to the high curvature of the ICA are even rarer.
Unlike previously reported cases, a focal point in our report is the curvature of the ICA. Given that the ICA is the exclusive pathway to the anterior circulation, its curvature represents an important challenge when performing MT. ICA tortuosity can be categorized into four types based on the geometry of the anterior and posterior curves. Type I ICA tortuosity is characterized by an open configuration or angle, with two subclasses: IA when the angle of the posterior knee is greater than 90°, and IB when the angle is equal to 90°. Type II is characterized by a closed anterior knee configuration with a sharper knee angle compared with Type I. Type III is defined as having the back knee angled backward, and Type IV ICA tortuosity exhibits a highly curved appearance, resembling the shape of a Simmons angiogram catheter. In this type, the posterior knee is curved upwards in comparison with the front knee, making it the most tortuous form of ICA tortuosity. Type I (A or B) represents mild tortuosity, Type II-III represents moderate tortuosity, and Type IV represents severe tortuosity[8,9]. In our case, as shown in Figure 4, this patient has a cavernous ICA tortuosity of type III, which is moderate tortuosity.
According to the study conducted by Ono et al[7], 89% of the reported CCFs occurred specifically at the genu (bend) of the cavernous ICA. This can be explained by the increased likelihood of direct perforation by the guidewire or distal access catheter at the curved portion of the ICA. A previous report[10] presented two cases of perforation during catheter navigation, the fistulas were located at the posterior part of the cavernous ICA. It was suggested that this occurrence might be attributed to the acutely angled vasculature in this particular region. Some evidence suggests that vascular tortuosity could depend on connective tissue alterations that weaken the structure of the nasal wall, making it more susceptible to dissection. In this regard, it could be considered a “visual marker” of vassal fragility[11]. Compared with straight arteries, tortuous arteries have a higher likelihood of vasospasm occurring during the passage of balloons, catheters, embolic protection devices and stents. This is due to the increased potential for collisions between these devices and the arterial wall. The presence of tortuosity is challenging during the procedure, typically involving repeated and prolonged mechanical stimulation to the arterial wall. This direct stimulation can induce vasospasm, which might have detrimental effects[12]. The tortuosity of the ICA can impede the advancement of intermediate catheters, microcatheters and retrievers, ultimately diminishing the effectiveness of proximal aspiration and reducing the likelihood of a successful embolectomy[13,14]. Consequently, this can negatively affect vessel recanalization and overall treatment outcome[15].
Complications after MT lead to increased length of stay in intensive care and stroke units, increasing the costs and delaying the commencement of rehabilitation[16]. Iatrogenic CCFs are a subset of traumatic fistulae that may occur during endovascular procedures[17]. With the increasing frequency of MTs performed for AIS, neuro-interventionalists should be aware of this potential rare complication. In future surgery, predicting the curvature of ICA can help to choose a better operation mode. However, in the case of emergency thrombectomy, the curvature of the ICA is mostly unpredictable. Specifically, in patients with ICA occlusion, by understanding the curvature grading of the cavernous sinus segment, the catheter and guidewire could be operated more gently and cautiously when passing through the cavernous sinus segment and stenting for embolization during future cerebral angiography and MT. Hence, the possibility of severe curvature of ICA should be considered. Caution and prudence of the neurointerventionist while performing the procedure can ensure a discreet approach, thereby minimizing the risk of CCF.
Although limited cases of CCF during neurointerventional radiology have been reported, it is anticipated that the number of cases will increase due to the significant rise in MT procedures following AIS. It is important to avoid iatrogenic direct CCF complications, especially that the degree of curvature of the carotid cavernous segment is mostly unknown at the time of MT with ICA occlusion. Therefore, it is advisable for the neurointerventionist to adopt a gentle and cautious approach during the procedure.
We would like to thank the patient and her family for their informed cooperation and support in our work.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ng ZQ, Australia; Yarmahmoodi F, Iran S-Editor: Lin C L-Editor: A P-Editor: Yuan YY
| 1. | Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye (Lond). 2018;32:164-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 155] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 2. | Sheinberg DL, Brunet MC, Chen SH, Luther E, Starke RM. Iatrogenic Direct Carotid-cavernous Fistula Following Mechanical Thrombectomy: A Case Report and Review of the Literature. Cureus. 2020;12:e7524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Miyamoto S, Kato N, Yamazaki T, Yamano A, Akutsu Y, Yasuda S, Matsumaru Y, Ishikawa E. Direct Carotid-Cavernous Fistula Caused by Internal Carotid Artery Perforation by a Microcatheter Body during Mechanical Thrombectomy. Asian J Neurosurg. 2022;17:638-641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Grüter BE, Kahles T, Anon J, Berberat J, Andereggen L, Killer HE, Gruber P. Carotid-cavernous sinus fistula following mechanical thrombectomy in acute ischaemic stroke: a rare complication. Neuroradiology. 2021;63:1149-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Matsumoto H, Nishiyama H, Takemoto H, Tetsuo Y, Nakao N. Carotid-cavernous Fistula Caused by Vessel Injury While Withdrawing a Stent Retriever during Mechanical Thrombectomy for Acute Ischemic Stroke: A Case Report. J Neuroendovascular Ther. 2018;12:235-240. [DOI] [Full Text] |
| 6. | Ihn YK, Shin SH, Baik SK, Choi IS. Complications of endovascular treatment for intracranial aneurysms: Management and prevention. Interv Neuroradiol. 2018;24:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 7. | Ono K, Oishi H, Tanoue S, Hasegawa H, Yoshida K, Yamamoto M, Arai H. Direct carotid-cavernous fistulas occurring during neurointerventional procedures. Interv Neuroradiol. 2016;22:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Koge J, Tanaka K, Yoshimoto T, Shiozawa M, Kushi Y, Ohta T, Satow T, Kataoka H, Ihara M, Koga M, Isobe N, Toyoda K. Internal Carotid Artery Tortuosity: Impact on Mechanical Thrombectomy. Stroke. 2022;53:2458-2467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 9. | Lin LM, Colby GP, Jiang B, Uwandu C, Huang J, Tamargo RJ, Coon AL. Classification of cavernous internal carotid artery tortuosity: a predictor of procedural complexity in Pipeline embolization. J Neurointerv Surg. 2015;7:628-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Kwon HJ, Jin SC. Spontaneous healing of iatrogenic direct carotid cavernous fistula. Interv Neuroradiol. 2012;18:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Venturini G, Vuolo L, Pracucci G, Picchioni A, Failli Y, Benvenuti F, Sarti C. Association between carotid artery dissection and vascular tortuosity: a case-control study. Neuroradiology. 2022;64:1127-1134. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Wang Q, Liu C, Yan B, Fan X, Zhang M, Li Y, Zhu W, Chen M, Huang X, Zhang Z, Xu G, Liu X. Correlation of extracranial internal carotid artery tortuosity index and intraprocedural complications during carotid artery stenting. Eur Neurol. 2012;68:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Kaymaz ZO, Nikoubashman O, Brockmann MA, Wiesmann M, Brockmann C. Influence of carotid tortuosity on internal carotid artery access time in the treatment of acute ischemic stroke. Interv Neuroradiol. 2017;23:583-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Snelling BM, Sur S, Shah SS, Chen S, Menaker SA, McCarthy DJ, Yavagal DR, Peterson EC, Starke RM. Unfavorable Vascular Anatomy Is Associated with Increased Revascularization Time and Worse Outcome in Anterior Circulation Thrombectomy. World Neurosurg. 2018;120:e976-e983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Leker RR, Kasner SE, El Hasan HA, Sacagiu T, Honig A, Gomori JM, Guan S, Choudhry O, Hurst RW, Kung D, Pukenas B, Sedora-Roman N, Ramchand P, Cohen JE. Impact of carotid tortuosity on outcome after endovascular thrombectomy. Neurol Sci. 2021;42:2347-2351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Balami JS, White PM, McMeekin PJ, Ford GA, Buchan AM. Complications of endovascular treatment for acute ischemic stroke: Prevention and management. Int J Stroke. 2018;13:348-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 182] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 17. | Alan N, Nwachuku E, Jovin TJ, Jankowitz BT, Jadhav AP, Ducruet AF. Management of Iatrogenic Direct Carotid Cavernous Fistula Occurring During Endovascular Treatment of Stroke. World Neurosurg. 2017;100:710.e15-710.e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |