Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5994
Peer-review started: May 31, 2023
First decision: July 19, 2023
Revised: July 28, 2023
Accepted: August 8, 2023
Article in press: August 8, 2023
Published online: September 6, 2023
Processing time: 93 Days and 1.6 Hours
Renal cell carcinoma (RCC) is the third most common malignancy in the genitourinary tract. The lungs, bone, lymph nodes, liver, and brain are common metastatic sites of RCC. However, there is limited literature on single omental metastasis of RCC.
We present the case of a 44-year-old man with single omental metastasis of RCC after laparoscopic radical nephrectomy. Pathological diagnosis of the resected left kidney revealed pT3a clear cell RCC (Fuhrman grade III). At 6 mo postoperatively, abdominal computed tomography revealed a 12-mm enhancing nodule in the left lower peritoneum. At 7 mo after initial operation, laparoscopic removal of the left omental nodule was performed. The pathological results indicated metastatic clear cell RCC. Currently, the patient is being treated with adjuvant pembrolizumab.
Omental metastasis of RCC owing to laparoscopic radical nephrectomy is rare. Urologists should be aware of the diverse nature of RCC.
Core Tip: The authors present the case of a 44-year-old man with single omental metastasis of renal cell carcinoma (RCC) after laparoscopic radical nephrectomy. Omental metastasis of RCC owing to laparoscopic radical nephrectomy is rare. Urologists should be aware of the diverse nature of RCC.
- Citation: Chung JW, Kang JK, Lee EH, Chun SY, Ha YS, Lee JN, Kim TH, Kwon TG, Yoon GS. Single omental metastasis of renal cell carcinoma after radical nephrectomy: A case report. World J Clin Cases 2023; 11(25): 5994-5999
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/5994.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.5994
Renal cell carcinoma (RCC) is the third most common malignancy in the genitourinary tract[1]. In South Korea, the incidence of RCC has been rising, with 6952 new cases estimated in both sexes in 2022[2]. The lungs, bone, lymph nodes, liver, and brain are common metastatic sites of RCC[1,3]. However, literature on single omental metastasis of RCC is limited. We herein present the case of a 44-year-old man with single omental metastasis of RCC after laparoscopic radical nephrectomy.
A 44-year-old man with gross hematuria and left flank pain visited our emergency department on July 14, 2022.
The patient’s gross hematuria started 1 day before admission. In the morning of the day of visit, the hematuria became more severe and was accompanied with clots. Moreover, he experienced severe pain in the left flank.
The patient was healthy and had a history of appendectomy 10 years earlier.
The patient denied any history of tobacco or alcohol consumption. He had no medication history. His family history was unremarkable.
At the emergency department, the patient’s initial vital signs were stable. His blood pressure level was 129/79 mmHg, pulse rate was 81 beats/min, and respiratory rate was 16 breaths/min. The patient’s body weight was 86 kg, and his height was 171.0 cm (body mass index = 29.4 kg/m2). There was no palpable mass around the left flank area. The patient showed left flank tenderness but no rebound tenderness.
Laboratory serum tests were normal (hemoglobin level: 13.7 g/dL, creatinine level: 1.05 mg/dL, and calcium level: 9.1 mg/dL). Urinalysis revealed the presence of many red blood cells. Electrocardiogram indicated normal sinus rhythm.
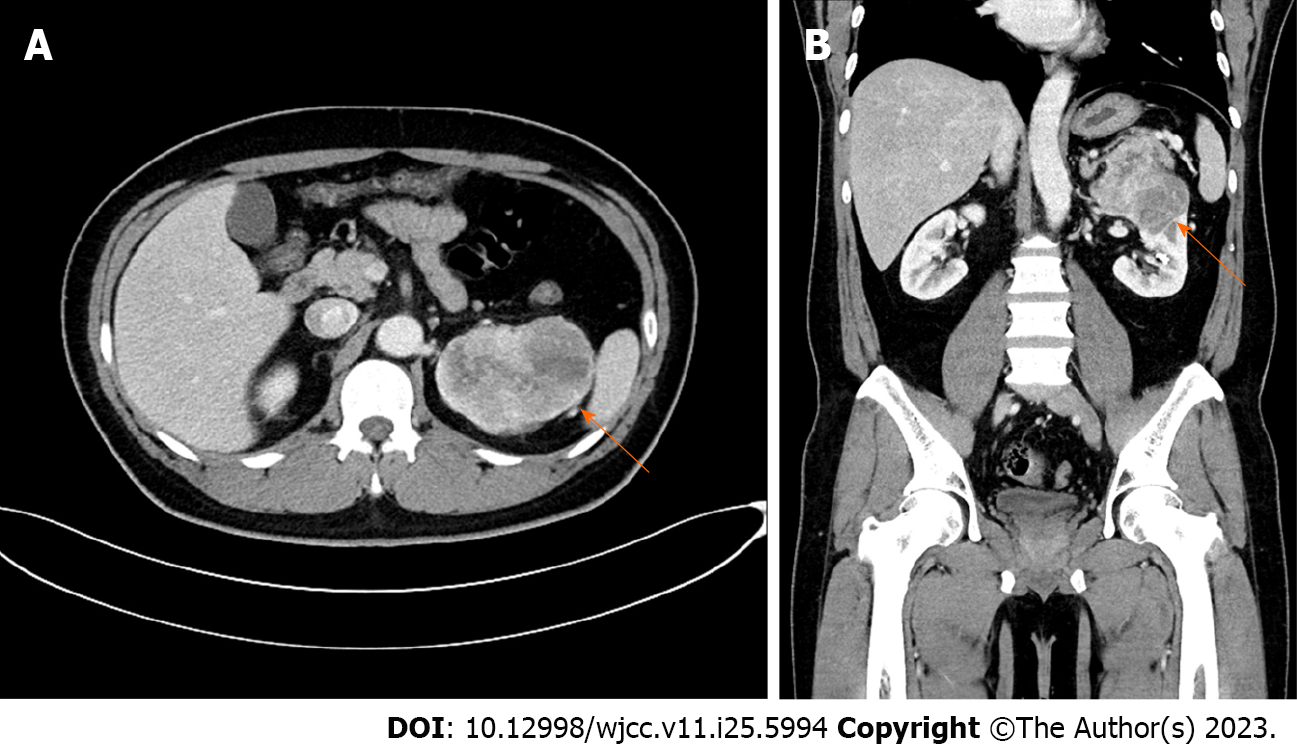
Initial kidney dynamic computed tomography (CT) (three phases of intravenous contrast enhancement) revealed an 8.8 cm × 6.1 cm heterogeneously enhancing mass in the upper to mid pole of the left kidney abutting the left adrenal gland and pancreas (Figure 1). No metastatic lesions were detected in the enhanced brain and chest CT scans.
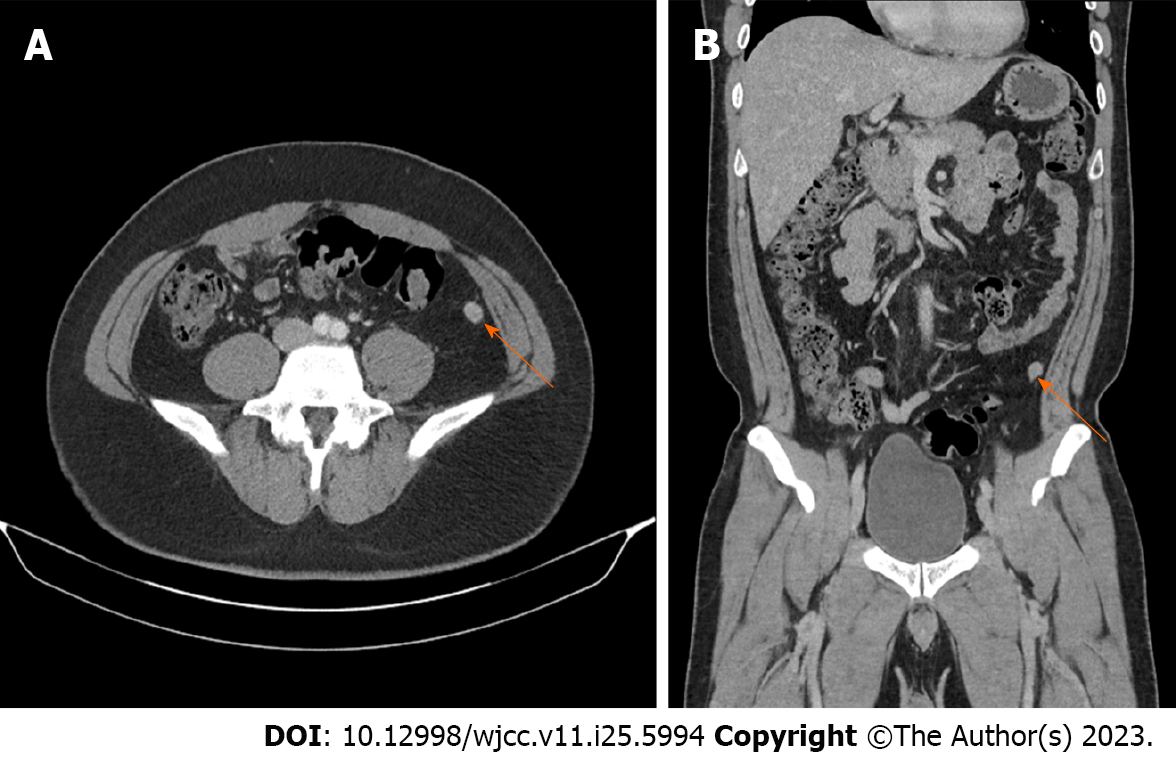
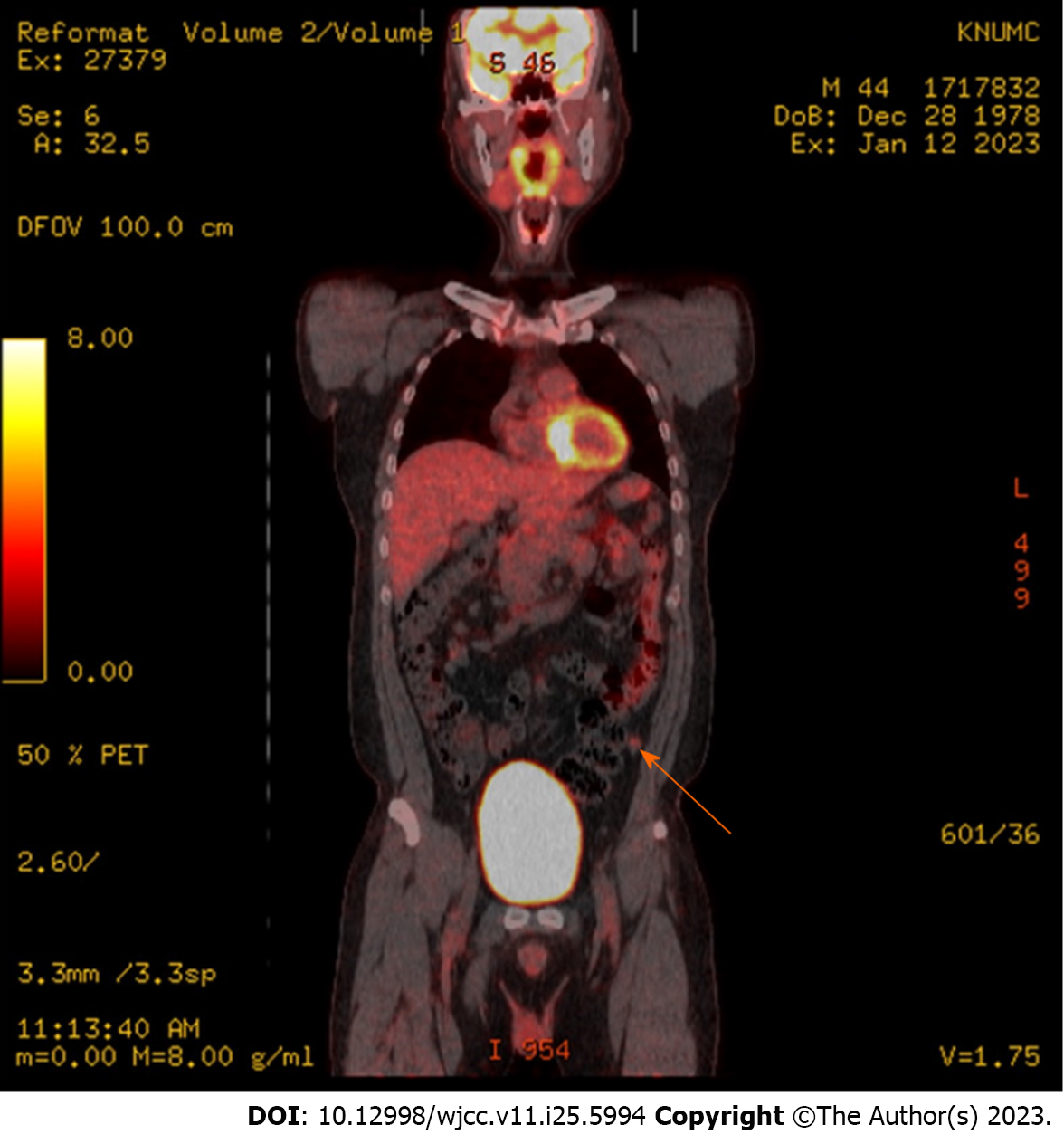
Follow-up CT 3 mo after radical nephrectomy showed no metastatic lesions. However, at 6 mo postoperatively, abdominal CT revealed a 12-mm enhancing nodule in the left lower peritoneum (Figure 2). 18F-fluorodeoxyglucose
Pathological diagnosis of the resected specimen from initial radical nephrectomy revealed pT3a clear cell RCC (Fuhrman grade III). Tumor capsular invasion was absent, but lymphovascular invasion and tumor cell necrosis were present (10%). No tumor was observed in the left adrenal gland.
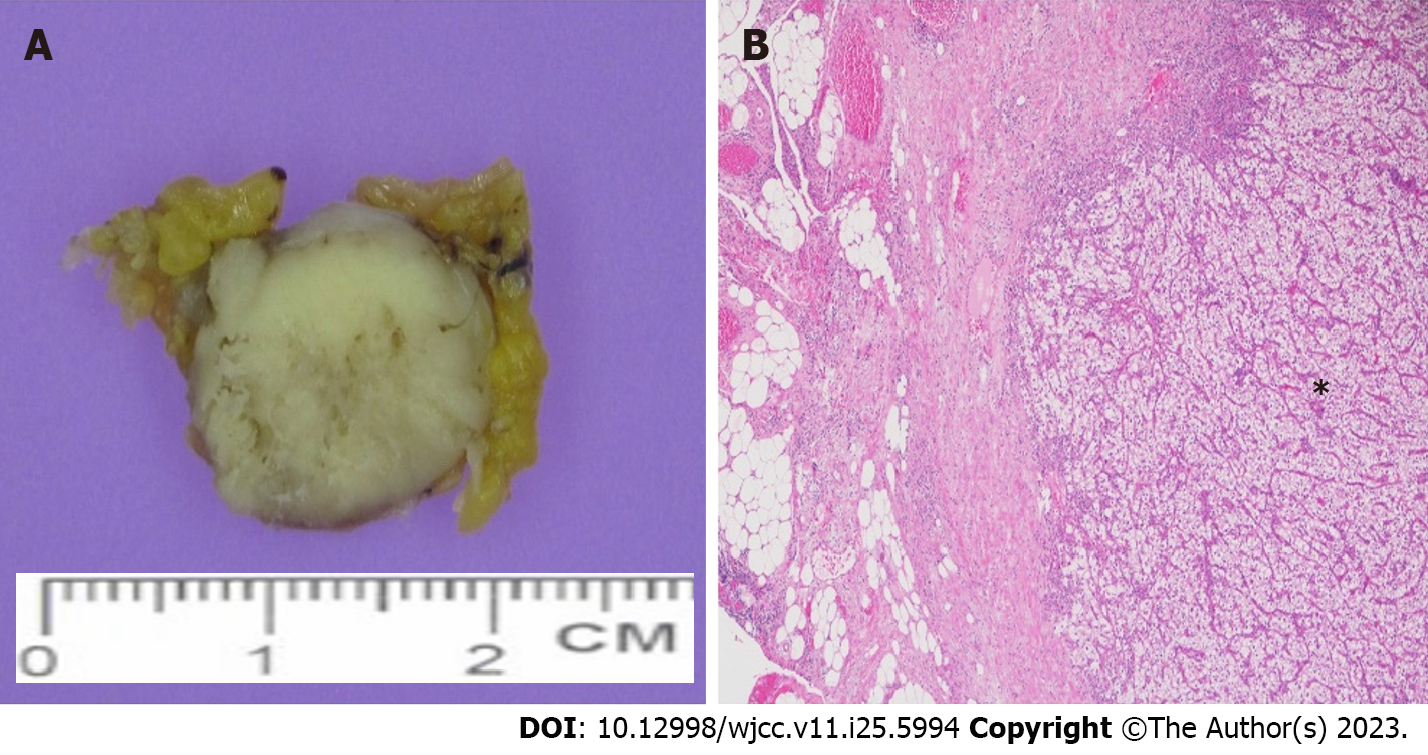
The pathological results of the second laparoscopic removal of the left omental nodule revealed metastatic clear cell RCC (Figure 4).
At the time of the patient’s visit to emergency department, he experienced severe flank pain and gross hematuria; therefore, we decided to perform emergency surgery rather than elective surgery. Laparoscopic radical nephrectomy and adrenalectomy were performed on the same day. We inserted a 12-mm camera port near the umbilicus. Mild adhesion was observed between the renal mass and pancreas, but pancreatic injury did not occur. No tumor spillage was found during radical nephrectomy. We further opened the 12-mm camera port to remove the specimen from the abdominal cavity using endobag (Lapbag®, SEJONG Medical).
On February 3, 2023, laparoscopic removal of the left omental nodule was performed. The patient underwent the second surgery in the supine position. A 12-mm port was inserted just above the umbilicus, and other 12- and 5-mm ports were inserted in the anterior axillary line at the level of the umbilicus and 2 cm below the xiphoid process. Fortunately, the nodule was visible immediately after entering the abdominal cavity, and the urologist could remove the nodule without any help from a general surgeon.
No metastatic lesion was observed in the most recent CT scan. The most recent brain, chest, and abdomen CT was performed on July 5, 2023. In other words, the interval between the primary surgery and the most recent CT was 12 mo.
Currently, the patient is being treated with adjuvant pembrolizumab. However, adjuvant pembrolizumab is not covered by Korean health insurance. Therefore, immediately after radical nephrectomy, he refused adjuvant pembrolizumab owing to its high cost but agreed to administer it after the second operation.
At our hospital, immunotherapy or targeted therapy for RCC is entirely established by urologists, not medical oncologists. Therefore, JWC decided to initiate treatment with adjuvant pembrolizumab. The duration/scheme of pembrolizumab application is intravenous injection every 3 wk, with at least ten administrations[4].
Thyroid function tests revealed minor abnormalities, but no recent side effects have been reported.
Kidney cancers are the third most common genitourinary malignancy, accounting for over 431288 new cancer diagnoses and over 179368 deaths worldwide annually[5]. CT and magnetic resonance imaging have increased the diagnosis of early RCC in many patients. The 5-year survival rate for early RCC is approximately 93%; however, the 5-year survival rate of RCC patients with metastases is only 12%[6].
RCC commonly metastasizes to the lung parenchyma (45.2%), bone (29.5%), lymph nodes (20.8%), liver (20.3%), adrenal glands (8.9%), and brain (8.1%)[1]. Metastases into the pancreas are rare and found mostly in asymptomatic patients[7]. Other atypical RCC metastases in the omentum, thyroid, and mediastinum are extremely rare. In particular, port-site metastasis or peritoneal metastasis after a laparoscopic procedure for urological malignancies is a rare event, accounting for approximately 0.09 % and 0.03 % of total cases, respectively[8,9]. RCC is the least common urological malignancy that leads to port-site metastasis or peritoneal metastasis, with only rare cases being reported in the literature[10].
In 2013, Ploumidis et al[9] presented a case report concerning tumor seeding in the omentum found in a 75-year-old female patient after a previous transperitoneal robot-assisted radical nephrectomy for papillary RCC. Two years after the initial surgery, the patient was diagnosed with cervical cancer, leading to radical hysterectomy with lymphadenectomy and omentectomy. Incidentally, a neoplastic omental nodule was discovered during the surgery. Pathological outcome and immunohistochemistry result confirmed the presence of features consistent with papillary RCC. In 2016, Acar et al[3] also presented a case report of a 62-year-old male patient who, 13 years after having undergone open extraperitoneal partial nephrectomy for pT1 clear cell RCC, developed an omental metastatic lesion.
Similarly, we present the case of a 44-year-old man with single omental metastasis of RCC after laparoscopic radical nephrectomy. We reviewed the recorded video of the surgery again and did not find intraoperative tumor spillage. We can conjecture that despite the absence of macroscopic surgically induced tumor spillage, there is a possibility that certain tumorigenic yet nonmetastasizing neoplastic cells, which typically do not survive the metastatic cascade under normal circumstances, could have been transferred and aided in establishing a novel neoplastic colony.
In summary, omental metastasis of RCC because of laparoscopic radical nephrectomy is rare. Urologists should be aware of the diverse nature of RCC. Various therapeutic approaches should be considered, such as morphological and functional imaging studies together with histopathological assessment of metastatic lesions, and a fundamental treatment for the causative disease should be applied.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Sawazaki H, Japan; Taskovska M, Slovenia S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Bruckschen F, Gerharz CD, Sagir A. Renal cell carcinoma with unusual metachronous metastasis up to 22 years after nephrectomy: two case reports. J Med Case Rep. 2021;15:490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Jung KW, Won YJ, Hong S, Kong HJ, Lee ES. Prediction of Cancer Incidence and Mortality in Korea, 2020. Cancer Res Treat. 2020;52:351-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 3. | Acar Ö, Mut T, Sağlıcan Y, Sag AA, Falay O, Selcukbiricik F, Tabak L, Esen T. Isolated omental metastasis of renal cell carcinoma after extraperitoneal open partial nephrectomy: A case report. Int J Surg Case Rep. 2016;21:6-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Choueiri TK, Tomczak P, Park SH, Venugopal B, Ferguson T, Chang YH, Hajek J, Symeonides SN, Lee JL, Sarwar N, Thiery-Vuillemin A, Gross-Goupil M, Mahave M, Haas NB, Sawrycki P, Gurney H, Chevreau C, Melichar B, Kopyltsov E, Alva A, Burke JM, Doshi G, Topart D, Oudard S, Hammers H, Kitamura H, Bedke J, Perini RF, Zhang P, Imai K, Willemann-Rogerio J, Quinn DI, Powles T; KEYNOTE-564 Investigators. Adjuvant Pembrolizumab after Nephrectomy in Renal-Cell Carcinoma. N Engl J Med. 2021;385:683-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 469] [Article Influence: 117.3] [Reference Citation Analysis (0)] |
| 5. | Saad AM, Gad MM, Al-Husseini MJ, Ruhban IA, Sonbol MB, Ho TH. Trends in Renal-Cell Carcinoma Incidence and Mortality in the United States in the Last 2 Decades: A SEER-Based Study. Clin Genitourin Cancer. 2019;17:46-57.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 136] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 6. | Kumar S, Singh V, Singh MK, Sankhwar SN. Management of Metastatic Renal Cell Carcinoma in a Tertiary Care Hospital. Cureus. 2023;e35623. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Tosoian JJ, Cameron JL, Allaf ME, Hruban RH, Nahime CB, Pawlik TM, Pierorazio PM, Reddy S, Wolfgang CL. Resection of isolated renal cell carcinoma metastases of the pancreas: outcomes from the Johns Hopkins Hospital. J Gastrointest Surg. 2014;18:542-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Tanaka K, Hara I, Takenaka A, Kawabata G, Fujisawa M. Incidence of local and port site recurrence of urologic cancer after laparoscopic surgery. Urology. 2008;71:728-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Ploumidis A, Panoskaltsis T, Gavresea T, Yiannou P, Yiannakou N, Pavlakis K. Tumor seeding incidentally found two years after robotic-Assisted radical nephrectomy for papillary renal cell carcinoma. A case report and review of the literature. Int J Surg Case Rep. 2013;4:561-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Castillo OA, Vitagliano G. Port site metastasis and tumor seeding in oncologic laparoscopic urology. Urology. 2008;71:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |