Published online Aug 26, 2023. doi: 10.12998/wjcc.v11.i24.5817
Peer-review started: June 10, 2023
First decision: June 21, 2023
Revised: July 10, 2023
Accepted: August 1, 2023
Article in press: August 1, 2023
Published online: August 26, 2023
Processing time: 75 Days and 23.3 Hours
Empty sella is an anatomical and radiological finding of the herniation of the subarachnoid space into the pituitary fossa leading to a flattened pituitary gland. Patients with empty sella may present with various symptoms, including headache due to intracranial hypertension and endocrine symptoms related to the specific pituitary hormones affected. Here, we report a female patient who developed persistent postoperative hypotension caused by subclinical empty sella syndrome after a simple surgery.
A 47-year-old woman underwent vocal cord polypectomy under general anesthesia with endotracheal intubation. She denied any medical history, and her vital signs were normal before the surgery. Anesthesia and surgery were uneventful. However, she developed dizziness, headache and persistent hypo
Endocrine etiologies such as pituitary and adrenal-related dysfunction should be considered in patients showing persistent postoperative hypotension when anesthesia- and surgery-related factors are excluded.
Core Tip: Perioperative hypotension is commonly caused by hypovolemia, reduced vascular tone and cardiac insufficiency. Occasionally, perioperative hypotension can be attributed to an endocrine etiology such as empty sella syndrome, as in our patient, which led to decreased adrenocorticotropic hormone secretion and secondary adrenal insufficiency. Therefore, clinicians managing persistent hypotension should consider the endocrine dysfunctions when common hypotension causes are excluded.
- Citation: Zhao KM, Hu JS, Zhu SM, Wen TT, Fang XM. Persistent postoperative hypotension caused by subclinical empty sella syndrome after a simple surgery: A case report. World J Clin Cases 2023; 11(24): 5817-5822
- URL: https://www.wjgnet.com/2307-8960/full/v11/i24/5817.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i24.5817
Empty sella is an anatomical and radiological finding of the herniation of the subarachnoid space into the sella turcica, which results in an elongated stalk and a flattened pituitary[1-3]. The incidence of primary empty sella is approximately 8%-35% in the general population. Most people with empty sella are asymptomatic. Patients with symptoms may experience headache due to increased intracranial pressure and endocrine dysfunctions depending on the affected hormones, including hyperprolactinemia and hypopituitarism. Rarely, primary empty sella is found without any hormone deficiency in some patients[4].
Perioperative hypotension is a common phenomenon. Common causes of perioperative hypotension include hypovolemia, reduced vascular tone and cardiac insufficiency caused by anesthesia[5,6]. However, postoperative hypotension can also be attributed to rare endocrine etiologies. Here we describe a patient who was asymptomatic before surgery but developed persistent postoperative hypotension due to empty sella syndrome.
The patient had hoarseness for two months.
A 47-year-old woman weighing 50 kg was presented to us with a two-month history of hoarseness after an influenza. She was diagnosed with vocal cord polyps and was scheduled for vocal cord polypectomy under general anesthesia. Her preoperative blood pressure was 112/78 mmHg, and her heart rate was 85 beats per minute. Anesthesia was induced intravenously with fentanyl (0.25 mg), propofol (100 mg), and rocuronium (50 mg), and the patient was then intubated. The anesthesia was maintained with propofol (100 µg/kg/min), remifentanil (0.5 µg/kg/min), and 1% inhaled sevoflurane. The surgery lasted approximately 15 min with a negligible amount of bleeding. Intraoperative blood pressure was stable, and no vasoactive drugs were administered. After surgery, the patient was transferred to the post-anesthesia care unit. Approximately one hour after the surgery, the patient was awake and extubated. She showed a gradual decrease in blood pressure in the recovery room. However, this decrease did not cause concern as her blood pressure was still in the normal range. Her symptoms progressed when she went back to the ward, where she developed low blood pressure and dizziness. Her lowest blood pressure was 77/45 mmHg after fluid therapy. Therefore, intravenous dopamine (3.3 mg/kg·min) was administered to maintain normal blood pressure and the patient’s symptoms improved. Surprisingly, the patient remained dependent on dopamine for more than 24 h without any obvious anesthesia- and surgery-related complications. Therefore, an endocrine etiology was suspected. Her blood hormone levels were then tested, and she underwent brain magnetic resonance imaging (MRI).
The patient did not have a history of past illness.
She denied any personal and family history.
On physical examination, her vital signs were as follows: Body temperature 36.0 °C; blood pressure, 94/73 mmHg with dopamine infusion; heart rate 62 beats per minute and respiratory rate, 16 breaths/min. The patient reported dizziness and slight throat pain.
Endocrine examination of her blood sample revealed an increase in prolactin, a low normal adrenocorticotropic hormone (ACTH) and a decreased cortisol level. The other hormones tested were in the normal range (Table 1).
| Variable | Measured value | Reference range |
| Growth hormone | 0.058 µg/L | 0.010-3.607 µg/L |
| Prolactin | 704 mIU/L | 70-566 mIU/L |
| Thyroid stimulating hormone | 1.78 mIU/L | 0.38-5.33 mIU/L |
| Free triiodothyronine | 4.34 pmol/L | 3.28-6.47 pmol/L |
| Adrenocorticotropic hormone | < 5 pg/L | 0-46 pg/L |
| Follicle stimulating hormone | 10.8 IU/L | - |
| Luteinizing hormone | 11.1 IU/L | - |
| Estradiol | 510.8 pmol/L | - |
| Progesterone | 0.11 nmol/L | - |
| Testosterone | 0.13 nmol/L | 0.00-2.60 nmol/L |
| Cortisol (8 a.m.) | 6.23 µg/L | 52.70-224.50 µg/L |
| Serum sodium | 137.4 mmol/L | 137.0-147.0 mmol/L |
| Serum potassium | 3.85 mmol/L | 3.5-5.3 mmol/L |
| 24 h urine | 1200 mL | 1500-2500 mL |
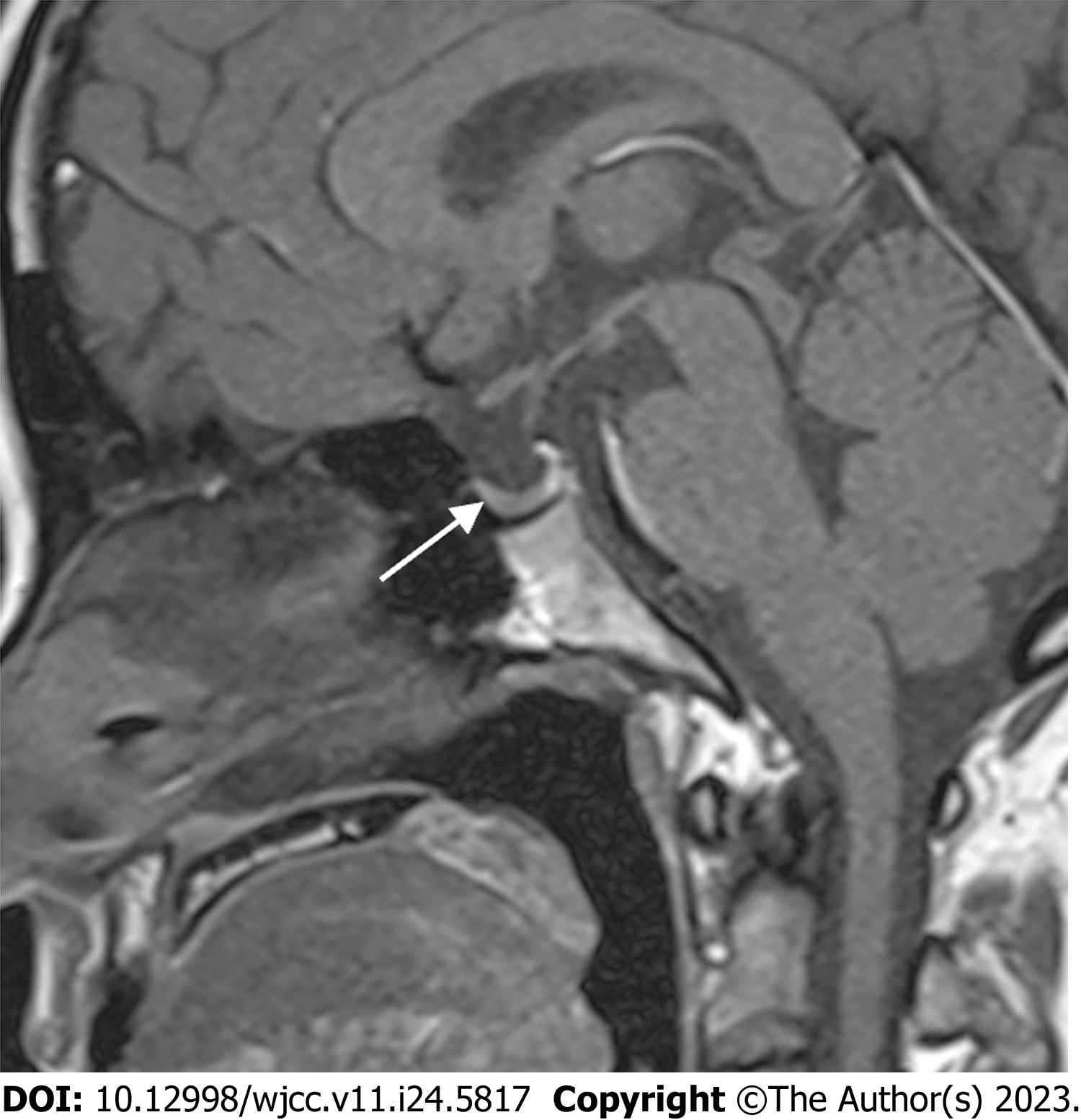
Brain MRI revealed an empty sella (Figure 1).
Empty sella syndrome and secondary adrenal insufficiency.
Following diagnosis of empty sella syndrome and secondary adrenal insufficiency, the patient was started on intravenous methylprednisolone treatment. Her blood pressure gradually increased to the normal range and dopamine infusion was stopped.
Two days later, the patient's symptoms subsided. She was switched to oral prednisone tablets and discharged from the hospital. A telephone interview one year after hospital discharge revealed that the patient did not have any discomfort and did not require further examination or treatment.
Empty sella is an anatomical finding of a flattened pituitary in the sellar space filled with cerebral fluid. Primary empty sella is caused by anatomical abnormalities, increased intracranial pressure or enlarged pituitary gland without underlying pathologies. While secondary empty sella results from pathogenic conditions, such as genetic diseases, hypophysis, pituitary stroke, Sheehan syndrome, pituitary surgery and/or radiation therapy, brain trauma, and infection[1-4]. Empty sella is more likely to be present in women than in men. The reason for the development of empty sella syndrome in our patient is unknown. Revision of her medical history did not show any obvious cause. As she did not report any discomfort before surgery while performing daily activities and thus empty sella syndrome was not diagnosed. We suspected that the surgery and anesthesia caused a stress response much greater than what she encountered during daily activities, resulting in her symptoms soon after the surgery.
The perioperative influence of empty sella syndrome varies depending on the specific hormones affected. Hormonal assessment is advocated in all patients with empty sella. Both multiple and isolated pituitary hormones deficiencies can be found in these patients. Hypopituitarism is most common with a 50% prevalence in primary empty sella patients. Hyperprolactinemia due to a lack of the inhibitory effect of dopamine from the hypothalamic region is also frequently found in empty sella syndrome[1-4,7]. Pituitary hormones from both anterior and posterior lobe are essential for maintenance of blood pressure, especially under stress. Notably, thyroid stimulating hormone (TSH) and ACTH from the anterior lobe are important to produce thyroxine and cortisol, both of which show permissive effects on the actions of catecholamines. Lamont and colleagues reported a rare case in which both ACTH and vasopressin were decreased in a patient with empty sella syndrome undergoing cardiac surgery[8]. Their patient suffered from hypotension post-operatively, and supplement of both cortisol and vasopressin corrected the symptom. Rarely, panhypopituitarism can be found with empty sella syndrome. Our patient showed an affected anterior lobe and presented with a normal TSH and free triiodothyronine (FT3), a mild high prolactin, a low normal ACTH, and a low cortisol level. In this case, posterior lobe hormone such as vasopressin were less likely to be affected as sodium and potassium level, 24-h urine amount and urine and plasma osmolarity (not shown) were in the normal range. Therefore, cortisol supplementation was effective in controlling her symptom.
Surgery and anesthesia can induce stress response which is associated with elevated cortisol level. In a patient with normal hypothalamus-pituitary-adrenal axis function, even minimal invasive surgeries can induce upregulation of cortisol due to the stress response, especially with general anesthesia[9]. Patients undergoing minimal invasive surgeries show increased cortisol level over 24 h post-surgery and the cortisol level is doubled than that of the healthy unstressed adults[10]. For moderate and high invasive surgeries, the mean cortisol level is much increased compared with minimal invasive procedures and remains elevated even up to post-operative day 7[10]. Endotracheal intubation and extubation and opening the mouth with a mouth prop are the steps that may induce the strongest stress during the polypectomy procedure, although polypectomy per se is not particularly invasive. The anesthesia record of our patient showed an increased blood pressure from the start of the surgery, which suggested an increased stress response. Adequate analgesia and muscle relaxation are essential to minimize the stress response[11].
Patients with lesions in the hypothalamus-pituitary-adrenal axis and those with chronic steroid intake may exhibit insufficient cortisol secretion in an emergent situation[12-14]. Although administration of “stress doses” of steroids during the perioperative period is controversial, some authors advocate the administration of such doses depending on the surgical stress risk due to the possible detrimental consequences of adrenal crisis. Our patient could have been benefited from preoperative administration of steroids.
Our case highlights the importance of endocrine hormones in maintaining blood pressure. Empty sella syndrome affecting hormones from the pituitary and the downstream target hormones can lead to severe perioperative hypotension. When perioperative hypotension occurred without apparent common surgery and anesthesia related reasons, endocrine etiology should be considered and evaluated.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Yarmahmoodi F, Iran S-Editor: Yan JP L-Editor: A P-Editor: Cai YX
| 1. | Chiloiro S, Giampietro A, Bianchi A, Tartaglione T, Capobianco A, Anile C, De Marinis L. DIAGNOSIS OF ENDOCRINE DISEASE: Primary empty sella: a comprehensive review. Eur J Endocrinol. 2017;177:R275-R285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 2. | Chiloiro S, Giampietro A, Bianchi A, De Marinis L. Empty sella syndrome: Multiple endocrine disorders. Handb Clin Neurol. 2021;181:29-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Maira G, Anile C, Mangiola A. Primary empty sella syndrome in a series of 142 patients. J Neurosurg. 2005;103:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Carosi G, Brunetti A, Mangone A, Baldelli R, Tresoldi A, Del Sindaco G, Lavezzi E, Sala E, Mungari R, Fatti LM, Galazzi E, Ferrante E, Indirli R, Biamonte E, Arosio M, Cozzi R, Lania A, Mazziotti G, Mantovani G. A Multicenter Cohort Study in Patients With Primary Empty Sella: Hormonal and Neuroradiological Features Over a Long Follow-Up. Front Endocrinol (Lausanne). 2022;13:925378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Liem VGB, Hoeks SE, Mol KHJM, Potters JW, Grüne F, Stolker RJ, van Lier F. Postoperative Hypotension after Noncardiac Surgery and the Association with Myocardial Injury. Anesthesiology. 2020;133:510-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 6. | Khanna AK, Shaw AD, Stapelfeldt WH, Boero IJ, Chen Q, Stevens M, Gregory A, Smischney NJ. Postoperative Hypotension and Adverse Clinical Outcomes in Patients Without Intraoperative Hypotension, After Noncardiac Surgery. Anesth Analg. 2021;132:1410-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Auer MK, Stieg MR, Crispin A, Sievers C, Stalla GK, Kopczak A. Primary Empty Sella Syndrome and the Prevalence of Hormonal Dysregulation. Dtsch Arztebl Int. 2018;115:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Lamont SN, McBride WT, Bill KM, Varadarajan B. Profound vasodilatory hypotension in a patient with known empty sella syndrome following cardiac surgery. Anaesthesia. 2007;62:846-849. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1231] [Cited by in RCA: 1283] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 10. | Prete A, Yan Q, Al-Tarrah K, Akturk HK, Prokop LJ, Alahdab F, Foster MA, Lord JM, Karavitaki N, Wass JA, Murad MH, Arlt W, Bancos I. The cortisol stress response induced by surgery: A systematic review and meta-analysis. Clin Endocrinol (Oxf). 2018;89:554-567. [PubMed] |
| 11. | Nandi R, Basu SR, Sarkar S, Garg R. A comparison of haemodynamic responses between clinical assessment-guided tracheal intubation and neuromuscular block monitoring-guided tracheal intubation: A prospective, randomised study. Indian J Anaesth. 2017;61:910-915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Marik PE, Varon J. Requirement of perioperative stress doses of corticosteroids: a systematic review of the literature. Arch Surg. 2008;143:1222-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 142] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Hahner S, Ross RJ, Arlt W, Bancos I, Burger-Stritt S, Torpy DJ, Husebye ES, Quinkler M. Adrenal insufficiency. Nat Rev Dis Primers. 2021;7:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 14. | Bancos I, Hahner S, Tomlinson J, Arlt W. Diagnosis and management of adrenal insufficiency. Lancet Diabetes Endocrinol. 2015;3:216-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 248] [Article Influence: 24.8] [Reference Citation Analysis (0)] |