Published online Aug 26, 2023. doi: 10.12998/wjcc.v11.i24.5762
Peer-review started: May 11, 2023
First decision: July 7, 2023
Revised: July 17, 2023
Accepted: July 31, 2023
Article in press: July 31, 2023
Published online: August 26, 2023
Processing time: 105 Days and 16.2 Hours
Endovascular recanalization of non-acute intracranial artery occlusion is techni
A 74-year-old man was admitted to the hospital two days after experiencing acute weakness in both lower extremities, poor speech, and dizziness. After admission, imaging revealed acute ischemic stroke and non-acute occlusion of bilateral intracranial vertebral arteries (ICVAs). On the fourth day of admission, the patient's condition deteriorated and an emergency endovascular recanalization of the left ICVA was performed. During this procedure, a microwire was advanced in the subintima of the vessel wall and successfully reentered the distal true lumen. Two stents were implanted in the subintima. The patient's Modified Rankin Scale was 1 at three months postoperatively.
We present a technical case of subintimal recanalization for non-acute ICVA occlusion in an emergency endovascular procedure. However, we emphasize the necessity for caution when applying the subintimal tracking approach in intracranial occlusion due to the significant dangers involved.
Core Tip: Technical challenges arise during endovascular recanalization of non-acute intracranial artery occlusions, particularly when the microwire enters the subintima. To our knowledge, this article details the first successful case of subintimal recanalization for non-acute intracranial vertebral artery occlusion in a patient with progressive ischemic stroke. However, we emphasize the necessity for caution when applying the subintimal tracking approach in intracranial occlusion due to the significant dangers involved.
- Citation: Fu JF, Zhang XL, Lee SY, Zhang FM, You JS. Subintimal recanalization for non-acute occlusion of intracranial vertebral artery in an emergency endovascular procedure: A case report. World J Clin Cases 2023; 11(24): 5762-5771
- URL: https://www.wjgnet.com/2307-8960/full/v11/i24/5762.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i24.5762
Intracranial vertebral artery (ICVA) occlusion is a prevalent but frequently disregarded condition[1-3]. There are no established recommendations for endovascular recanalization of ICVA non-acute occlusion (mostly chronic occlusion). Previous studies have indicated procedural success rates of 75%-100% and perioperative complications of 0%-37.5%[4-6].
When there is heavy fibrous calcified plaque or when the course of the occlusion is unclear during neuro-endovascular interventions, the guidewire frequently fails to cross the occlusive lesion[4]. Additionally, the guidewire favors areas of low resistance, which makes it enter the subintima automatically.
The subintimal tracking and re-entry (STAR) technique has been well-established in peripheral vasculature[7-9]. In chronic total occlusion (CTO) of the internal carotid artery (ICA), Chen et al[10] indicated that the STAR technique may be used liberally below the ophthalmic artery segment due to a lack of major side branches. This article describes a case of fortuitous subintimal recanalization for non-acute ICVA occlusion.
A 74-year-old man presented acute weakness in both lower extremities, poor speech, and dizziness for two days.
At the beginning of the two days, prior to admission, the patient awoke in the morning with a sudden onset of weakness in both lower extremities, poor speech, and dizziness, with a spinning sensation that lasted for several minutes, without headache, nausea, vomiting, or any difficulty swallowing.
The patient had a history of hypertension with poor management for over 10 years. He began experiencing recurrent episodes of vertigo six months prior, and the transcranial Doppler (TCD) revealed a peak systolic/end-diastolic flow velocity of 26/11 cm/s in the left ICVA. At that time, he was taking aspirin and a statin.
He had been smoking for over 60 years. He declined to provide other personal and family medical history.
The National Institutes of Health Stroke Scale (NIHSS) at admission was 4. The main neurological examinations included grade 4+ muscle strength of both lower extremities, mild facial and tongue paralysis on the right side, and the presence of bilateral Babinski's sign.
No obvious abnormalities were found on routine blood tests, routine urine tests, routine fecal tests, blood biochemistry and immune indexes.
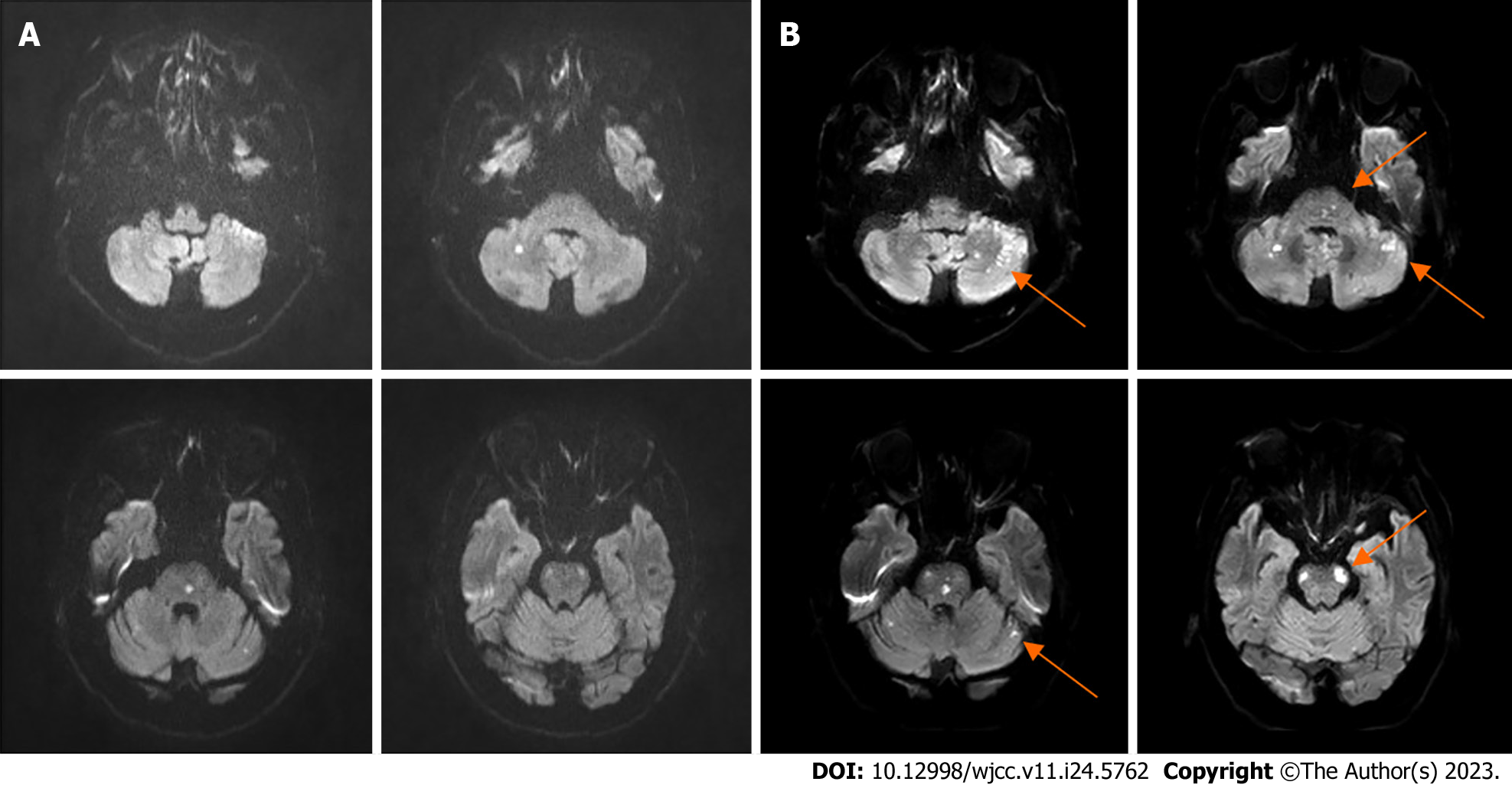
A brain Magnetic Resonance Imaging (MRI) revealed scattered acute infarcts in the posterior circulation (Figure 1A).
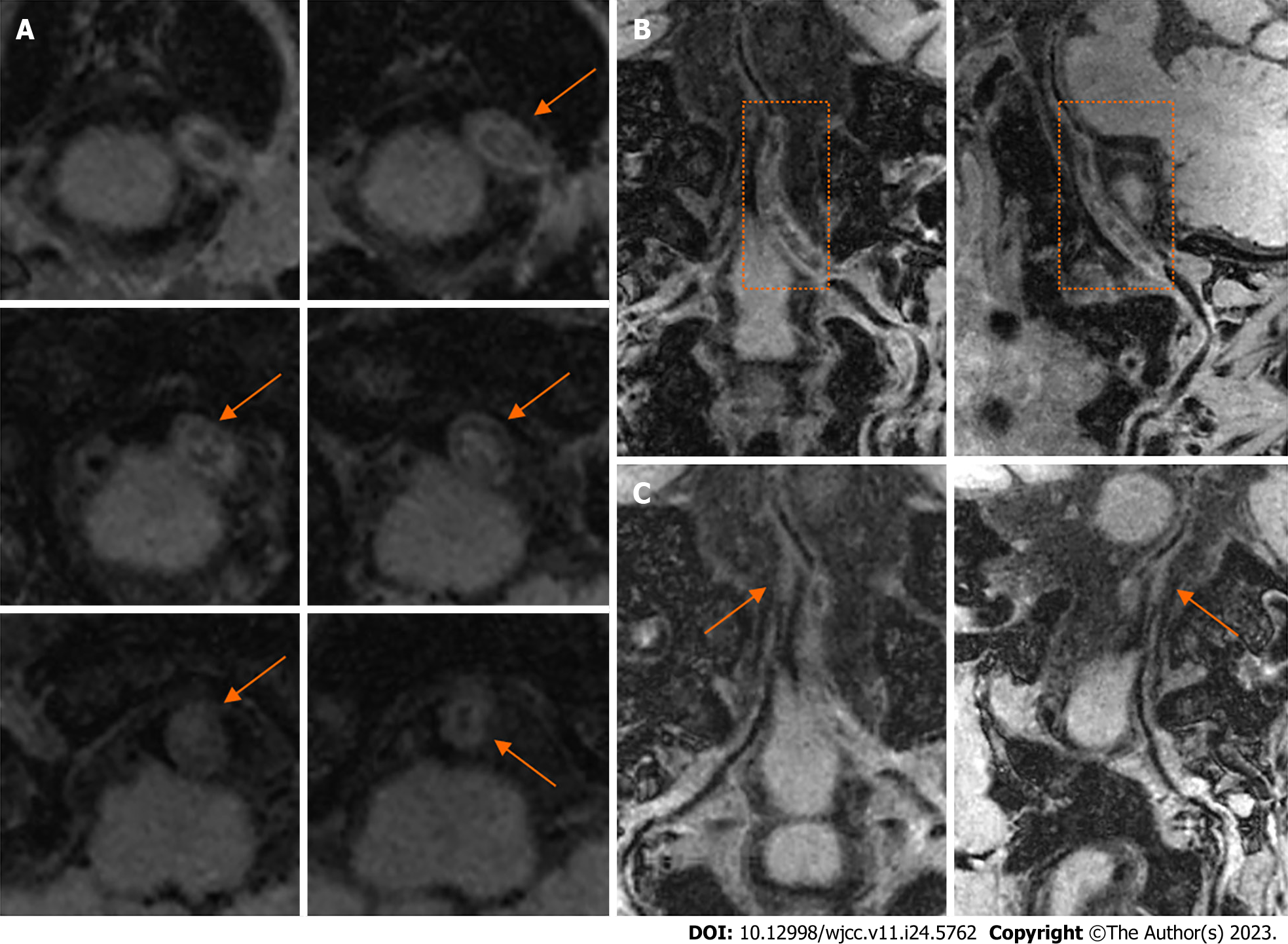
On the second day of admission, cerebral angiography revealed that the left vertebral artery (VA) had been occluded close to the origin of the left posterior inferior cerebellar artery (PICA) with a blunt proximal stump, and the right VA had been occluded near the junction of the basilar artery (BA). The BA was supplied by the anastomosis of the right VA branch vessels. No patent posterior communicating artery (PComA) was identified (Figure 2).
Then, a High-Resolution Magnetic Resonance Imaging (HRMRI) in the T1-weighted sequence revealed long-range thrombosis, lumen occlusion, wall thickening and no notable hyperintense signals far from the V4 segment of the left VA (Figure 3).
The final diagnosis was progressive ischemic stroke coupled with intracranial vertebral artery occlusion.
On admission, aspirin, clopidogrel, and atorvastatin were administered orally. Meanwhile, the intravenous fluid infusion was increased to improve cerebral perfusion. Nevertheless, the patient's symptoms fluctuated.
On the fourth day of admission, the patient's condition deteriorated and the NIHSS increased to 10, in addition to a repeat brain MRI which revealed a larger infarct (Figure 1B). Then, we decided to perform an emergency endovascular procedure to open the left ICVA. After we explained the patient's situation and the treatment plan to his family, they expressed their understanding and signed their written informed consent to the procedure.
Aspiration thrombectomy was initially used. The 6F Sofia intermediate catheter (MicroVention) was introduced close to the left vertebral artery occlusion through the 6F long sheath, however, no thrombus was retrieved via intermediate catheter aspiration.
Subsequently, the Synchro microwire (Stryker) and PILOT-50 guidewire (Abbott) were used alternatively to try to penetrate the proximal end of the occlusion with the assistance of a Rebar 18 microcatheter (eV3 Covidien) under the guidance of a roadmap. However, the organization of thrombus and the stiffer proximal fibrous cap, as well as the frequent slips of the microwire into the nearby PICA branch made it challenging to manipulate the microwire through the occlusion. After changing its direction of advancement, the microwire eventually entered the proximal end of the occlusion. The resistance and morphology of the advancing microwire indicated that it entered the subintima. Since the guidewire was located in the subintima, we were unable to perform routine mechanical thrombectomy using a stent retriever.
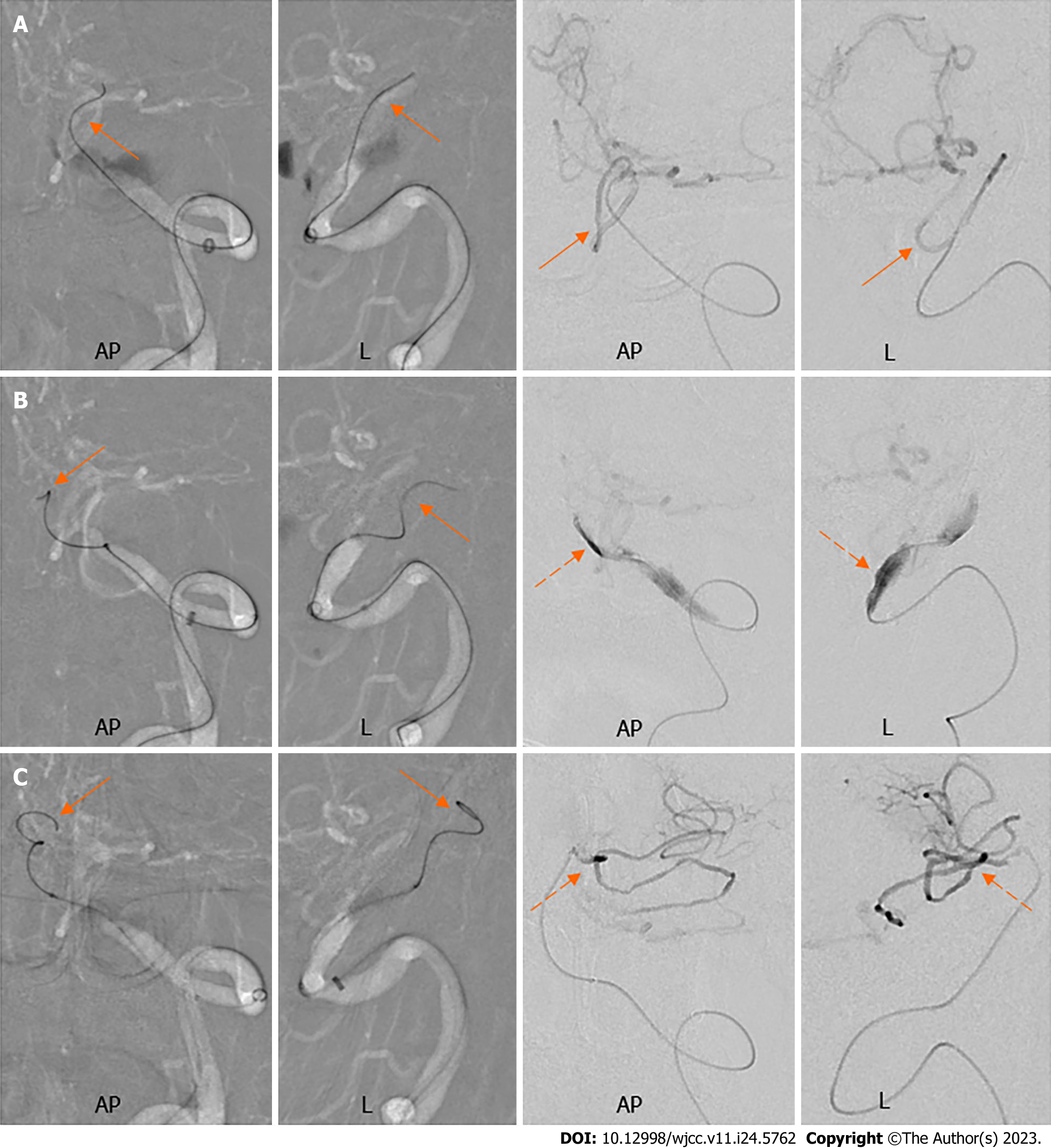
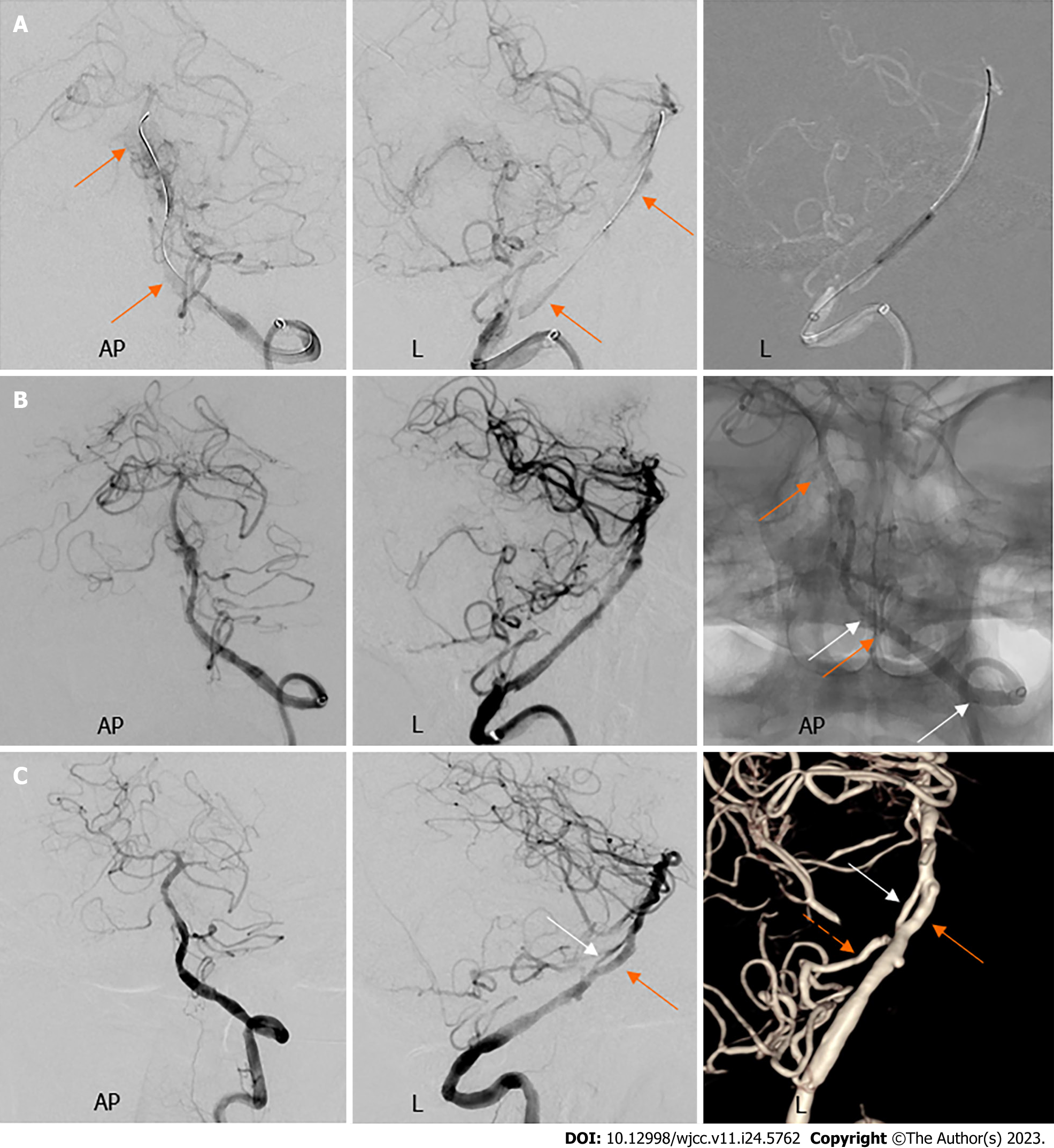
The roadmap served as a guide as the microwire was repeatedly repositioned so that it advanced into the subintimal space with a sigmoid curve. Microcatheter angiography was then used to evaluate the position of the microwire, the morphology of the subintimal channel, and to look for potential microchannels leading to the true lumen (Figure 4).
When the subintimal microwire approached the anterior inferior cerebellar artery (AICA), the microcatheter angiography implied entry into the AICA branch. The microwire was then carefully withdrawn, reoriented, and it continued advancing in the subintima. As the microwire advanced to the distal end of the occlusion, microcatheter angiography revealed the position of the true lumen and the existence of microchannel connectivity between the subintima and the true lumen. Subsequently, the microwire and the microcatheter were manipulated to attempt to cross the microchannel under the guidance of the roadmap. Eventually, the microwire re-entered the true lumen and was advanced to the left superior cerebellar artery (Figure 5).
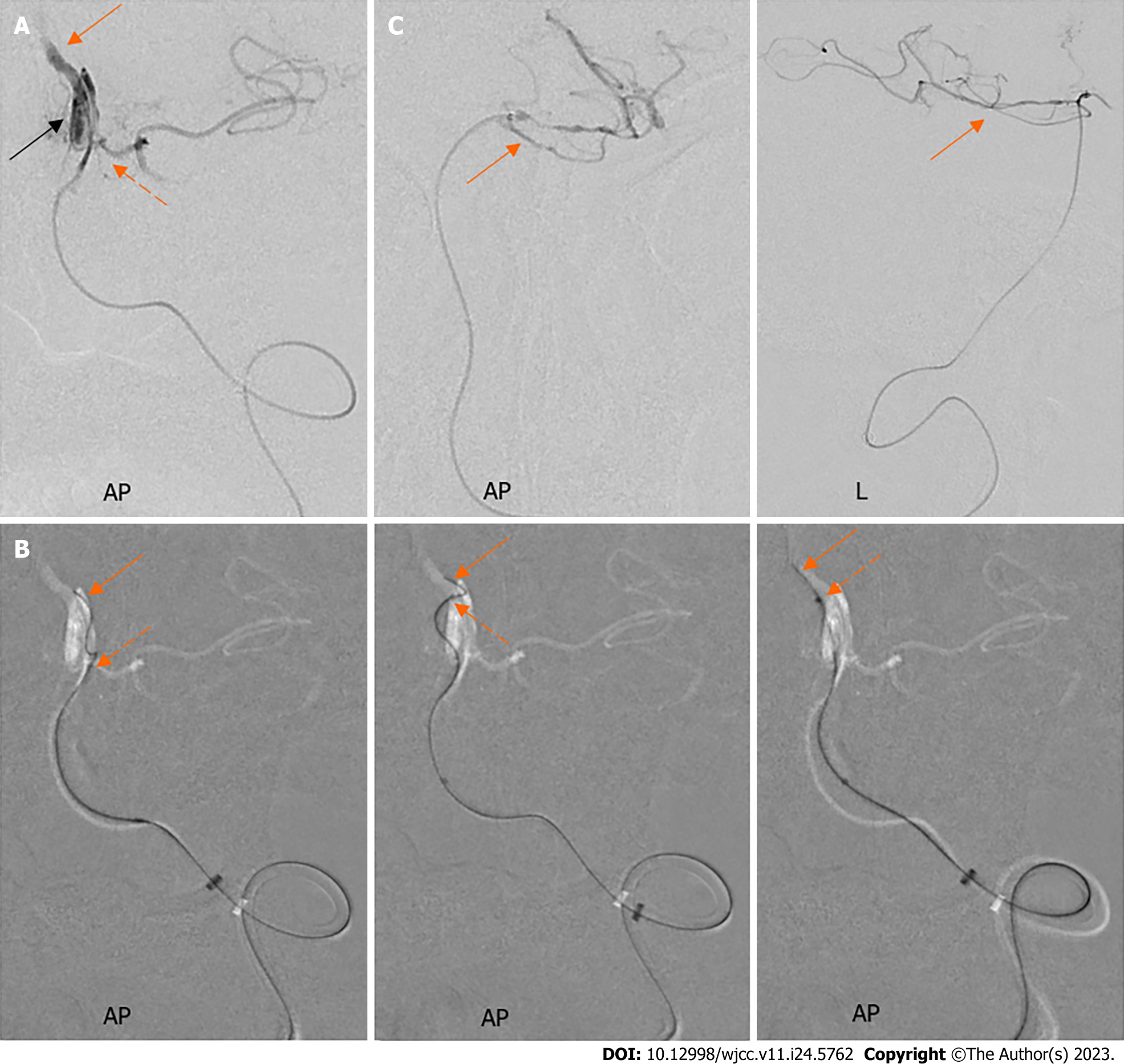
The subintimal channel was completely covered by the placement of two Enterprise stents (Codman) after distal and proximal dilation twice with a balloon (Figure 6). Repeat imaging revealed the Thrombolysis in Cerebral Infarction score of 3, and satisfactory stent apposition, therefore the procedure was completed. There were no intraoperative complications such as distal embolism from thrombus dislodgment, subarachnoid hemorrhage from vessel perforation, or in-stent thrombosis.
On postoperative day 1, repeat brain MRI did not reveal any new infarction or hemorrhage, and TCD demonstrated smooth in-stent flow with a flow velocity of 78/24 cm/s. Upon discharge, the patient's symptoms had greatly improved, and the NIHSS score was 3.
At 3 mo postoperatively, the follow-up angiography revealed satisfactory vascular healing and smooth blood flow in the subintimal channel without in-stent re-stenosis (Figure 6). At that time, the patient's modified Rankin Scale was 1.
In this patient, cerebral angiography revealed that the lesions involved bilateral vertebral arteries. No patent PComA was found (Figure 2). We speculated that the progressive stroke mechanism was hypoperfusion, which would have affected the clearance and destination of embolic particles due to the poor vascular state and collateral circulation[11].
We viewed the patient's left VA lesion as a non-acute occlusion in this case. According to prior studies, the blunt stump was associated with a CTO at a late stage[10,12]. Additionally, we did not detect any notable hyperintense signals in the HRMRI, indicating the absence of any fresh thrombus or intraplaque hemorrhage[13,14]. Furthermore, the operator felt more resistance when attempting to push the microwire through the proximal end of the occlusion, which differed from acute occlusion due to atherosclerosis-related in situ stenosis. As a result, we could reasonably assume that it was a chronic occlusion with more fibrous composition and organized thrombus[15].
Although initially optimal medical therapy was administered, this patient's symptoms worsened, but the infarct size was not large, resulting in a clinical-core mismatch. We thought that urgent endovascular recanalization was necessary, as stated by Aghaebrahim et al[16] as a reason for the intervention.
We discovered that the existence of a branch vessel close to the proximal occlusion may have made the procedure more difficult[17]. As in this case, the left VA was occluded after the PICA originated and the guidewire repeatedly entered the PICA branch (Figure 4). However, obvious wall thickening in the occlusive lesion, acceptable occlusion length, and the absence of lumen collapse made us more confident in the successful subintimal recanalization in this patient.
The STAR technique was initially presented in the 1980s to treat superficial femoral CTO[7]. Subsequently, it was developed in coronary CTO, where a more systematic subintimal recanalization strategy was designed based on modern percutaneous transluminal coronary intervention techniques and dedicated CTO devices[18].
Currently, endovascular recanalization of intracranial non-acute occlusion lacks dedicated CTO devices and techniques. For this patient, depending on the resistance of the guidewire in the occluded lesion, we alternated between the Synchro microwire and the PILOT-50 guidewire. The Synchro microwire has a softer tip and is safer in low resistance locations, although excessive guidewire bending should be avoided to expand the subintimal space. The PILOT guidewire has better penetration and can more easily enter the subintima, although attention is required to prevent perforation. Additionally, the microcatheter can increase the backup support and improve guidewire penetration. Subintimal microcatheter angiography can evaluate the morphology of the subintimal channel and look for potential microchannels leading to the true lumen.
The morphology of the subintimal channel or dissection is associated with technical success. According to interventional cardiologists Carlino et al[19], a "tubular" dissection shows that the microcatheter is in the subintima, and the success rate of guidewire re-entry into the real lumen is higher; in contrast, a "storm cloud" dissection suggests that the contrast has extravasated into the peri-adventitial regions. If a "storm cloud" dissection occurs, it is important to carefully evaluate the danger of vascular perforation and the procedure should be stopped if required. For this patient, the microcatheter angiography revealed a "tubular" pattern, indicating that the guidewire was in the subintima and the procedure was eventually successful (Figure 5).
According to several CTO pathologic and imaging studies[15,20], the neo-vessels within the intimal plaque are in touch with the subintimal vasa vasorum. These microchannels may be detected by microcatheter angiography making it easier for the guidewire to re-enter the true lumen. For this patient, we performed microcatheter angiography with about 0.2 mL of contrast by hand and found the location of the distal true lumen. Subsequently, the guidewire was successfully manipulated to re-enter the true lumen under the guidance of the roadmap (Figure 5).
Although a positive clinical outcome was achieved in this case with subintimal stenting, adoption of the subintimal recanalization technique in intracranial non-acute occlusions is still debatable because of the technical challenges and the high risk of the procedure.
The architecture of intracranial vessels differs from that of the peripheral vasculature. In the intradural portion of intracranial arteries, the external elastic lamina progressively disappears and connective tissues are sparse[21-23], so advancement of the subintimal guidewire can easily cause vascular perforation and catastrophic subarachnoid hemorrhage. Only lesions with sufficient wall thickening and no lumen collapse should be attempted on. Fortunately, there was no vascular perforation in this case.
Evaluation of the distal branches is crucial. According to Galassi et al[24], the subintimal guidewire is frequently re-entered into the true lumen at the distal vascular branch in coronary CTO. As for ICA CTO, the level of distal ICA reconstitution at the ophthalmic or communicating segments was predictive of a significantly lower rate of success[10]. Distal branches may occasionally be penetrated by the subintimal guidewire. Careful manipulation is necessary to prevent branch perforation due to the fragility of the intracranial branches. Additionally, the subintimal tracking technique should be avoided in the presence of major branches since subintimal balloon dilation or stenting may result in intima tears and subsequent branch occlusion. It is fortunate that the AICA, a significant branch, was preserved in this patient (Figure 6).
Additionally, the subintimal tracking technique may result in subintimal hematomas, which could compress the distal true lumen and hinder attempts of re-entry[25]. As a result, careful guidewire manipulation is necessary to prevent expanding the subintimal space. At present, we recommend avoiding subintimal guidewire manipulation for chronic intracranial occlusion whenever feasible, particularly for neuro-interventionalists with limited expertise in CTO recanalization.
We present a fortuitous case of successful subintimal recanalization for non-acute occlusion of the intracranial vertebral artery in an emergency endovascular procedure. However, we emphasize the necessity for caution when applying the subintimal tracking approach in intracranial occlusion due to the significant dangers involved. Nevertheless, we are optimistic that this case study will be beneficial for furthering understanding of this topic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH, Indonesia; Sotelo J, Mexico S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Glass TA, Hennessey PM, Pazdera L, Chang HM, Wityk RJ, Dewitt LD, Pessin MS, Caplan LR. Outcome at 30 days in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2002;59:369-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 98] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Shin HK, Yoo KM, Chang HM, Caplan LR. Bilateral intracranial vertebral artery disease in the New England Medical Center, Posterior Circulation Registry. Arch Neurol. 1999;56:1353-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 60] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Caplan LR. The intracranial vertebral artery: a neglected species. The Johann Jacob Wepfer Award 2012. Cerebrovasc Dis. 2012;34:20-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Gao P, Wang Y, Ma Y, Yang Q, Song H, Chen Y, Jiao L, Qureshi AI. Endovascular recanalization for chronic symptomatic intracranial vertebral artery total occlusion: Experience of a single center and review of literature. J Neuroradiol. 2018;45:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Xu Z, Ma N, Mo D, Wong EH, Gao F, Jiao L, Miao Z. Endovascular recanalization for chronic symptomatic intracranial vertebral artery total occlusion. Minim Invasive Surg. 2014;2014:949585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Derdeyn CP, Fiorella D, Lynn MJ, Rumboldt Z, Cloft HJ, Gibson D, Turan TN, Lane BF, Janis LS, Chimowitz MI; Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis Trial Investigators. Mechanisms of stroke after intracranial angioplasty and stenting in the SAMMPRIS trial. Neurosurgery. 2013;72:777-95; discussion 795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Bolia A, Brennan J, Bell PR. Recanalisation of femoro-popliteal occlusions: improving success rate by subintimal recanalisation. Clin Radiol. 1989;40:325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 109] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Glasby MJ, Bolia A. Treatment of chronic mesenteric ischemia by subintimal angioplasty of an occluded superior mesenteric artery. Eur J Vasc Endovasc Surg. 2007;33:676-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Taylor MA, Vetrovec GW. Angioplasty of a totally occluded right coronary artery. Cathet Cardiovasc Diagn. 1992;25:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Chen YH, Leong WS, Lin MS, Huang CC, Hung CS, Li HY, Chan KK, Yeh CF, Chiu MJ, Kao HL. Predictors for Successful Endovascular Intervention in Chronic Carotid Artery Total Occlusion. JACC Cardiovasc Interv. 2016;9:1825-1832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 11. | Caplan LR, Wong KS, Gao S, Hennerici MG. Is hypoperfusion an important cause of strokes? Cerebrovasc Dis. 2006;21:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 115] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Wei LM, Zhu YQ, Zhang PL, Liu F, Lu HT, Zhao JG. Correction to: Morphological characteristics of chronic total occlusion: predictors of different strategies for long-segment femoral arterial occlusions. Eur Radiol. 2018;28:2708-2710. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Hou Z, Yan L, Zhang Z, Jing J, Lyu J, Hui FK, Fu W, Yu Y, Cui R, Wan M, Song J, Wang Y, Miao Z, Lou X, Ma N. High-resolution magnetic resonance vessel wall imaging-guided endovascular recanalization for nonacute intracranial artery occlusion. J Neurosurg. 2021:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 14. | Zhang J, Ding S, Zhao B, Sun B, Guo Q, Pan Y, Li X, Wang L, Zhang J, Tian J, Zhou Y, Xu J, Yuan C, Wan J, Zhao X, Zhao H. Morphological and Compositional Features of Chronic Internal Carotid Artery Occlusion in MR Vessel Wall Imaging Predict Successful Endovascular Recanalization. Diagnostics (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Srivatsa SS, Edwards WD, Boos CM, Grill DE, Sangiorgi GM, Garratt KN, Schwartz RS, Holmes DR Jr. Histologic correlates of angiographic chronic total coronary artery occlusions: influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J Am Coll Cardiol. 1997;29:955-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 182] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 16. | Aghaebrahim A, Jovin T, Jadhav AP, Noorian A, Gupta R, Nogueira RG. Endovascular recanalization of complete subacute to chronic atherosclerotic occlusions of intracranial arteries. J Neurointerv Surg. 2014;6:645-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Park Y, Park HS, Jang GL, Lee DY, Lee H, Lee JH, Kang HJ, Yang DH, Cho Y, Chae SC, Jun JE, Park WH. Intravascular ultrasound guided recanalization of stumpless chronic total occlusion. Int J Cardiol. 2011;148:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Wu EB, Brilakis ES, Mashayekhi K, Tsuchikane E, Alaswad K, Araya M, Avran A, Azzalini L, Babunashvili AM, Bayani B, Behnes M, Bhindi R, Boudou N, Boukhris M, Bozinovic NZ, Bryniarski L, Bufe A, Buller CE, Burke MN, Buttner A, Cardoso P, Carlino M, Chen JY, Christiansen EH, Colombo A, Croce K, de Los Santos FD, de Martini T, Dens J, di Mario C, Dou K, Egred M, Elbarouni B, ElGuindy AM, Escaned J, Furkalo S, Gagnor A, Galassi AR, Garbo R, Gasparini G, Ge J, Ge L, Goel PK, Goktekin O, Gonzalo N, Grancini L, Hall A, Hanna Quesada FL, Hanratty C, Harb S, Harding SA, Hatem R, Henriques JPS, Hildick-Smith D, Hill JM, Hoye A, Jaber W, Jaffer FA, Jang Y, Jussila R, Kalnins A, Kalyanasundaram A, Kandzari DE, Kao HL, Karmpaliotis D, Kassem HH, Khatri J, Knaapen P, Kornowski R, Krestyaninov O, Kumar AVG, Lamelas PM, Lee SW, Lefevre T, Leung R, Li Y, Lim ST, Lo S, Lombardi W, Maran A, McEntegart M, Moses J, Munawar M, Navarro A, Ngo HM, Nicholson W, Oksnes A, Olivecrona GK, Padilla L, Patel M, Pershad A, Postu M, Qian J, Quadros A, Rafeh NA, Råmunddal T, Prakasa Rao VS, Reifart N, Riley RF, Rinfret S, Saghatelyan M, Sianos G, Smith E, Spaedy A, Spratt J, Stone G, Strange JW, Tammam KO, Thompson CA, Toma A, Tremmel JA, Trinidad RS, Ungi I, Vo M, Vu VH, Walsh S, Werner G, Wojcik J, Wollmuth J, Xu B, Yamane M, Ybarra LF, Yeh RW, Zhang Q. Global Chronic Total Occlusion Crossing Algorithm: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;78:840-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 141] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 19. | Carlino M, Godino C, Latib A, Moses JW, Colombo A. Subintimal tracking and re-entry technique with contrast guidance: a safer approach. Catheter Cardiovasc Interv. 2008;72:790-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Munce NR, Strauss BH, Qi X, Weisbrod MJ, Anderson KJ, Leung G, Sparkes JD, Lockwood J, Jaffe R, Butany J, Teitelbaum AA, Qiang B, Dick AJ, Wright GA. Intravascular and extravascular microvessel formation in chronic total occlusions a micro-CT imaging study. JACC Cardiovasc Imaging. 2010;3:797-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Ritz K, Denswil NP, Stam OC, van Lieshout JJ, Daemen MJ. Cause and mechanisms of intracranial atherosclerosis. Circulation. 2014;130:1407-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 162] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 22. | Johnson CP, Baugh R, Wilson CA, Burns J. Age related changes in the tunica media of the vertebral artery: implications for the assessment of vessels injured by trauma. J Clin Pathol. 2001;54:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Masuoka T, Hayashi N, Hori E, Kuwayama N, Ohtani O, Endo S. Distribution of internal elastic lamina and external elastic lamina in the internal carotid artery: possible relationship with atherosclerosis. Neurol Med Chir (Tokyo). 2010;50:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Galassi AR, Tomasello SD, Costanzo L, Campisano MB, Barrano G, Ueno M, Tello-Montoliu A, Tamburino C. Mini-STAR as bail-out strategy for percutaneous coronary intervention of chronic total occlusion. Catheter Cardiovasc Interv. 2012;79:30-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 25. | Michael TT, Papayannis AC, Banerjee S, Brilakis ES. Subintimal dissection/reentry strategies in coronary chronic total occlusion interventions. Circ Cardiovasc Interv. 2012;5:729-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |