Published online Aug 16, 2023. doi: 10.12998/wjcc.v11.i23.5615
Peer-review started: June 8, 2023
First decision: July 4, 2023
Revised: July 11, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: August 16, 2023
Processing time: 69 Days and 3.4 Hours
Pancreatic cavernous hemangioma (pCH) is a rare type of benign vascular tumor. Making the right diagnosis is challenging due to low clinical suspicion and the lack of existing cross-sectional imaging tools to distinguish it from other pan
We describe a male patient, age 18, who presented with a pCH. Computed tomo
Chronic spontaneous hemorrhage may occur in pCH, which may greatly influ
Core Tip: Pancreatic cavernous hemangioma (pCH) is a rare type of benign vascular tumor, which is difficulty to correctly diagnose. The imaging features of pCH differ among the different cases. Herein, we present an 18-year-old male patient who was diagnosed with pCH after surgical resection. On the T2-weighted image of the magnetic resonance imaging, a dark spot sign was observed. The sign represented chronic intracapsular hemorrhage and was not reported before. We hope this case can help us gain knowledge about diagnosing pCH accurately.
- Citation: Li T. Pancreatic cavernous hemangioma complicated with chronic intracapsular spontaneous hemorrhage: A case report and review of literature. World J Clin Cases 2023; 11(23): 5615-5621
- URL: https://www.wjgnet.com/2307-8960/full/v11/i23/5615.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i23.5615
Pancreatic cavernous hemangioma (pCH) is an extremely uncommon tumor with no acknowledged typical imaging characteristics in the current literature[1]. As a result, modern imaging may not sufficiently define this benign illness because hemangiomas closely resemble frequent pancreatic tumors, especially when the pCH is complicated by other clinical conditions. In this work, we report an 18-year-old male who failed to be correctly diagnosed preoperatively by imaging modalities. For this patient, pCH complicated with chronic intracapsular spontaneous hemorrhage was confirmed by pathological specimens after surgical resection.
An 18-year-old male patient with an abdominal cyst lesion found during a physical examination one year ago was referred to our hospital for reexamination of the tumor, which was enlarged.
There was no abdominal pain, diarrhea, or significant change in body weight during the course of the disease.
The patient did not receive any relevant treatment before hospitalization and had no history of surgery or medication.
The patient denied any family medical history.
No positive physical examination sign was identified.
Complete blood counts, aspartate aminotransferase, alkaline phosphatase, bilirubin, serum electrolytes, creatinine, urea, glucose, and serum tumor marker levels were all within normal ranges.
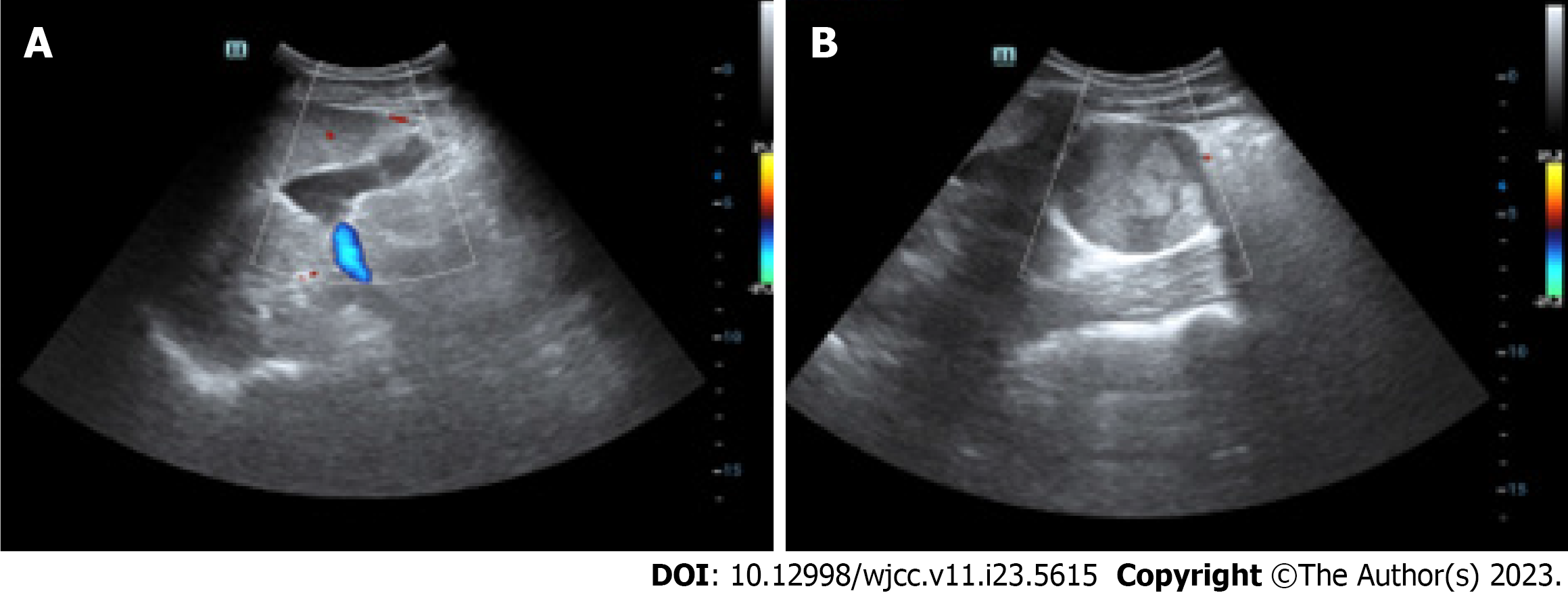
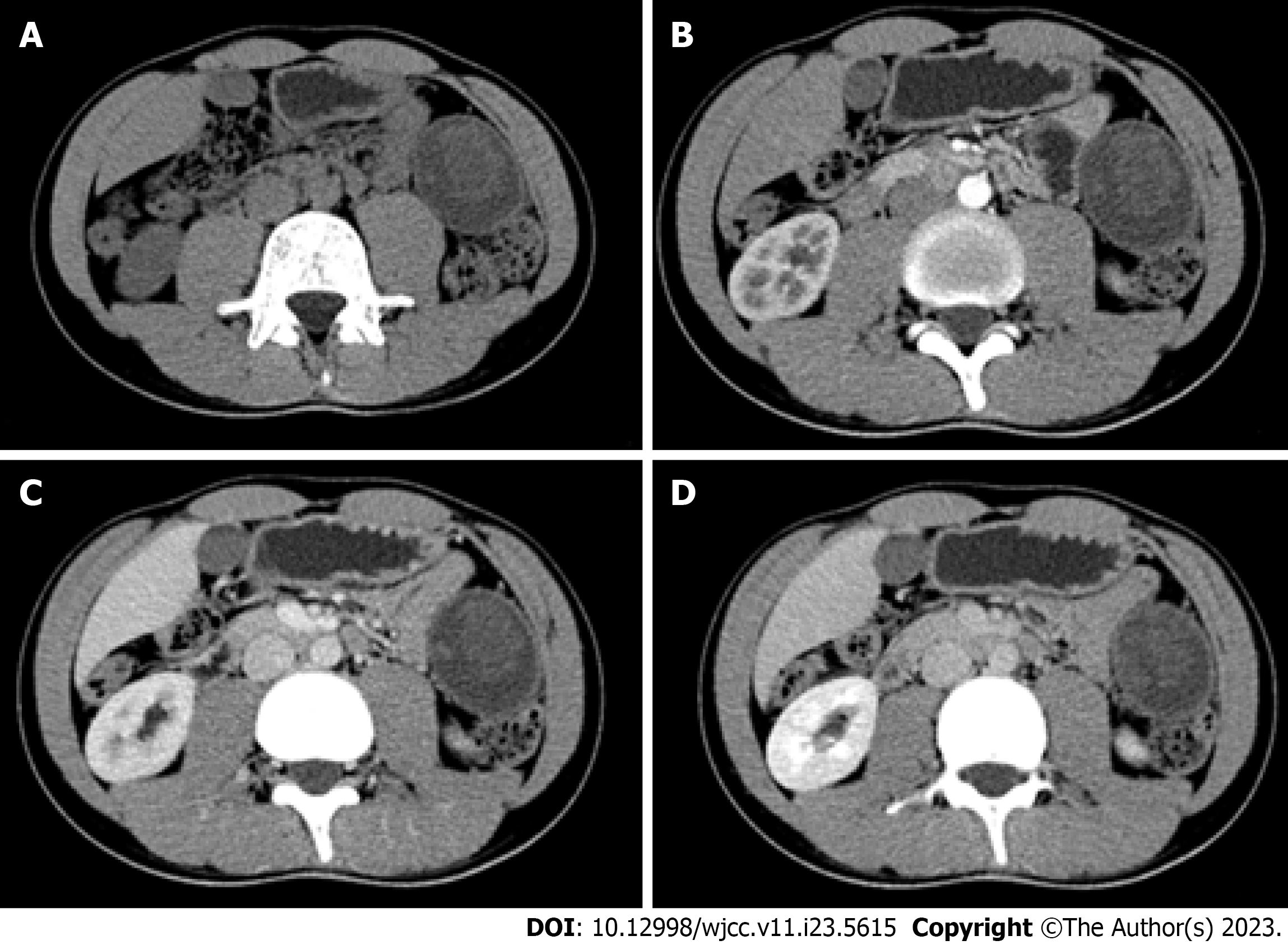
Trans-abdominal ultrasound (US) revealed a cystic solid mass with clear margins in the left abdomen, and no obvious blood flow signal was observed in color Doppler flow imaging. Moreover, there was no echo zone between the mass and spleen (Figure 1). A computed tomography (CT) scan revealed an irregular mixed density mass in the splenorenal space of the left upper abdomen, with uneven cystic density and punctate calcification in the cyst wall. The tumor enhancement was not obvious on the contrast-enhanced CT (Figure 2). Magnetic resonance imaging (MRI) showed a round T1 and T2 hypersignal mass, which was about 64 mm × 51 mm in size, in the splenorenal space of the left upper abdomen. The multiple quasi-circular lesions with a high T1 weighted image (WI) signal, low T2WI signal, and slightly low signal fat suppression sequence were seen inside the tumor. No obvious enhancement was observed in the lesions; the cyst wall was slightly enhanced; and fine line enhancement was observed in the delayed period of enhanced scanning (Figure 3). Localized fluid signals were seen around the lesion. Notably, the “dark spot” sign was observed on T2WI.
The term “pancreas hemangioma” was used in a literature search on PubMed and Google Scholar, and relevant papers and their references were examined. In total, 23 works on pCH have been published since 1960[1,4-25], including one case of a child[6]. Finally, 22 cases were enrolled for further analysis.
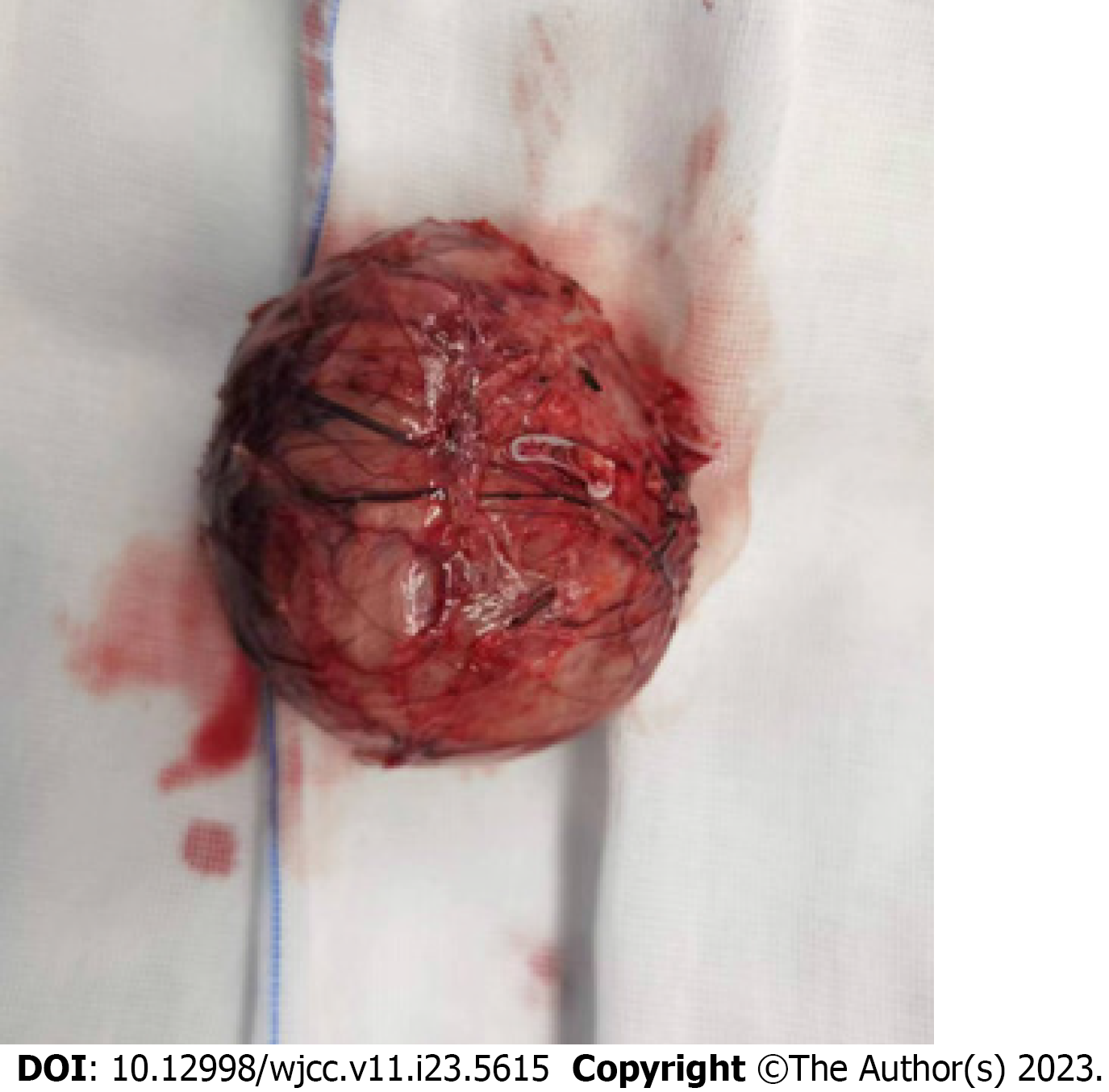
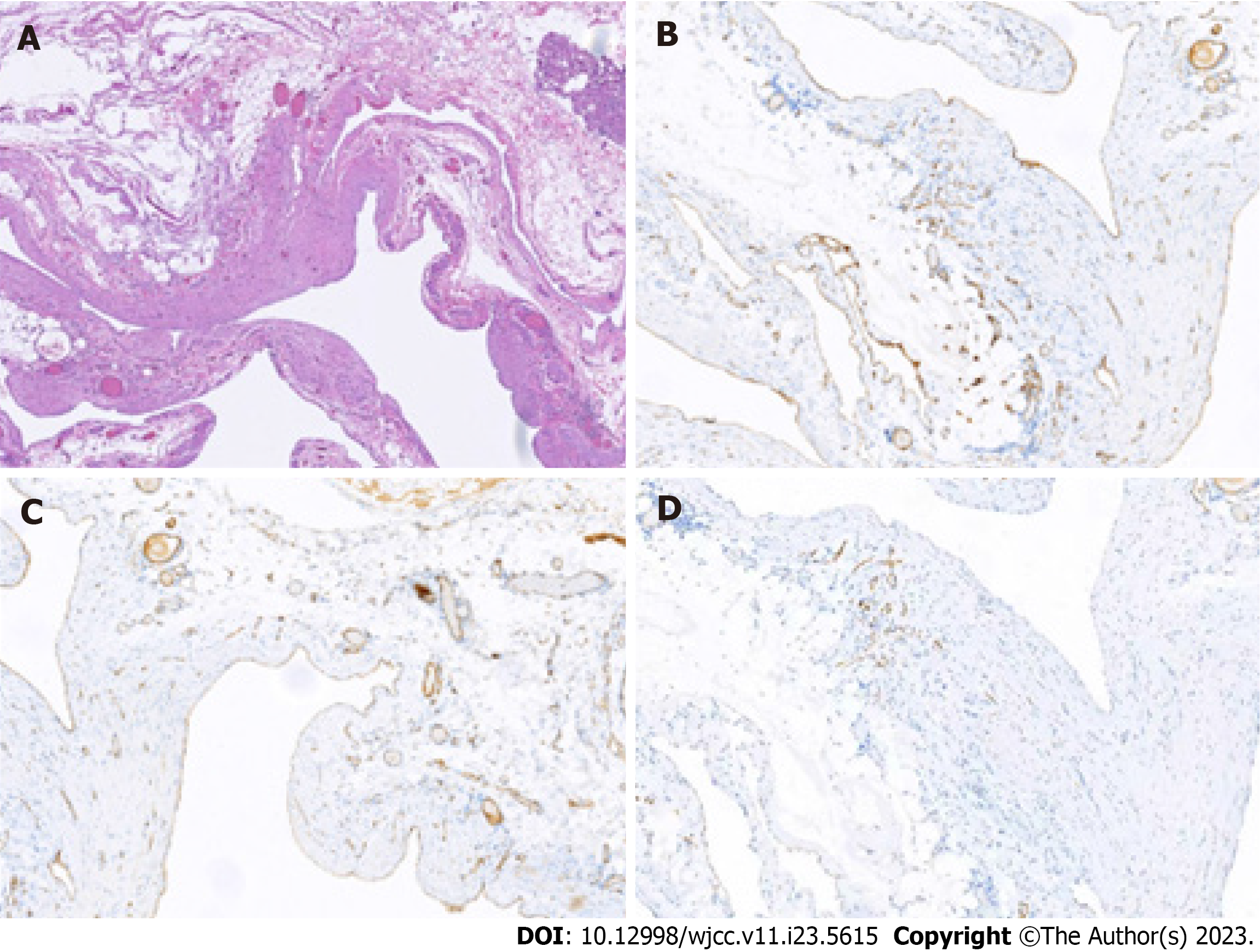
Pathological specimen examination revealed a soft, sac-like red mass (Figure 4). The patient’s pathology corresponds to a chronic retraction blood clot and contains hemosiderin. Microscopically, a monolayer of endothelial cells was observed. Immunohistochemical staining for CD31 and CD34 was positive; D2-40 was positive in interstitial lymphatic vessels and negative in vascular epithelial cells; and calcium-binding protein was negative. The results support the diagnosis of a hemangioma (Figure 5).
The diagnosis of mucinous cystic neoplasm with chronic bleeding was proposed after the clinical presentations combined with imaging presentations were taken into consideration. The patient was recommended for surgery according to the Fukuoka guidelines[2]. Finally, we performed a distal pancreatic tumor resection under laparoscopic guidance. The tumor was located in the region of the pancreatic tail and spleen hilum, extending upward to the rear of the splenic vein, and connected to the splenic region of the colon and duodenum below with a relatively clear space and no obvious infiltration. The operation was successful, and no surgery-related complications occurred.
After surgery, the patient had one day of observation in the intensive care unit. He was able to tolerate drinking liquids orally on the second day. On the seventh post-operative day, he was allowed to go home. He had no symptoms or signs of a recurrence six months following surgery, according to CT scans and telephone follow-up.
Hemangioma is a tumor formed by the proliferation of angioblast cells during the embryo development that can occur anywhere in the body. Pancreatic hemangiomas are rare, making up about 0.1% of pancreatic tumors[3]. pCH, a type of pancreatic hemangioma, is even rarer and still has an unknown pathogenesis[4].
According to the literature review, the age of onset of adult pCH is between 18 and 79 years old, and the ratio of male to female is about 1:3. pCH occurs most frequently in the head of the pancreas, followed by the tail and body; although, some cases have also occurred in the neck of the pancreas. pCHs exhibit no specific symptoms and have been found due to the non-specific abdominal symptoms, including pain, fever, nausea, vomiting, dizziness, and jaundice. Some pCHs were accidentally discovered during physical examination. Notably, one case with massive upper gastrointestinal bleeding was found to be associated with pCH[16].
The conventional imaging modalities used to diagnose pCH are transabdominal US, CT, endoscopic US (EUS), and MRI. In 10 cases, hemangiomas larger than 5 cm were detected by US. Moreover, US and EUS imaging are generally a hyperechoic no blood flow signal or a mild blood flow signal mass. If there is calcification in the lesion, a strong echo can be observed[17]. In contrast to a mucinous cystic tumor, the lack of a fine speckled internal echo pattern may indicate a vascular tumor[12]. However, in our case, the imaging feature was not present, and no Doppler signal was detected. Poor Doppler signals may be caused by hemorrhage, thrombosis, necrosis, shunting, and the vascularity of the solid com
It is pertinent to mention the usefulness of EUS in diagnosing pancreatic lesions. EUS is rarely performed in teenage patients, and the imaging features of EUS may be similar to that of US. Fine needle aspiration may not be applicable in pCH cases due to the risk of bleeding. Moreover, only one study reported the use of EUS in diagnosing pCH[9]. Therefore, the feature of EUS cannot be summarized, and the role of EUS should be explored in future studies.
According to the CT imaging findings of hepatic cavernous hemangiomas, the tumors are generally circular with smooth edges, strong peripheral enhancement in the arterial phase of enhanced scanning, and gradual filling of the contrast medium in the delayed scanning[26]. However, preoperative diagnosis of pCH was proposed in one study based on these characteristics. Hemangiomas cannot be ruled out by a three-phase contrast CT scan that is not enhanced, which was the case in our report. The reason remains unclear, and thus, we should not heavily rely on CT imaging to diagnose pCHs.
Hemangiomas on MRIs show up as a lobulated, hypointense mass on T1WIs and as a moderately hyperintense signal on T2WI[27,28]. Only three studies reported MRI findings: Low T1W signal attenuation was observed in two cases[10,12], and high T2W signal attenuation was observed in another two cases[10,11]. The imaging feature was similar to ours[10,11]. Moreover, the “dark spot” sign was observed on the T2WI sequence. The dark spot sign is an extremely low signal on the T2WIs of cystic lesions, which is specific for chronic hemorrhagic disease and can be seen in hemorrhagic tumors[29]. This article is the first to describe the T2 black spot sign in pCH, which could be attributed to the chronic retraction clots that shorten the T2 relaxation time and the features identified by pathological analysis.
Due to the small number of cases of pCH without special clinical manifestations and atypical imaging features, it is easy to preoperatively misdiagnose. In the majority of cases, surgery was performed without a confirmed diagnosis. pCHs provide imaging features that are similar to the radiographic phenotypes of other frequent pancreatic lesions. It should also be distinguished from pancreatic cystic lesions[30], pancreatic neuroendocrine tumors[31], paraganglioma[32] and pancreatic cancer. We can judge benign and malignant tumors through a combination of clinical manifestations, imaging examination, laboratory tumor markers, and fine needle aspiration.
It is crucial to obtain an accurate histological diagnosis of a hemangioma since other vascular tumors can require a greater surgical margin during resection, adjuvant medication, or a more intensive post-resection follow-up. One study reported recurrence rates of 10%-27% and 50%-100% after total and partial resection in hemolymphangioma, respectively[33]. Hemangiomas consist of an increased number of ectatic capillaries that are filled with blood, have flat endothelium lining them, and are divided by sparse fibrous connective tissue stroma. Vascular spaces may be of the capillary or cavernous kind, depending on their size. Hemangioma, lymphangioma, and other benign vascular tumors are indicated by the presence of vascular endothelial markers (CD31, CD34, and factor VIII-related antigen) coupled with negative cytokeratin (AE1/AE3, D2-40, CAM 5.2, and MNF 116) immunohistochemical staining findings.
Hemangiomas in childhood cannot be treated with tumor resection because they can resolve spontaneously. However, the natural history of adult pCHs remains unclear as they do not present any malignant potential and seem to develop quite slowly. If a certain diagnosis is established prior to surgery, a conservative strategy might be taken into account. For large hemangiomas with persistent diagnostic ambiguity, uncontrolled symptoms after ineffective conservative therapy, or problems resulting from mass impact, surgical excision seems to be a suitable course of action. Successful outcomes were achieved for all patients who had pCHs removed. Similarly, no recurrence was observed in our case after follow-up for 6 mo.
In this study, we present a misdiagnosed adult pCH patient case who underwent surgical resection. We propose a novel imaging feature that may aid the correct diagnosis of pCH. The review of literature may constantly help to improve our understanding of this disease and to summarize its clinical and imaging characteristics. As a result, the precise treatment may be achieved.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia; Sperti C, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Huang JY, Yang R, Li JW, Lu Q, Luo Y. Cavernous hemangioma of an intrapancreatic accessory spleen mimicking a pancreatic tumor: A case report. World J Clin Cases. 2022;10:1973-1980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Reference Citation Analysis (0)] |
| 2. | Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K; International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 1613] [Article Influence: 124.1] [Reference Citation Analysis (0)] |
| 3. | Vieira RMF, Souza Junior AS, Kerche LE. Cystic pancreatic lesions: imaging versus anatomopathological findings-how to improve diagnostic accuracy? Arq Bras Cir Dig. 2023;36:e1735. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Ringoir S, Derom F, Colle R, Mortier G. Hemangioma of the pancreas. Report of a case. Gastroenterology. 1961;41:43-45. [PubMed] |
| 5. | Bursics A, Gyökeres T, Bély M, Pörneczi B. Adult hemangioma of the pancreas: difficult diagnosis of a rare disease. Clin J Gastroenterol. 2013;6:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | England RJ, Woodley H, Cullinane C, McClean P, Walker J, Stringer MD. Pediatric pancreatic hemangioma: a case report and literature review. JOP. 2006;7:496-501. [PubMed] |
| 7. | Søreide JA, Greve OJ, Gudlaugsson E. Adult pancreatic hemangioma in pregnancy--concerns and considerations of a rare case. BMC Surg. 2015;15:119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Mundinger GS, Gust S, Micchelli ST, Fishman EK, Hruban RH, Wolfgang CL. Adult pancreatic hemangioma: case report and literature review. Gastroenterol Res Pract. 2009;2009:839730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Mondal U, Henkes N, Henkes D, Rosenkranz L. Cavernous hemangioma of adult pancreas: A case report and literature review. World J Gastroenterol. 2015;21:9793-9802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Lu ZH, Wu M. Unusual features in an adult pancreatic hemangioma: CT and MRI demonstration. Korean J Radiol. 2013;14:781-785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Naito Y, Nishida N, Nakamura Y, Torii Y, Yoshikai H, Kawano H, Akiyama T, Sakai T, Taniwaki S, Tanaka M, Kuroda H, Higaki K. Adult pancreatic hemangioma: A case report. Oncol Lett. 2014;8:642-644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Chang WT, Lee KT, Yang SF. Cavernous hemangioma of the pancreas: report of a case. Pancreas. 2003;26:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Colardyn F, Elewaut A, Van de Velde E, Barbier F. Hemangioma of the pancreas. Tijdschr Gastroenterol. 1972;15:260-267. [PubMed] |
| 14. | Lee J, Raman K, Sachithanandan S. Pancreatic hemangioma mimicking a malignant pancreatic cyst. Gastrointest Endosc. 2011;73:174-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Lu T, Yang C. Rare case of adult pancreatic hemangioma and review of the literature. World J Gastroenterol. 2015;21:9228-9232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Koo CH, Koh YX, Hennedige T, Thng CH, Chung AY. Pancreatic Haemangioma: An Unusual Case of Massive Upper Gastrointestinal Bleeding with Clinical and Radiological Correlation of the Literature and Recommendations. Ann Acad Med Singap. 2018;47:345-348. [PubMed] |
| 17. | Jin C, Mo JG, Jiang H, Wang LZ, Zou H, Wang KP. Adult pancreatic hemangioma: a rare case report and literature review. BMC Surg. 2020;20:118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Kobayashi H, Itoh T, Murata R, Tanabe M. Pancreatic cavernous hemangioma: CT, MRI, US, and angiography characteristics. Gastrointest Radiol. 1991;16:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Weidenfeld J, Zakai BB, Faermann R, Barshack I, Aviel-Ronen S. Hemangioma of pancreas: a rare tumor of adulthood. Isr Med Assoc J. 2011;13:512-514. [PubMed] |
| 20. | Raymundo SRO, Hussain KMK, Hussein KG, Kuga ML. Rare case of adult pancreatic haemangioma and literature review. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Zhou J, Chen Z. Rare adult pancreatic hemangioma: review of the literature with a case report. Gland Surg. 2020;9:1596-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Jarboui S, Salem A, Gherib BS, Ben Moussa M, Rajhi H, Mnif N, Zaouche A. Hemangioma of the pancreas in a 60-year-old woman: a report of a new case. Gastroenterol Clin Biol. 2010;34:569-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Williamson JM, Finch-Jones M, Pope I. Endoscopic ultrasonography allowing expectant management of pancreatic haemangioma. Ann R Coll Surg Engl. 2014;96:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Kim SH, Kim JY, Choi JY, Choi YD, Kim KS. Incidental detection of pancreatic hemangioma mimicking a metastatic tumor of renal cell carcinoma. Korean J Hepatobiliary Pancreat Surg. 2016;20:93-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Jeong MA, Lee JK, Nam JH, Jang DK, Lim YJ, Lee JJ, Kim EJ. Pancreatic Hemangioma Suspected of Neuroendocrine Tumor. Korean J Gastroenterol. 2020;76:46-48. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Aziz H, Brown ZJ, Baghdadi A, Kamel IR, Pawlik TM. A Comprehensive Review of Hepatic Hemangioma Management. J Gastrointest Surg. 2022;26:1998-2007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 27. | Semelka RC, Brown ED, Ascher SM, Patt RH, Bagley AS, Li W, Edelman RR, Shoenut JP, Brown JJ. Hepatic hemangiomas: a multi-institutional study of appearance on T2-weighted and serial gadolinium-enhanced gradient-echo MR images. Radiology. 1994;192:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 222] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 28. | Goshima S, Kanematsu M, Kondo H, Yokoyama R, Kajita K, Tsuge Y, Shiratori Y, Onozuka M, Moriyama N. Hepatic hemangioma: correlation of enhancement types with diffusion-weighted MR findings and apparent diffusion coefficients. Eur J Radiol. 2009;70:325-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Corwin MT, Gerscovich EO, Lamba R, Wilson M, McGahan JP. Differentiation of ovarian endometriomas from hemorrhagic cysts at MR imaging: utility of the T2 dark spot sign. Radiology. 2014;271:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 30. | Taouli B, Vilgrain V, Vullierme MP, Terris B, Denys A, Sauvanet A, Hammel P, Menu Y. Intraductal papillary mucinous tumors of the pancreas: helical CT with histopathologic correlation. Radiology. 2000;217:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 135] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Bian Y, Li J, Jiang H, Fang X, Cao K, Ma C, Lu J. Tumor Size on Microscopy, CT, and MRI Assessments Versus Pathologic Gross Specimen Analysis of Pancreatic Neuroendocrine Tumors. AJR Am J Roentgenol. 2021;217:107-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Moor R, Goutnik M, Lucke-Wold B, Laurent D, Chen S, Friedman W, Rahman M, Allen N, Rivera-Zengotita M, Koch M. Clival Paraganglioma, Case Report and Literature Review. OBM Neurobiol. 2022;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 33. | Fang YF, Qiu LF, Du Y, Jiang ZN, Gao M. Small intestinal hemolymphangioma with bleeding: a case report. World J Gastroenterol. 2012;18:2145-2146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |