Published online Aug 6, 2023. doi: 10.12998/wjcc.v11.i22.5391
Peer-review started: May 21, 2023
First decision: June 13, 2023
Revised: June 25, 2023
Accepted: July 17, 2023
Article in press: July 17, 2023
Published online: August 6, 2023
Processing time: 73 Days and 18.3 Hours
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is an acute, self-limiting vasculitis of unknown aetiology that mainly involves the medium and small arteries and can lead to serious cardiovascular complications, with a 25% incidence of coronary artery aneurysms. Periton–Sillar abscesses are a rare symptom of KD and is easily misdiagnosed at its early stages.
A 5-year-old boy who presented to a community hospital with a 3-d fever, difficulty in opening his mouth, and neck pain and was originally treated for throat infection without improvement. On the basis of laboratory tests, ultrasound of submandibular and superficial lymph nodes and computed tomography of the neck, the clinician diagnosed the periamygdala abscess and sepsis that did not resolve after antibiotic therapy. On the fifth day of admission, the child developed conjunctival congestion, prune tongue, perianal congestion and desquamation, and slightly stiff and swollen bunions on both feet. A diagnosis of KD was reached with complete remission after intravenous immunoglobulin treatment.
Children with neck pain, lymph node enlargement, or airway obstruction as the main manifestations are poorly treated with intravenous broad-spectrum antibiotics. Clinicians should not rush invasive operations such as neck puncture, incision, and drainage and should be alert for KD when it cannot be explained by deep neck space infection and early treatment with aspirin combined with gammaglobulin.
Core Tip: Some typical symptoms of a suppurative infection of the deep neck fever, for example elevated white blood cell count, lymph node enlargement, and abnormal changes in the head and neck, may also be atypical manifestations of Kawasaki disease (KD). For cases with a long course of fever and no response to antibiotic treatment, careful observation of symptoms, signs, and cervical imaging findings in the progression of the disease can be used to detect KD with deep neck changes as the first symptom early and avoid the occurrence of serious complications.
- Citation: Huo LM, Li LM, Peng HY, Wang LJ, Feng ZY. Kawasaki disease with peritonsillar abscess as the first symptom: A case report. World J Clin Cases 2023; 11(22): 5391-5397
- URL: https://www.wjgnet.com/2307-8960/full/v11/i22/5391.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i22.5391
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is an acute, self-limiting vasculitis of unknown aetiology that mainly involves the medium and small arteries and can lead to serious cardiovascular complications, with a 25% incidence of coronary artery aneurysms. Periton–Sillar abscesses are a rare symptom of KD and is easily misdiagnosed at its early stages. There are a few children with early meningitis, parotitis, changes in renal function indicators, pancreatitis, cholecystitis, intestinal obstruction[1,2]. Rare symptoms such as inflammatory changes in the parapharyngeal space or postpharyngeal space, rather than typical KD clinical manifestations, often lead to clinical misdiagnosis, delayed diagnosis and unnecessary treatment. In this paper, we report a case of KD with peri-tonsillar abscess as the first presentation and review the literature to summarise the clinical features and treatment course to improve the ability of clinicians to identify the disease early.
A 5-year-old boy presented with a 3-d history of fever, neck pain, and difficulty in opening his mouth. After anti-infective symptomatic treatment at the community hospital, the child’s fever and sore throat did not improve. The boy was admitted to our hospital on May 20, 2021, for further treatment.
On admission, the patient had a febrile temperature of 40 ℃, a heart rate of 100 beats/min, and a respiratory rate of 40 breaths/min. Congestion and swelling were observed in the neck and behind the ear, with significant tenderness causing the child to resist manipulation of the area. An enlarged lymph node measuring approximately 1.5 cm × 1 cm was palpable under the right jaw. The bilateral Bulbar conjunctiva was mildly congested, the pharynx was congested, tonsils were enlarged to degree II, and no herpes or exudate was seen.
The laboratory tests showed the following: white blood cell count, 10.27 × 109/L; neutrophil percentage, 80.3%; lymphocyte percentage, 10.0%; C-reactive protein 21.49 mg/L; and erythrocyte sedimentation rate 56.00 mm/h. A blood smear showed no significant abnormalities.
An ultrasound showed cortical thickening of multiple lymph nodes adjacent to cervical vessels bilaterally, including both posterior cervical and left submandibular nodes, with the largest lymph node measuring 2.4 cm × 1.0 cm.
KD.
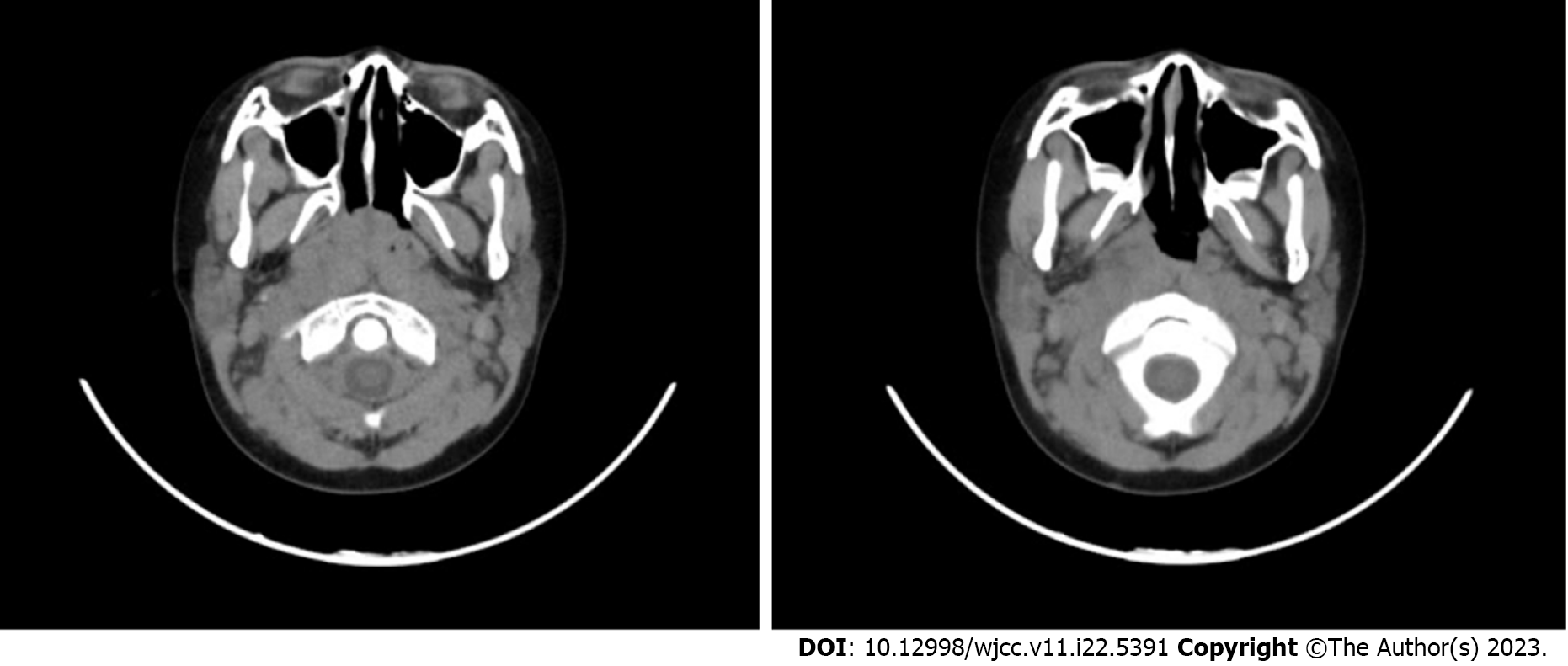
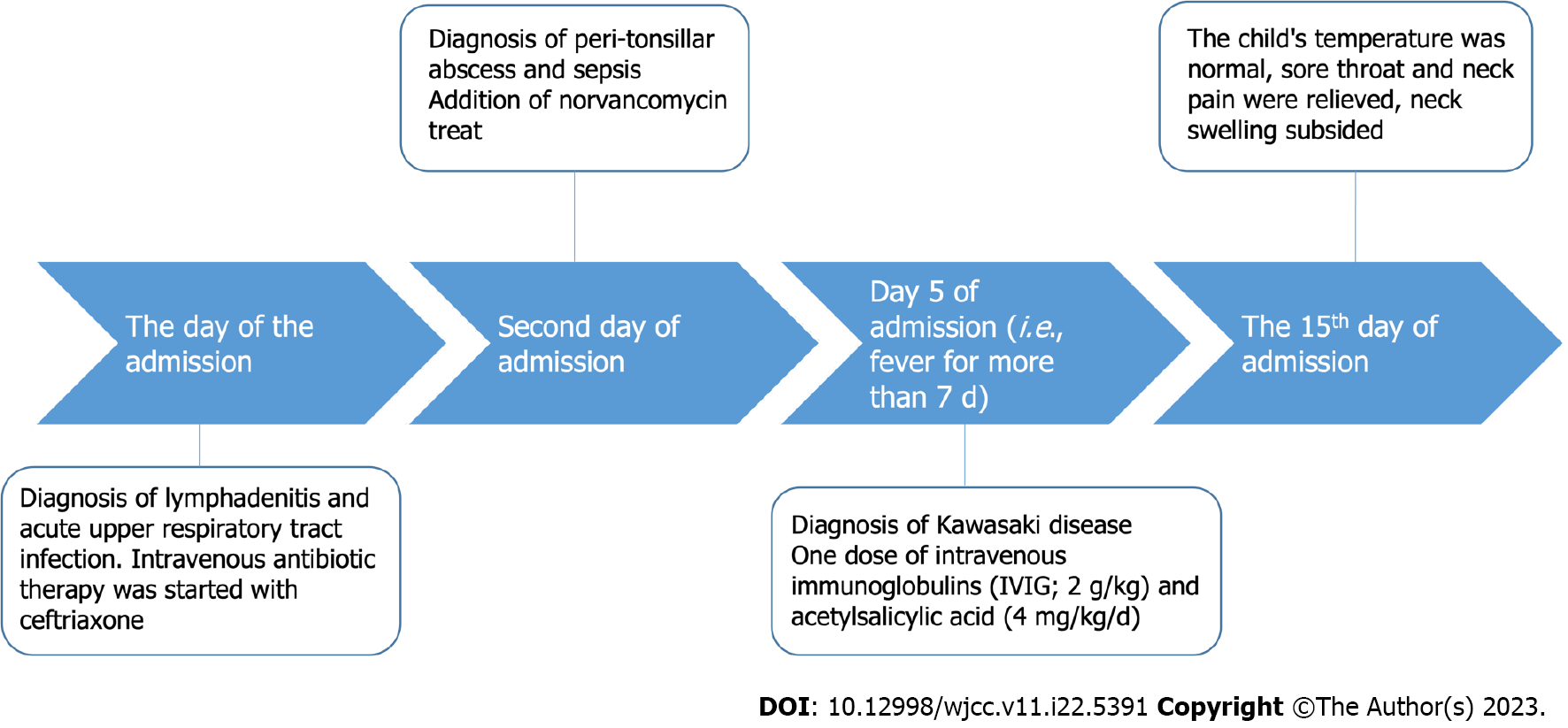
On the first day of hospitalisation, intravenous antibiotic therapy was initiated with ceftriaxone, based on the suspicion of lymphadenitis and acute upper respiratory tract infection. The child had persistent high fever with chills, and computed tomography (CT) of the neck showed a widening of the retropharyngeal space with liquid hypodensity, thickening of the pharyngeal lymphatic ring, and multiple slightly large lymph nodes in the neck space (Figure 1). Based on these findings, the diagnoses were modified to peri-tonsillar abscess and sepsis, which were treated with norvancomycin. On the fifth day of admission (i.e., after more than seven days with fever), the child developed conjunctival congestion, prune tongue, perianal congestion and desquamation, and slightly stiff and swollen bunions on both feet. Based on this clinical presentation and lack of response to antibiotics, the patient was diagnosed with KD. Echocardiography performed on the same day did not reveal any coronary artery abnormalities. One dose of intravenous immunoglobulin (IVIG; 2 g/kg) was administered with rapid defervescence, and acetylsalicylic acid (4 mg/kg/day) was started and continued at home for 8 wk. On day 15, a CT scan of the neck suggested that multiple small lymph nodes in the neck were reduced in size compared to the previous film, and the oropharyngeal and retropharyngeal space effusion had disappeared (Figure 2). The child’s temperature was normal, his sore throat and neck pain were relieved, and the neck swelling subsided. No coronary artery dilatation was detected on cardiac ultrasound during hospitalisation; therefore, the child was discharged in good general condition. After discharge, the boy continued to take aspirin 100 mg 1/d orally for 2 mo. The timeline of diagnosis and treatment of KD in this child (Figure 3).
Six months later, the child was followed-up. The family complained that the child's temperature was normal, there was no swelling or pain in the neck, and the blood count was normal. Cardiac ultrasound showed no abnormalities in the morphology, structure, or function of the heart.
Deep-neck infections occur primarily in the underlying deep cervical space formed by the deep cervical fascia, including the parapharyngeal, retropharyngeal, submandibular, and parotid spaces. Peritonsillar, parapharyngeal, and retropharyngeal involvement with oedema, cellulitis, and abscess-like lesions are rare but possible manifestations of KD. According to a cross-sectional study in the United States, approximately 0.6% of patients with KD have a combination of deep cervical space involvement[3]. A Japanese study found that 3.6% of patients with KD had CT scans suggestive of hypodense lesions in the retropharyngeal space[4]. Roh et al[5] found that 61% (34/56) of the cases were finally diagnosed with KD in 56 cases with fever, cervical lymphadenopathy as the main clinical manifestation, and CT enhancement of the neck suggesting retropharyngeal hypointense shadow). Another Korean study proposed that 25% of patients newly diagnosed with deep cervical space infection according to neck CT examination were diagnosed with KD[6].
The pathogenesis of KD remains unclear, and its epidemiology in recent years is highly suggestive of infection-related pathogenesis. A single-retrospective study found the presence of infection in 33% of patients with KD[7]. The microorganisms currently reported to be associated with KD include bacteria, viruses, Mycoplasma pneumoniae, and Chlamydia. The microbial toxin-like superantigen pathogenesis theory and pathogenic role of bacteria mimicking the host's own antigens may play an important role in pathogenesis. The main bacterial species associated with upper respiratory tract infections and peri-tonsillar abscesses include streptococci, Staphylococcus aureus, and oropharyngeal anaerobes. The microbiological mechanisms of KD and deep cervical space infections share similar pathogenic bacterial profiles. Katano et al[8] detected the streptococcal genomes in the cervical lymph nodes of patients with KD. Therefore, scholars have suggested that bacterial infection may be involved in KD pathogenesis with deep cervical space involvement, but no bacteria have been found in the cervical puncture drainage fluid of patients with KD combined with cervical space involvement[9-11]. In view of this, anti-infective treatment may also be necessary. However, antibiotic treatment is ineffective, and aspirin and gamma globulin are still needed to relieve the typical symptoms of KD.
The diagnostic criteria for KD include clinical features that are common to other febrile illnesses in children. KD is sometimes confused with bacterial infections, which leads to antibiotic therapy in patients with KD. In actual clinical practice, a high percentage of patients with KD receive antibiotic therapy because of empirical diagnoses and misdiagnoses. It has been reported that more than half of the patients (54.3%) received antibiotics before receiving standard treatment for KD[11]. A retrospective study reported that 33% of patients had a confirmed infection at the time of KD diagnosis, but (64%) (83/129) of patients received oral antibiotics for suspected infection prior to the diagnosis of KD[7]. When KD is combined with head and neck complications, the first symptoms are fever with limited neck movement, neck swelling and pain, slumped neck, and painful swallowing[12-16], and these clinical manifestations are very similar to those of cervical infections. Patients with KD and combined cervical involvement receive antibiotics more frequently and have a longer treatment time compared to those without combined cervical involvement[17]. However, KD coinfection does not affect the patient’s response to treatment or coronary prognosis.
A peri-tonsillar abscess following acute tonsillitis is often associated with sore throat, dysphagia, restricted mouth opening, slurred pronunciation on the affected side, erythema, and elevation of the soft palate on examination[18]. In addition to clinical manifestations, enhanced CT has a higher sensitivity for the diagnosis of peritonsillar abscesses[19]. The initial presentation in our case was fever, enlarged lymph nodes and tonsils, neck pain, and difficulty in opening the mouth. CT of the cervical region showed a widening of the posterior oropharyngeal space with fluid hypodensity, thickening of the pharyngeal lymphatic ring, and multiple, slightly large lymph nodes in the cervical space. The child was considered to have a peri-tonsillar abscess, but anti-infective treatment was ineffective. It was not until the child presented with typical KD features (fever for more than seven days, visible conjunctival congestion, prune tongue, perianal congestion and desquamation, and slightly stiff and swollen bunions) that the diagnosis of KD was confirmed and treated with aspirin combined with gammaglobulin. The temperature decreased to normal after 1 d of aspirin and gammaglobulin treatment. Therefore, in infants and children with an initial diagnosis of peri-tonsillar abscess, KD needs to be considered as a possibility, especially if antibiotic therapy is not effective.
KD is a febrile multisystem vasculitis of unknown aetiology that primarily affects the coronary arteries and may result in serious cardiovascular disease if not diagnosed and treated promptly. Although antimicrobial therapy does not lead to a poor prognosis, delayed treatment and misdiagnosis may lead to poor prognosis in KD. Early recognition in clinical workup, especially in the differential diagnosis of infectious diseases, is particularly important. CT or magnetic resonance imaging (MRI) can be used for differential diagnosis. From an imaging perspective, septic infections and cellulitis changes have different presentations. In the case of septic changes, CT is mainly characterised by marginal strengthening hypointense images, whereas in patients with KD with deep neck changes, CT is mainly characterised by retropharyngeal hypointensity without marginal strengthening[20-22]. On MRI, septic neck infection is mainly characterised by central T1 hypo, T2 hyper, and peripheral marginal strengthening[23]. In some cases, CT and MRI of the cervical region can be used to differentiate deep cervical lesions of KD from bacterial septic infections.
It is difficult to distinguish patients with early KD and peri-tonsillar abscesses as the first manifestation of peritonsillar abscesses due to infection, thus leading to treatment with local incision and drainage or even tonsillectomy. Ravi and Brooks reported a 7-year-old child with clinically diagnosed tonsillar abscess who underwent right tonsillectomy on day 6 after admission and was diagnosed with KD on day 2 postoperatively, with resolution of symptoms after treatment with aspirin and intravenous gammaglobulin[24]. Cai et al[25] reported a 3-year-old child with parapharyngeal swelling secondary to KD who underwent parapharyngeal abscess incision and drainage on day 3 of admission, and for whom KD was diagnosed on day 8 of admission, with the symptoms resolving after treatment with aspirin and intravenous gammaglobulin. A 14-year-old male was initially diagnosed with a peri-tonsillar abscess, and the patient presented with clinical manifestations typical of KD before surgical treatment was performed[26]. All of these cases which initially lacked the typical clinical manifestations of KD, were typically treated with local surgery. Deep abscess-like lesions in the neck develop from local inflammation and oedema in the setting of systemic vasculitis, and these abscess-like lesions are absorbed and disappear with IVIG and aspirin therapy. Therefore, delayed surgical treatment is essential in these patients.
In our case, even after imaging, we had difficulty ruling out a cervical infection and instead added anti-infective treatment with norvancomycin. The diagnosis of KD was not confirmed until the child presented with typical KD features. The child received aspirin combined with gammaglobulin for one day to reduce his temperature to normal.
Children with neck pain, lymph node enlargement, or airway obstruction as the main manifestations are poorly treated with intravenous broad-spectrum antibiotics. Clinicians should not rush invasive operations such as neck puncture, incision, and drainage and should be alert for KD when it cannot be explained by deep neck space infection or early treatment with aspirin combined with gammaglobulin.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dauyey K, Kazakhstan; Kim BS, South Korea S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Zhang B, Hao Y, Zhang Y, Yang N, Li H, Liang J. Kawasaki disease manifesting as bilateral facial nerve palsy and meningitis: a case report and literature review. J Int Med Res. 2019;47:4014-4018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Lai CC, Lin WT, Lin HC. Parotitis: An Initial Manifestation of Kawasaki Disease. J Pediatr. 2019;214:235-235.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Inagaki K, Blackshear C, Hobbs CV. Deep Neck Space Involvement of Kawasaki Disease in the US: A Population-Based Study. J Pediatr. 2019;215:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Tona R, Shinohara S, Fujiwara K, Kikuchi M, Kanazawa Y, Kishimoto I, Harada H, Naito Y. Risk factors for retropharyngeal cellulitis in Kawasaki disease. Auris Nasus Larynx. 2014;41:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Roh K, Lee SW, Yoo J. CT analysis of retropharyngeal abnormality in Kawasaki disease. Korean J Radiol. 2011;12:700-707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Lim S, Lee NY, Han SB, Jeong DC, Kang JH. Deep Neck Inflammation: Probable Kawasaki Disease in Korean Children. Clin Exp Otorhinolaryngol. 2020;13:77-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Benseler SM, McCrindle BW, Silverman ED, Tyrrell PN, Wong J, Yeung RS. Infections and Kawasaki disease: implications for coronary artery outcome. Pediatrics. 2005;116:e760-e766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Katano H, Sato S, Sekizuka T, Kinumaki A, Fukumoto H, Sato Y, Hasegawa H, Morikawa S, Saijo M, Mizutani T, Kuroda M. Pathogenic characterization of a cervical lymph node derived from a patient with Kawasaki disease. Int J Clin Exp Pathol. 2012;5:814-823. [PubMed] |
| 9. | Pontell J, Rosenfeld RM, Kohn B. Kawasaki disease mimicking retropharyngeal abscess. Otolaryngol Head Neck Surg. 1994;110:428-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Principi N, Esposito S. Antibiotic-related adverse events in paediatrics: unique characteristics. Expert Opin Drug Saf. 2019;18:795-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Langley EW, Kirse DK, Barnes CE, Covitz W, Shetty AK. Retropharyngeal edema: an unusual manifestation of Kawasaki disease. J Emerg Med. 2010;39:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Isidori C, Sebastiani L, Esposito S. A Case of Incomplete and Atypical Kawasaki Disease Presenting with Retropharyngeal Involvement. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Aldemir-Kocabaş B, Kcal MM, Ramoğlu MG, Tutar E, Fitöz S, Çiftçi E, İnce E. Recurrent Kawasaki disease in a child with retropharyngeal involvement: a case report and literature review. Medicine (Baltimore). 2014;93:e139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Hung MC, Wu KG, Hwang B, Lee PC, Meng CC. Kawasaki disease resembling a retropharyngeal abscess--case report and literature review. Int J Cardiol. 2007;115:e94-e96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Homicz MR, Carvalho D, Kearns DB, Edmonds J. An atypical presentation of Kawasaki disease resembling a retropharyngeal abscess. Int J Pediatr Otorhinolaryngol. 2000;54:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Kasem Ali Sliman R, van Montfrans JM, Nassrallah N, Hamad Saied M. Retropharyngeal abscess-like as an atypical presentation of Kawasaki disease: a case report and literature review. Pediatr Rheumatol Online J. 2023;21:34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | Cheng XY. Analysis of clinical features of Kawasaki disease combined with deep cervical space involvement. Master Thesis, China Medical University, China, 2021. [DOI] [Full Text] |
| 18. | AlAwadh I, Aldrees T, AlQaryan S, Alharethy S, AlShehri H. Bilateral peritonsillar abscess: A case report and pertinent literature review. Int J Surg Case Rep. 2017;36:34-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Baker KA, Stuart J, Sykes KJ, Sinclair KA, Wei JL. Use of computed tomography in the emergency department for the diagnosis of pediatric peritonsillar abscess. Pediatr Emerg Care. 2012;28:962-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Nomura O, Hashimoto N, Ishiguro A, Miyasaka M, Nosaka S, Oana S, Sakai H, Takayama JI. Comparison of patients with Kawasaki disease with retropharyngeal edema and patients with retropharyngeal abscess. Eur J Pediatr. 2014;173:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Vural C, Gungor A, Comerci S. Accuracy of computerized tomography in deep neck infections in the pediatric population. Am J Otolaryngol. 2003;24:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Tsujioka Y, Handa A, Nishimura G, Miura M, Yokoyama K, Sato K, Handa H, Jinzaki M, Nosaka S, Kono T. Multisystem Imaging Manifestations of Kawasaki Disease. Radiographics. 2022;42:268-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Chiappini E, Camaioni A, Benazzo M, Biondi A, Bottero S, De Masi S, Di Mauro G, Doria M, Esposito S, Felisati G, Felisati D, Festini F, Gaini RM, Galli L, Gambini C, Gianelli U, Landi M, Lucioni M, Mansi N, Mazzantini R, Marchisio P, Marseglia GL, Miniello VL, Nicola M, Novelli A, Paulli M, Picca M, Pillon M, Pisani P, Pipolo C, Principi N, Sardi I, Succo G, Tomà P, Tortoli E, Tucci F, Varricchio A, de Martino M; Italian Guideline Panel For Management Of Cervical Lymphadenopathy In Children. Development of an algorithm for the management of cervical lymphadenopathy in children: consensus of the Italian Society of Preventive and Social Pediatrics, jointly with the Italian Society of Pediatric Infectious Diseases and the Italian Society of Pediatric Otorhinolaryngology. Expert Rev Anti Infect Ther. 2015;13:1557-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Ravi KV, Brooks JR. Peritonsillar abscess--an unusual presentation of Kawasaki disease. J Laryngol Otol. 1997;111:73-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Cai Q, Luo R, Gan J, Zhang L, Qu Y, Mu D. Kawasaki disease mimicking a parapharyngeal abscess: a case report. Medicine (Baltimore). 2015;94:e761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Connell JT, Park JH. Acute peritonsillar swelling: a unique presentation for Kawasaki disease in adolescence. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |