Published online Jul 26, 2023. doi: 10.12998/wjcc.v11.i21.5173
Peer-review started: May 19, 2023
First decision: June 13, 2023
Revised: June 21, 2023
Accepted: July 4, 2023
Article in press: July 4, 2023
Published online: July 26, 2023
Processing time: 68 Days and 12.6 Hours
Subarachnoid-pleural fistula (SPF) is a complex and rare condition characterized by a pathological shunt between the subarachnoid and pleural spaces. It can lead to the accumulation of cerebrospinal fluid (CSF) in the pleural space, pneumocephalus, and the development of central nervous system infection. Trauma or thoracic spinal surgery are common causes of SPF, with symptoms including pos
We report a case of an 83-year-old male patient with traumatic SPF and bilateral frontal subdural hygroma following a fall from height. The patient initially presented with severe lower back and buttock pain. During admission, the patient developed worsening lower limb weakness and pleural effusion. Further investigation revealed the presence of subdural hygromas with mass effect, requiring emergency bilateral subdural drainage. A multidisciplinary approach was under
Traumatic SPF with subsequent subdural hygroma is a rare but serious combi
Core Tip: We present here a case of traumatic subarachnoid-pleural fistula in combination with bilateral frontal subdural hygroma. We also searched the existing literature to provide an evidence-based discussion of the correlation between these two clinical events.
- Citation: Chen PH, Li CR, Gan CW, Yang TH, Chang CS, Chan FH. Rare combination of traumatic subarachnoid-pleural fistula and intracranial subdural hygromas: A case report. World J Clin Cases 2023; 11(21): 5173-5178
- URL: https://www.wjgnet.com/2307-8960/full/v11/i21/5173.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i21.5173
Subarachnoid-pleural fistula (SPF) is an uncommon and complex disease. Pathologic shunt between the subarachnoid and pleural spaces can lead to cerebrospinal fluid (CSF) accumulation in the pleural space, pneumocephalus, and the development of central nervous system infection. A history of trauma or thoracic spinal surgery are common among patients with SPF[1-4]. Depending upon the fistula grade, imaging typically reveals blunting of the costophrenic angle or widening of the mediastinum due to persistent draining of the CSF into the pleural space. Pneumothorax or hemothorax are seen more frequently in spinal injury cases or iatrogenic cases.
Symptoms of SPF include postural headache, level of consciousness changes, and dyspnea. Meningitis, encephalitis, or aggressive chest infection may develop subsequent to persistent CSF leakage and pleural effusion accumulation. These scenarios often lead to catastrophic events. Therefore, early recognition of SPF and immediate surgical and/or non-surgical interventions are important priorities[5-7].
According to the present literature, traumatic SPFs are more scarce than iatrogenic cases. The combination of prominent intracranial hygromas and trauma-related SPF has never been reported before. In this article, we present a case of traumatic SPF followed by bilateral frontal subdural hygroma. In addition to the clinical illustration of the severe combination of SPF and subdural hygroma, we also searched the existing literature and discussed the correlation between these clinical events.
An 83-year-old male patient was sent to the emergency department for severe lower back and buttock pain.
The patient had recently fallen from a height of 3 meters.
The patient self-reported a medical history of hypertension, diabetes mellitus, and ankylosing spondylitis, all of which were controlled by the appropriate medicines.
There was no notable personal or family history.
The patient presented with alert consciousness, having glasgow coma scale score of E4V5M6. Normal findings for examinations of the level of consciousness, cranial nerves, motor and sensory systems, and coordination were documented.
Laboratory examinations revealed a slightly elevated C-reactive protein level (3.42 mg/dL; normal range: 0-0.748 mg/dL).
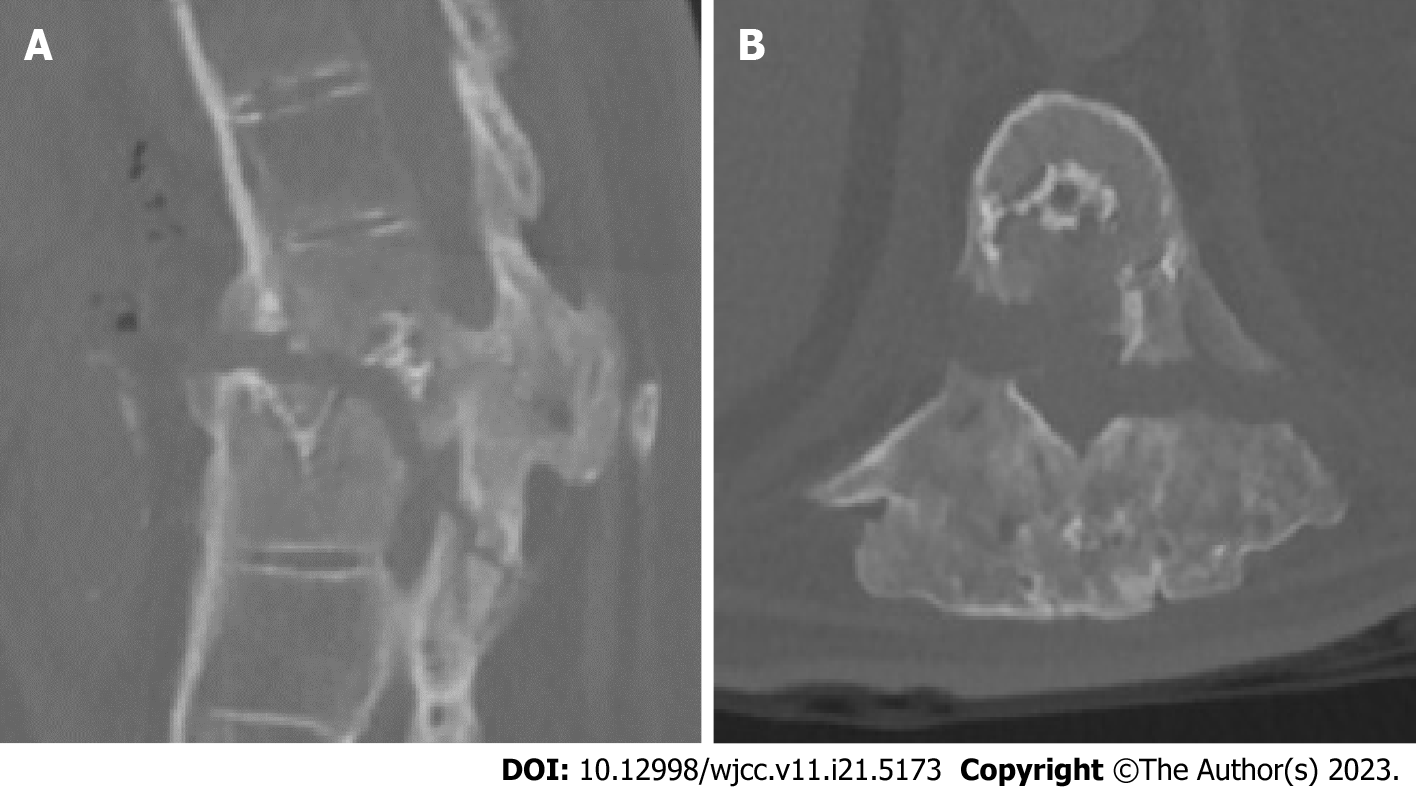
Chest X-ray showed a T10-T11 fracture and blunting of the costophrenic angle on the left side with suspected hemothorax. Chest computed tomography (CT) revealed left-side hemothorax and T10-T11 chance fracture with spinal cord compression (Figure 1).
Traumatic chest injury with SPF.
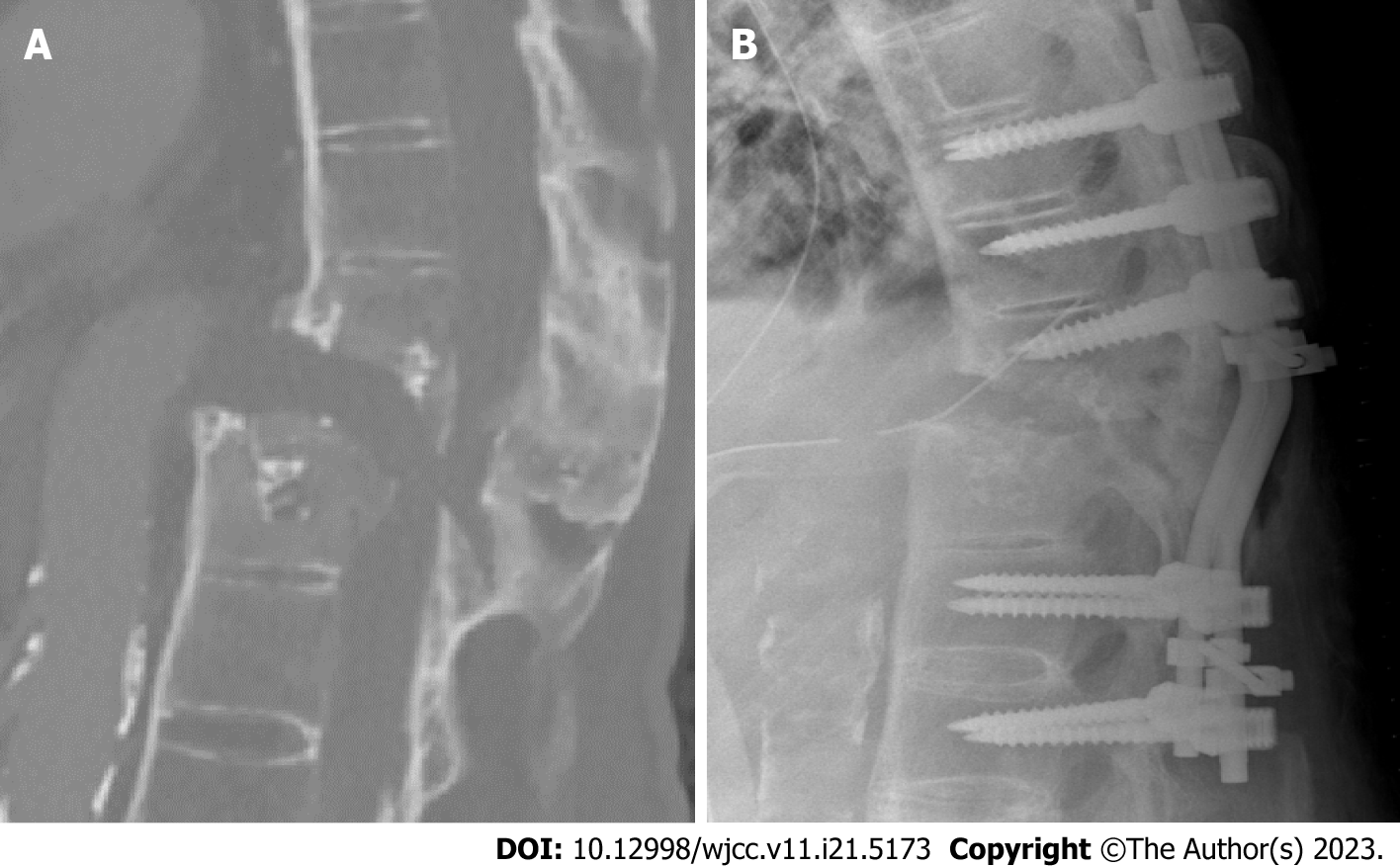
Emergency video-assisted thoracoscopic surgery and left chest tube insertion for massive hemothorax were performed. In addition, surgical management of the T10-T11 fracture was suggested. However, the patient and his family were hesitant about the operation. After admission to the intensive care unit, the patient experienced worsening lower limb weakness (muscle power grading 2 bilaterally) after 3 d. A repeat thoracic spinal CT revealed an aggravated fracture and spinal cord stretching (Figure 2A). Emergency surgery of T11 and partial T12 laminectomy and bilateral T9-T10-T11-L1-L2 transpedicular screw fixation were performed (Figure 2B).
The patient was transferred to the general ward 2 wk postoperatively, under relatively stable condition. However, frequent serous oozing from the chest tube insertion wound was noted. Daily chest tube drainage increased from 200 mL to 450 mL. It was suspected that the patient was experiencing aggravation of the pleural effusion. Right-side pigtail insertion was performed, and the effusion analysis revealed a transudative quality with a positive finding of glucose. Broad-spectrum antibiotics were administered due to suspicion of an SPF. Furthermore, the patients’ level of consciousness continued to decline [glasgow coma scale (GCS) E1VTM4] 5 d after transferring to the general ward.
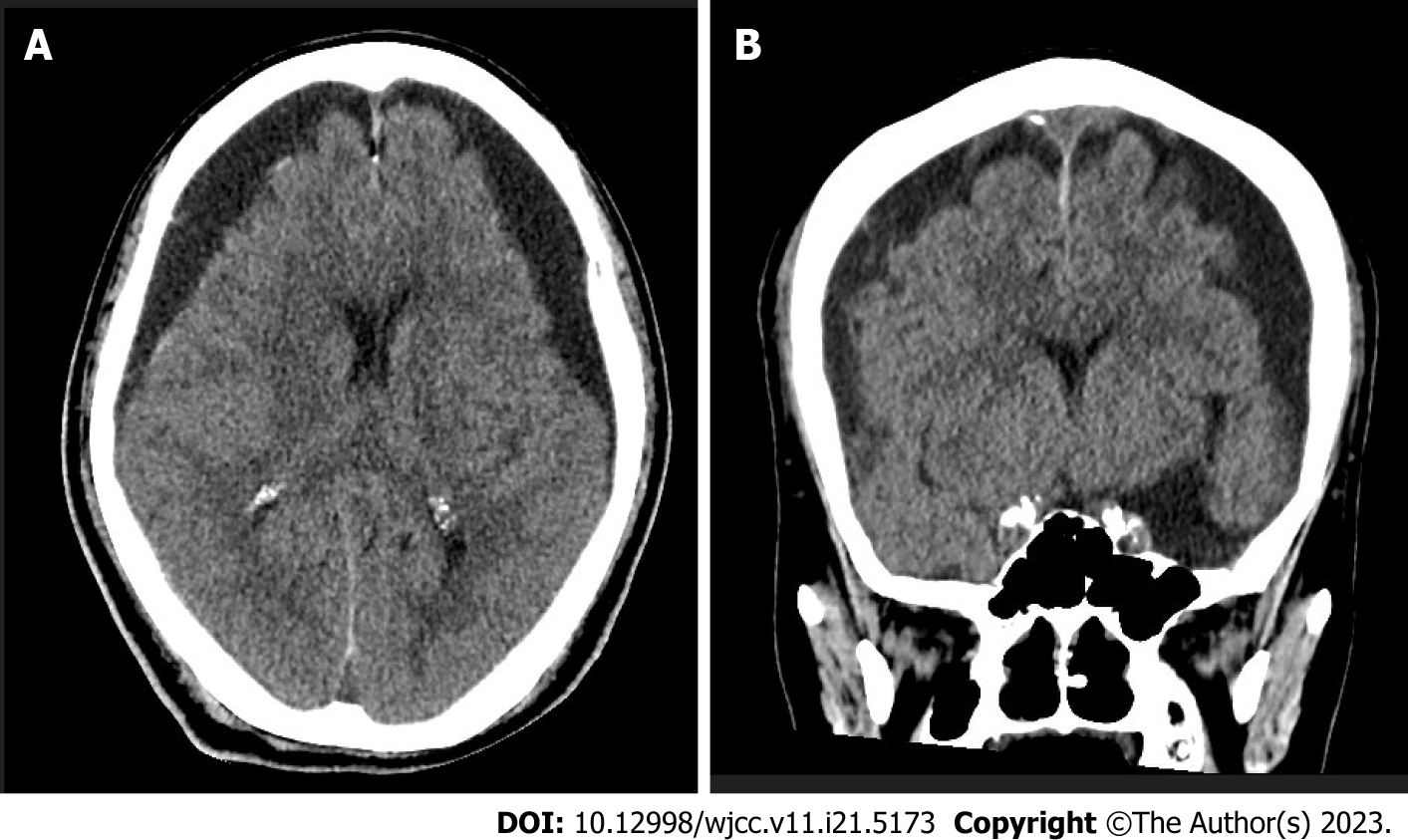
Brain CT investigation showed bilateral subdural hygromas with a mass effect (Figure 3). Bilateral subdural drainage was performed for decompression. The intraoperative hygroma specimen revealed similar components as the CSF.
The patient recovered well postoperatively. The patient’s GCS returned to E3VTM5, and the subdural drainage tubes were removed 1 wk postoperatively. The chest tube and pigtail were eventually removed after clinical condition improvement.
There are few published reports of traumatic CSF leakage, and incidence remains unknown. In a current review article, Wallace et al[8] reported a 4% incidence of CSF leakage in stab injuries, whereas Luszczyk et al[9] found that approximately 10% of individuals with thoracic spine fractures experienced CSF leakage.
In cases of persistent CSF leakage from the spinal canal to the pleural space following trauma, communicating fistulae can develop. Peter and Rode[10] proposed subtypes of SPFs to aid in the investigation of this condition. Type I SPFs are solely characterized by continuous CSF leakage and pleural effusion, while type II SPFs may also be associated with tension pneumothorax and subarachnoid air.
The most frequent clinical manifestation of SPF is a postural headache due to intracranial hypotension. A subsequent mental change may imply deterioration of the clinical condition, such as a subdural hematoma caused by a tear in a cortical bridging vein or an ongoing infection. According to the literature, Chadduck[11], Ladehoff et al[12] separately documented 2 cases of cerebellar hemorrhage following iatrogenic SPF related to downward cerebellar herniation and accompanied by CSF hypovolemia. In addition, Khurana et al[13] described 2 cases of sixth cranial nerve palsy sub
There is currently no gold standard algorithm for the diagnosis and management of SPFs. Non-surgical treatment, including broad-spectrum antibiotics, are typically initiated if there is suspicion of central nervous system infection or infection at the chest tube insertion site[10-14]. Surgical management is indicated for progressive symptoms or failure to respond to conservative management. Feasible surgical options include direct closure of the fistula, placement of plugging materials with autologous blood patch[15], or placement of a thrombin-coated sponge[16]. Additionally, Knafo et al[17] successfully used percutaneous injection of onyx (an ethylene-vinyl alcohol copolymer manufactured by ev3, Irvine, CA, United States) to obliterate an SPF.
Subdural hygromas are frequently associated with spontaneous intracranial hypotension[18]. Lin et al[19] described a case of intracranial subdural hygroma after endoscopic lumbar spinal surgery. A retrospective review from 2008 to 2013 of 1113 consecutive patients who underwent spinal surgery found 4 patients (0.27%) with intracranial hygromas[20]. Another review article showed that typical magnetic resonance imaging findings of subdural hygromas included subdural fluid accumulation, engorgement of venous structures, and sagging of the brain[21].
We documented that our patient experienced progressive consciousness disturbance and increasing pleural effusion drainage in the 3 wk after a fall from height. Imaging revealed bilateral frontal subdural hygromas. We hypothesize that the arachnoid membrane tearing was caused by hypovolemic CSF or by passive effusion aggravation associated with persistent low intracranial pressure.
In this case report, we highlighted a rare but serious combination of traumatic SPF with subsequent subdural hygroma. Although the optimal treatment strategy for this complex condition remains uncertain, our literature review suggested that a multidisciplinary approach, including intervention for hypovolemic CSF and management of the subdural hygroma, is the most beneficial. Further research is needed to better understand the pathophysiology of traumatic SPFs and to guide the development of more targeted and optimized treatment approaches.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vyshka G, Albania; Yarmahmoodi F, Iran S-Editor: Qu XL L-Editor: A P-Editor: Cai YX
| 1. | Monla-Hassan J, Eichenhorn M, Spickler E, Talati S, Nockels R, Hyzy R. Duropleural fistula manifested as a large pleural transudate: an unusual complication of transthoracic diskectomy. Chest. 1998;114:1786-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Jahn K, Winkler K, Tiling R, Brandt T. Intracranial hypotension syndrome due to duropleural fistula after thoracic diskectomy. J Neurol. 2001;248:1101-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Hentschel SJ, Rhines LD, Wong FC, Gokaslan ZL, McCutcheon IE. Subarachnoid-pleural fistula after resection of thoracic tumors. J Neurosurg. 2004;100:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Nyunoya T, Gross T, Rooney C, Mendoza S, Kline J. Massive pleural transudate following a vertebral fusion in a 49-year-old woman. Chest. 2003;123:1280-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Shamji MF, Sundaresan S, Da Silva V, Seely J, Shamji FM. Subarachnoid-pleural fistula: applied anatomy of the thoracic spinal nerve root. ISRN Surg. 2011;2011:168959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Yang W, Ge M, Chen C, Zeng Q. Diagnose and treatment of traumatic pleural-subarachnoid fistula in children: A case report and systematic review. Chin Neurosurg J. 2020;6:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Alnajdi N, Darwish A, Alharbi A, Khairo M, Brinji Z, Rawah E. Pneumocephalus resulting from chest infection complicated by pleural-subarachnoid fistula. Radiol Case Rep. 2021;16:2012-2016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Wallace DJ, Sy C, Peitz G, Grandhi R. Management of non-missile penetrating spinal injury. Neurosurg Rev. 2019;42:791-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Luszczyk MJ, Blaisdell GY, Wiater BP, Bellabarba C, Chapman JR, Agel JA, Bransford RJ. Traumatic dural tears: what do we know and are they a problem? Spine J. 2014;14:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Peter JC, Rode H. Traumatic subarachnoid-pleural fistula: case report and review of the literature. J Trauma. 1993;34:303-304. [PubMed] |
| 11. | Chadduck WM. Cerebellar hemorrhage complicating cervical laminectomy. Neurosurgery. 1981;9:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Ladehoff M, Zachow D, Koch C, Nowak G, Echelmeyer A, Arnold H, Giese A. Cerebellar haemorrhage and tension pneumocephalus after resection of a Pancoast tumour. Acta Neurochir (Wien). 2005;147:561-564; discussion 564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Khurana A, Brousil J, Russo A, Evans A, Quraishi NA, Boszczyk BM. Intracranial hypotension with a sixth cranial nerve palsy subsequent to massive thoracic CSF hygroma: a rare complication of thoracic disc excision. Eur Spine J. 2013;22:2047-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ramirez-Ferrer E, Abaunza-Camacho JF, Pineda-Martinez AF, Aguilera-Pena MP, Riveros-Castillo WM, Laverde-Frade L. Cerebrospinal fluid leak following penetrating trauma to the spine without neurological deficit: A case report. Surg Neurol Int. 2022;13:327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Salerni AA, Kuivila TE, Drvaric DM, Deutsch SD, Knuckey NW. Traumatic subarachnoid-pleural fistula in a child. A case report. Clin Orthop Relat Res. 1991;184-188. [PubMed] |
| 16. | Sarwal V, Suri RK, Sharma OP, Baruah A, Singhi P, Gill S, Bapuraj JR. Traumatic subarachnoid-pleural fistula. Ann Thorac Surg. 1996;62:1622-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Knafo S, Parker F, Herbrecht A, Court C, Saliou G. Percutaneous treatment of subarachnoid-pleural fistula with Onyx. J Neurosurg Spine. 2013;18:378-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Smith KA. Spontaneous intracranial hypotension: Targeted or blind blood patch. J Clin Neurosci. 2016;25:10-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Lin GX, Chen CM, Kim JS, Song KS. The Transformation of Intracranial Subdural Hygroma to Chronic Subdural Hematoma Following Endoscopic Spinal Surgery: A Case Report. J Neurol Surg A Cent Eur Neurosurg. 2022;83:502-506. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Pham MH, Tuchman A, Platt A, Hsieh PC. Intracranial complications associated with spinal surgery. Eur Spine J. 2016;25:888-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 667] [Cited by in RCA: 694] [Article Influence: 36.5] [Reference Citation Analysis (0)] |