Published online Jul 16, 2023. doi: 10.12998/wjcc.v11.i20.4883
Peer-review started: March 14, 2023
First decision: April 19, 2023
Revised: May 8, 2023
Accepted: June 21, 2023
Article in press: June 21, 2023
Published online: July 16, 2023
Processing time: 119 Days and 14.2 Hours
The gold standard treatment for papillary thyroid carcinoma is total thyroidectomy and indications for microwave thermal ablation for primary thyroid cancers have not yet been clearly established However, some patients refuse surgery and others have no indication for it, for example patients under palliative care as in this case, or cannot undergo surgery, based on their comorbidities. These indications are described in the most recent Korean, North American and European guidelines. Laser ablation, radiofrequency ablation, and microwave ablation are similarly safe and effective, so the choice should be based on the specific competences and resources of the pertaining centers. These indications are Percutaneous minimally-invasive techniques; they can be useful to stop disease progression and as an alternative to surgery in patients with contraindication or who refuse surgery. We present a case of a thyroid papillary carcinoma with 17 mm effectively treated with microwave thermal ablation and without recurrence after one year of follow up.
The authors present a case of a 71-years-old patient with a left lobe papillary thyroid carcinoma with 13 mm × 17 mm × 13 mm, with no indication for thyroid surgery given the context of another cancer in palliative treatment. Microwave thermoablation was performed on December 2021. Four months later he repeated computed tomography (CT) scan, which showed that the tumor had disappeared. Six months after ablation he underwent a positron emission tomography/CT-fluorodeoxyglucose scan, which didn’t show any evidence of hypermetabolic tumor lesions.
This case shows microwave thermoablation can be a safe and effective alternative to surgery in patients with no conditions to undergo surgery or when they refuse it. By treating the tumor, with this minimally invasive technique, we are stopping its growth and avoiding disease progression.
Core Tip: The authors present a case of a well succeeded treatment with microwave thermoablation of a papillary thyroid carcinoma, in a patient with no indication for thyroid surgery given the context of another neoplastic disease in palliative treatment.
- Citation: Dionísio T, Lajut L, Sousa F, Violante L, Sousa P. Microwave ablation of solitary T1N0M0 papillary thyroid carcinoma: A case report. World J Clin Cases 2023; 11(20): 4883-4889
- URL: https://www.wjgnet.com/2307-8960/full/v11/i20/4883.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i20.4883
Surgery was historically the treatment of choice for most thyroid cancers[1,2]. However, microwave thermal ablation has become a minimally invasive option for patients who have no indication or cannot undergo surgery, avoiding disease progression[1,3,10].
We present a case of a thyroid papillary carcinoma with 17 mm effectively treated with microwave thermal ablation, without major complications and without recurrence after one year of follow up.
71 years old male patient with lung adenocarcinoma T4N0M0 initially treated with chemotherapy and radiotherapy. Because of disease progression patient restarted chemotherapy.
During follow up, the patient was referred for a positron emission tomography-computed tomography-fluorodeoxyglucose scan (18F-FDG PET-CT) scan, which showed focal and intense uptake of 18F-FDG in the left lobe of the thyroid gland. An ultrasound-guided biopsy confirmed the presence of an 13 mm × 17 mm ×13 mm (corresponding to a volume of 1.4 mL) papillary carcinoma.
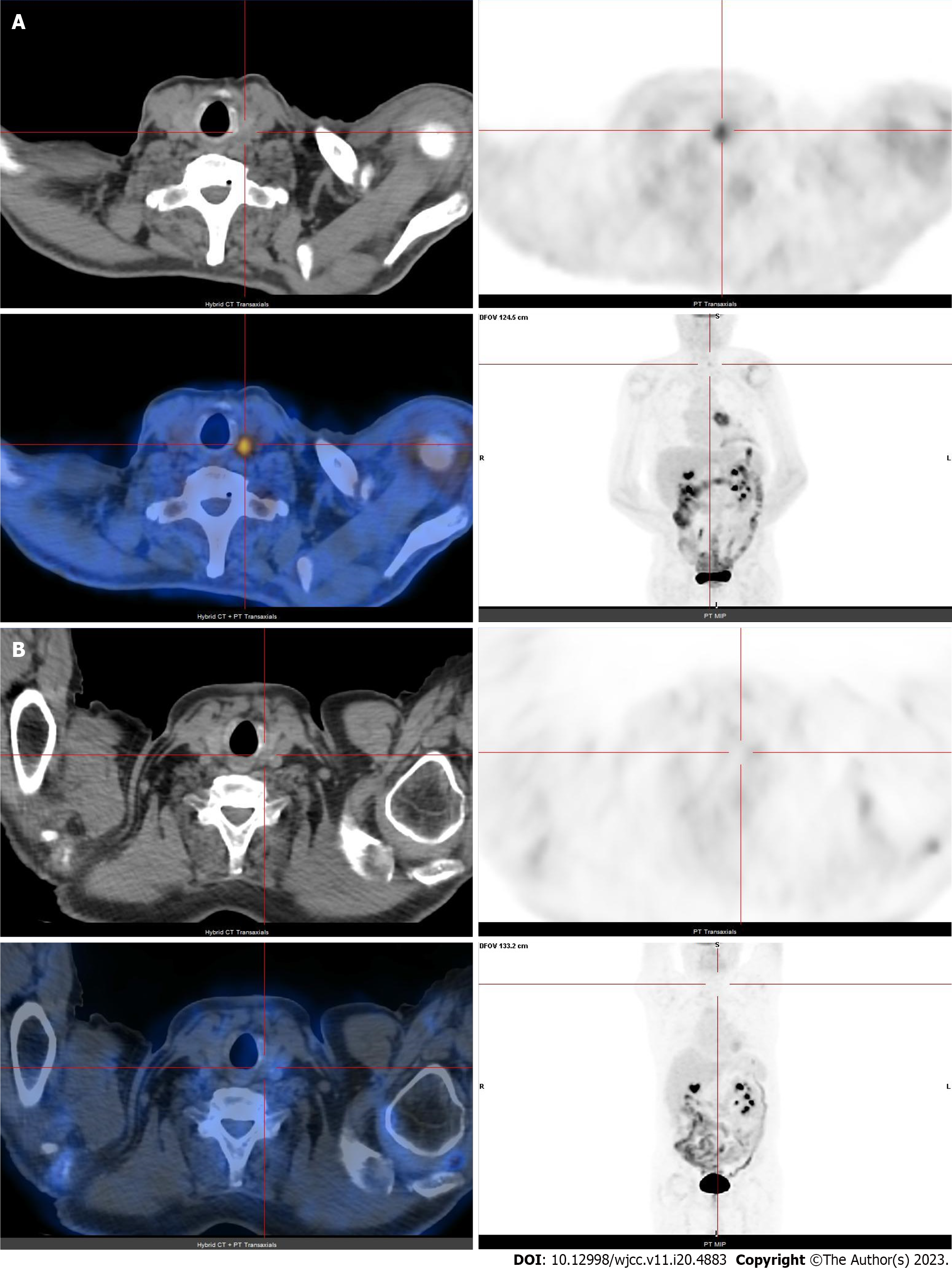
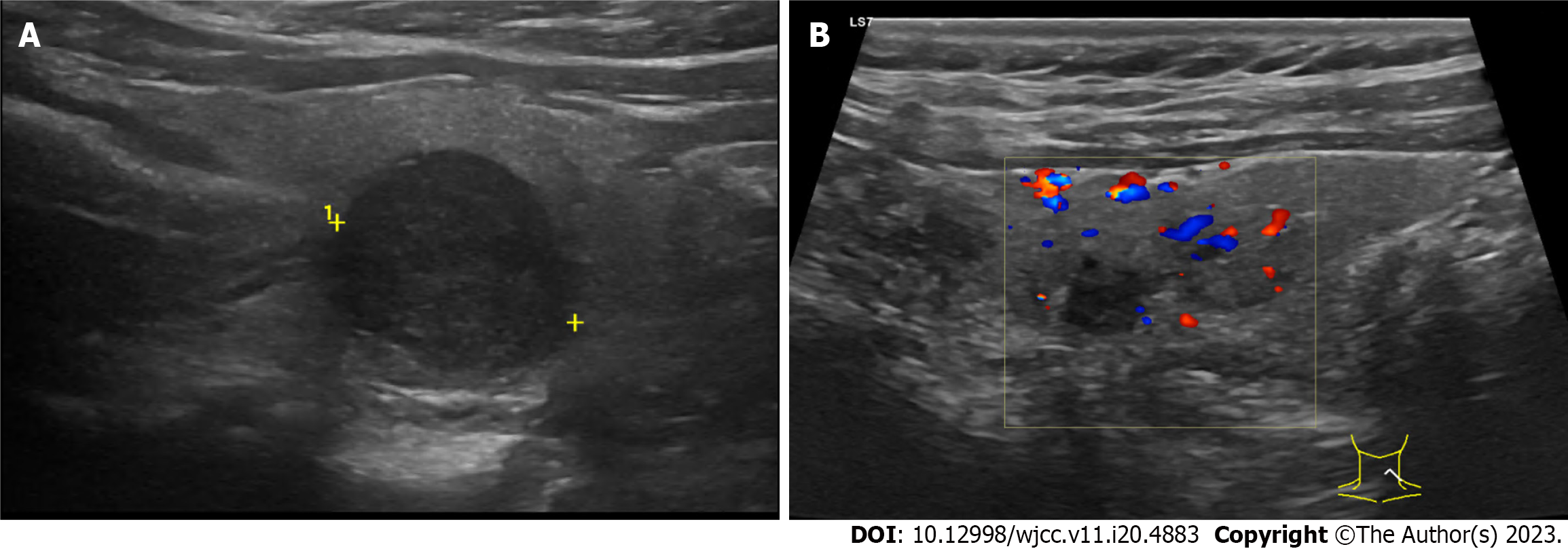
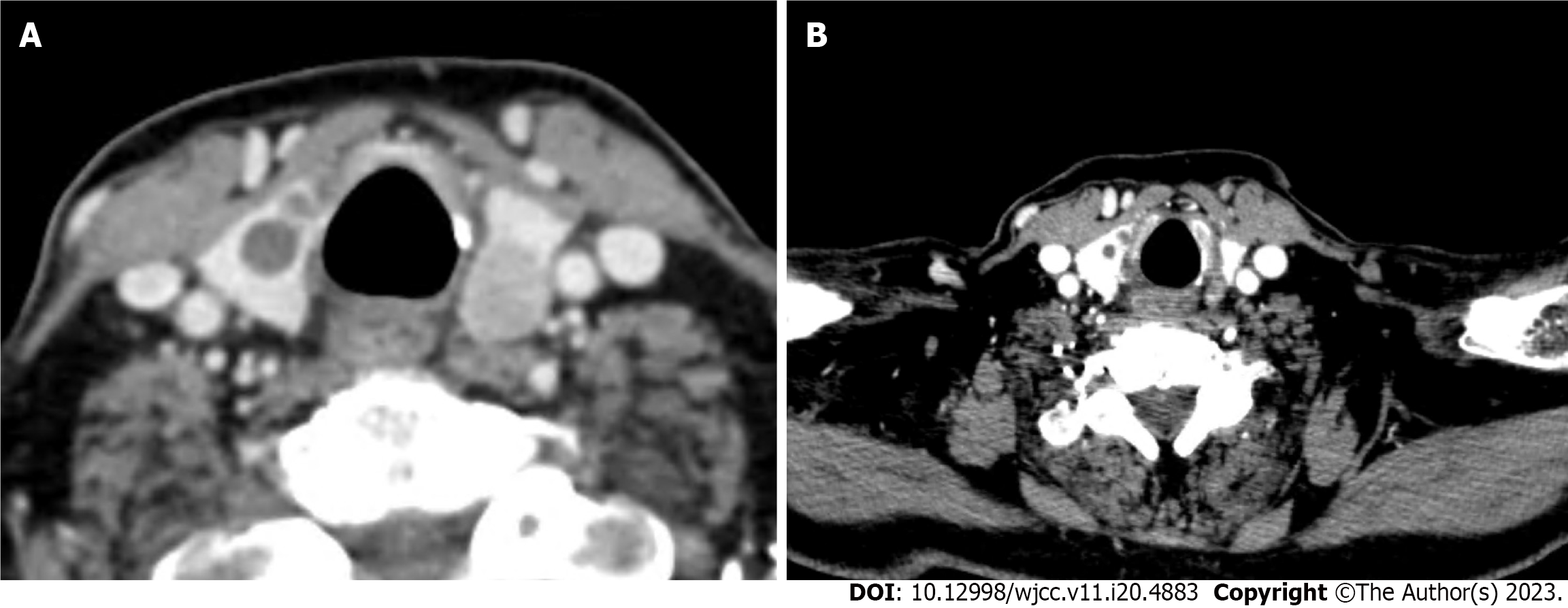
PET/CT-FDG scan showed focal and intense uptake of 18F-FDG in the left lobe of the thyroid gland (Figure 1A). Ultrasonography revealed a hypoechogenic mass, with a diameter of 1.7 cm, on the left lobe of the thyroid (Figure 2A). Nodule biopsy was performed under ultrasound control and the cytological study revealed a papillary carcinoma. Neck CT showed a contrast-enhancing nodule in the left lobe of the thyroid and absence of locoregional lymph node metastasis (Figure 3A).
Thyroid papillary carcinoma.
Given the context of palliative treatment for lung cancer, the patient had no indication for thyroid surgery, so he was proposed for microwave thermal ablation of the thyroid tumor.
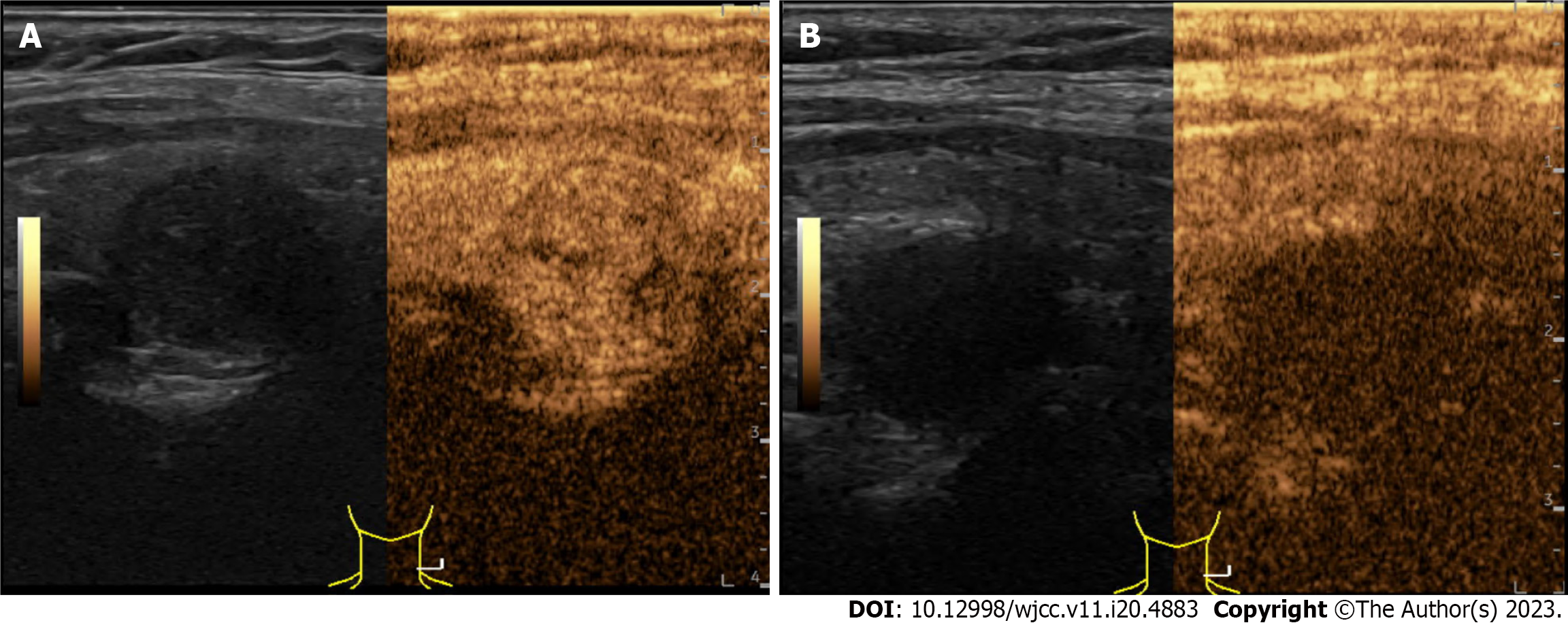
Before microwave ablation (MWA), contrast-enhanced ultrasound (CEUS) was performed to evaluate the extent of the tumor and its enhancement mode (Figure 4A). The relationship between the tumor and cervical critical structures was carefully evaluated to determine the best puncture site.
Topical 2% lidocaine was applied for local anesthesia and hydro dissection technique, which was employed at the designated ablation site before insertion of the ablation antenna.
It was then inserted a TATO 18-gauge microwave antenna. The output microwave power was 15 W for the ablation (Figure 5A).
We started from the most posterior part of the lower pole of the nodule, ablating to include the limit of the nodule and 2 mm of the surrounding thyroid tissue and the antenna was repositioned several times, successively in a more anterior and cranial direction of the lesion, always taking care to ensure that all tissue in the nodule and 2 mm around it were ablated. Iatrogenic injury to neighboring structures was avoided, using hydrodissection with lidocaine diluted in saline. This way, a safety margin of at least 2 mm was obviously guaranteed in relation to vital structures, such as the carotid artery.
The ablation time was 20 min.
After MWA, CEUS was performed to confirm whether the ablation was complete (Figure 4B).
Vocal cord function was evaluated during and after the procedure.
After ablation, the patient remained under observation for 1 h, with an ice patch at the puncture site.
At the end of this period, an ultrasound was performed to exclude acute complications of the procedure and the patient was discharged home.
Thermoablation of the malignant thyroid nodule was performed with technical success, meaning complete nodule ablation with safety margins.
The procedure was well tolerated by the patient and there were no acute complications.
The follow-up has been carried out with clinical and imaging surveillance, with thyroid ultrasound and CT to look for local or distant disease progression.
Ultrasound showed an avascularized hypoechoic area in the topography of the previous nodule, reflecting the ablation area (Figure 2B).
A CT scan 5 and 12 mo after MWA thermal ablation shows tumor disappearance and absence of locoregional or distant disease progression (Figure 3B).
A PET/CT-FDG scan 6 mo after thermal ablation had no evidence of hypermetabolic tumor lesions (Figure 1B).
Thermal ablations proved to be an effective and safe treatment option in small low-risk PTCs supported by recent long-term follow-up data[1-6]. However, there are no relevant data about treatment of thyroid papillary carcinomas with more than 1 centimeter and comparisons between MWA and surgical resection in the management of these tumors are rare[7-10].
This case illustrates a successful treatment of a thyroid papillary carcinoma with 17 mm, with a follow up of one year without recurrence.
No vital cervical structures were injured, namely vessels, nerves or vocal cords, and the patient's voice was unaffected. The remaining thyroid parenchyma remained intact, with normal thyroid function.
It is not possible to present an anatomopathological result that confirms the absence of remaining tumor tissue, since the patient did not undergo surgery and did not die (post mortem examination). However, none of the imaging tests he performed, such as CEUS, neck CT and PE-CT, found aspects that would raise this suspicion, quite the opposite, they demonstrated the disappearance of the nodule and of the area of hypermetabolism where it was previously present.
Literature on percutaneous treatment of thyroid carcinomas is limited. This case illustrates an effective treatment of a thyroid papillary carcinoma with microwave thermal ablation, with no major complications or signs of recurrence after one year of follow-up. MWA was comparable in the short term to surgery in terms of treatment safety and efficacy, that is, in this one-year follow-up period, no major iatrogenic complications of the procedure were identified and there were no signs of tumor recurrence. The patient was spared the morbidity of an open surgical procedure potentially higher, due to the fact that he was an immunosuppressed patient, because he was undergoing chemotherapy. Moreover, he did not have to be hospitalized and did not need hormone replacement therapy. At the time of diagnosis of thyroid carcinoma, the patient had no indication for thyroidectomy and, in the impossibility of percutaneous treatment, the thyroid nodule would only be under surveillance. However, at this moment, there are no signs of regional or distant recurrence of the lung neoplasm, so the attempt at a curative treatment for thyroid carcinoma proved to be an asset.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liu J, China; Jin S, China S-Editor: Ma YJ L-Editor: A P-Editor: Zhao S
| 1. | Cao XJ, Liu J, Zhu YL, Qi L, Liu G, Wang HL, Wang ZH, Zhou Y, He JF, Guo JQ, Shi LL, Jian M, Shataer A, Yan GZ, Zhao ZL, Wei Y, Peng LL, Li Y, Che Y, Wang SR, Yu MA. Efficacy and Safety of Thermal Ablation for Solitary T1bN0M0 Papillary Thyroid Carcinoma: A Multicenter Study. J Clin Endocrinol Metab. 2021;106:e573-e581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Cao XJ, Zhao ZL, Wei Y, Peng LL, Li Y, Wu J, Yu MA. Microwave ablation for papillary thyroid cancer located in the thyroid isthmus: a preliminary study. Int J Hyperthermia. 2021;38:114-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, Vitti P; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. J Endocrinol Invest. 2010;33:51-56. [PubMed] |
| 4. | Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10769] [Cited by in RCA: 9571] [Article Influence: 1063.4] [Reference Citation Analysis (1)] |
| 5. | Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, Chung SR, Ha EJ, Hahn SY, Jung SL, Kim DS, Kim SJ, Kim YK, Lee CY, Lee JH, Lee KH, Lee YH, Park JS, Park H, Shin JH, Suh CH, Sung JY, Sim JS, Youn I, Choi M, Na DG; Guideline Committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. 2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018;19:632-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 437] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 6. | Mauri G, Hegedüs L, Bandula S, Cazzato RL, Czarniecka A, Dudeck O, Fugazzola L, Netea-Maier R, Russ G, Wallin G, Papini E. European Thyroid Association and Cardiovascular and Interventional Radiological Society of Europe 2021 Clinical Practice Guideline for the Use of Minimally Invasive Treatments in Malignant Thyroid Lesions. Eur Thyroid J. 2021;10:185-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 154] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 7. | Wei Y, Niu WQ, Zhao ZL, Wu J, Peng LL, Li Y, Yu MA. Microwave Ablation versus Surgical Resection for Solitary T1N0M0 Papillary Thyroid Carcinoma. Radiology. 2022;304:704-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 50] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 8. | Wu J, Wei Y, Zhao ZL, Peng LL, Li Y, Lu NC, Yu MA. A preliminary study of microwave ablation for solitary T1N0M0 papillary thyroid carcinoma with capsular invasion. Int J Hyperthermia. 2022;39:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 9. | Wu J, Zhao ZL, Cao XJ, Wei Y, Peng LL, Li Y, Yu MA. A feasibility study of microwave ablation for papillary thyroid cancer close to the thyroid capsule. Int J Hyperthermia. 2021;38:1217-1224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Zheng L, Dou JP, Liu FY, Yu J, Cheng ZG, Yu XL, Wang H, Liu C, Yu MA, Cong ZB, Wang SR, Che Y, Xu ZF, Hao Y, Bai N, Wang X, Liu Y, Zhou Y, Shi J, Fu ZH, Zhan HY, Han ZY, Liang P. Microwave ablation vs. surgery for papillary thyroid carcinoma with minimal sonographic extrathyroid extension: a multicentre prospective study. Eur Radiol. 2023;33:233-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |