Published online Jul 16, 2023. doi: 10.12998/wjcc.v11.i20.4874
Peer-review started: May 25, 2023
First decision: June 13, 2023
Revised: June 16, 2023
Accepted: June 26, 2023
Article in press: June 26, 2023
Published online: July 16, 2023
Processing time: 48 Days and 5.5 Hours
Numerous variables are linked to the success of vaginal delivery, including the subpubic arch angle (SPAA) during labor, the importance of which has not yet been fully elucidated.
To examine the SPAA distributional characteristics and to ascertain SPAA’s ability to predict the type and duration of labor.
We determined the SPAA and analyzed the corresponding data. We also evaluated the relationship between the SPAA and the mode of delivery and the duration of labor by regression. The present study comprised a total of 301 pregnant women who had given birth at Beijing Tiantan Hospital of the Capital Medical University between January and December of 2021.
Our analysis of 301 pregnant women revealed that the SPAA measured using three-dimensional trans-perineal ultrasound had a minimum angle of 81° and a maximum angle of 122.2°. The angle in the normal vaginal delivery group was greater than that in the labor cesarean group (P = 0.000). The SPAA was a highly significant positive predictor of normal vaginal delivery (P = 0.000) with an area under the curve of 0.782 (P = 0.000; 95%CI: 0.717–0.848). We found the length of the second stage of labor to be positively influenced by the SPAA using linear regression analysis (P = 0.045).
The SPAA was a highly significant positive predictor of normal vaginal delivery. The length of the second stage of labor and normal vaginal birth were predicted by SPAA.
Core Tip: We adopted three-dimensional trans-perineal ultrasound to examine the subpubic arch angle (SPAA) distributional characteristics, and to ascertain the SPAA’s ability to predict the length of the second stage of labor and normal vaginal birth. We herein provided a noninvasive, low-cost tool to reduce the number of emergency cesarean deliveries conducted during labor.
- Citation: Liang ZW, Gao WL. Predictive value of the trans-perineal three-dimensional ultrasound measurement of the pubic arch angle for vaginal delivery. World J Clin Cases 2023; 11(20): 4874-4882
- URL: https://www.wjgnet.com/2307-8960/full/v11/i20/4874.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i20.4874
One of the key concerns of obstetricians and laboring mothers is predicting the results of labor. The discomfort experienced by pregnant women unable to give birth vaginally can be lessened by attenuating the effects of obstetricians’ differing degrees of experience with labor outcomes. Additionally, elective cesarean deliveries can be performed to end a pregnancy before labor begins, effectively lowering the rate of emergency cesarean deliveries.
Numerous variables-including a mother’s age, height, body mass index (BMI), weight gain during pregnancy, newborn weight, and pelvic size-are linked to a vaginal delivery's success. Due to its ambiguity, pelvic measurement is currently relegated to a lesser position in several obstetric textbooks[1]. Some argue that pelvic measurement should be abandoned entirely. However, some obstetricians have found that specific pelvic measurement indicators—including the subpubic arch angle (SPAA) are crucial to labor outcomes. A few studies have confirmed this observation[2-4]. An essential but underutilized signal in pelvic measurements is the SPAA, which serves as a gauge of the pelvic outlet’s anterior triangle’s size. Women with small SPAAs frequently have protracted or stalled labor that often requires forceps, fetal head extraction, or emergency cesarean section, which significantly increases the risk to both the mother and fetus.
Previous clinical and empirical studies have not fully elucidated the SPAA's importance in labor, possibly due to traditional measurement methods[5]. For example, obstetricians often use a protractor for manual measurement. Recently, new methods-including X-rays, subpubic arch angle (SPAA), magnetic resonance imaging (MRI), and ultrasonography-have been applied to measuring the SPAA. Ultrasonography's advantages in pelvic measurement are becoming increasingly evident. Ultrasound measurement of the SPAA before delivery has a relatively low technical requirement, but can accurately and objectively reflect the pelvic outlet without individual bias. While X-rays avoid fetal head obstruction and CT offers higher accuracy, both use radiation, which is unacceptable to most patients. MRI is radiation-free and accurate, but more expensive and less accessible.
Thus, this study aimed to explore three-dimensional (3D) ultrasound measurement of the SPAA as a noninvasive, low-risk, highly accurate method to predict the delivery mode before labor and investigate the relationship between the SPAA, vaginal delivery, and labor duration.
For this study we selected 301 mothers, all of whom delivered at the Obstetrics Department of Beijing Tiantan Hospital, Capital Medical University, during the period January–December of 2021. The maternal enrollment criteria were gestational week > 36 wk, singleton pregnancy, and primigravida. All pregnant women participating in this study signed an informed consent form approved by our hospital Ethics Committee.
The SPAA of the enrolled pregnant women was measured at 36-38 wk of gestation and three measurements were completed, each with an interval of one week. The mean of the three measurements was then used as the final SPAA. We also conducted an evaluation of the delivery mode at 36-38 wk of gestation. If the woman was deemed suitable for vaginal delivery, a routine ultrasound was performed and the SPAA was measured. No specific interventions were performed either during or after delivery regarding the mode of delivery. Following delivery, patients were categorized into four groups based on their respective modes of delivery. The antepartum cesarean section group referred to women who underwent surgical termination of their pregnancies prior to entering labor; the labor cesarean section group referred to those who could not continue vaginal delivery during labor and underwent emergency cesarean section; and the remaining women were in the vaginal delivery group that was subdivided into a normal vaginal delivery group (i.e., pregnant women who underwent natural delivery without forceps assistance), and a forceps group (i.e. pregnant women who experienced forceps delivery during labor). In cases where a pregnant woman experiences a significant complication during the second stage of labor necessitating urgent delivery of the fetus, forceps are typically employed to assist with delivery. Unfortunately, our hospital does not currently possess any fetal head extraction devices.
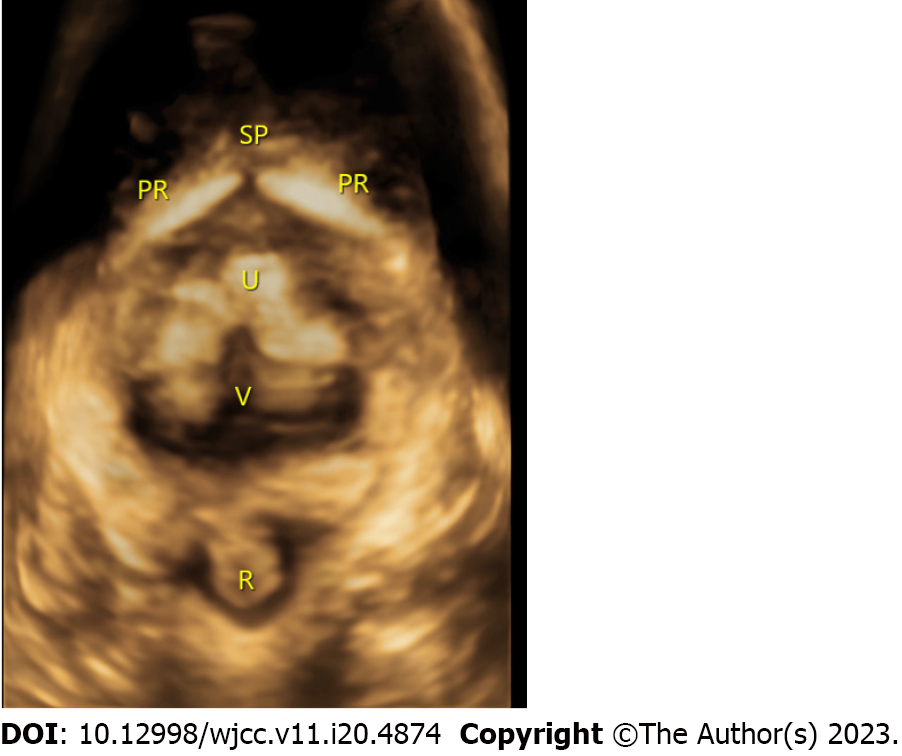
The measurement of the SPAA was performed by an established ultrasonographer using a General Electric Company Voluson E10 system with a 3–5-MHz transabdominal convex probe. The measurements were conducted by adopting the method used in the study by Choi et al[6]. This measurement was performed with the pregnant woman emptying her bladder, in a supine position, and with her legs straight up and as relaxed as possible. A glove was placed on the surface of the probe and the gel was applied and placed laterally on the vulva of the pregnant woman. The labia were gently separated to obtain a sagittal view of the pelvic floor. At this point, the pubic symphysis and urethra were located in front of the view, and the anus was located posteriorly. The midpoint of the inferior border of the pubic symphysis was then taken as a reference point and the axial plane was rotated until the median sagittal plane appeared. At this point, the full length of the descending pubic symphysis could be observed, and its angle was then measured. The 3D ultrasound measurements of one of the patients participating in the study are shown in Figure 1.
Data were collected in two categories for all pregnant women. The first category was general maternal information that included maternal age, height, gestational week at delivery, BMI and weight gain (pre-delivery weight minus first pregnancy check-up weight), and neonatal weight. The second category encompassed data on birth-related outcomes such as the length of the first stage of labor and the length of the second stage of labor in the normal vaginal delivery group and in the forceps group.
The data were statistically processed using SPSS 26. Our statistical methods entailed the distribution of the SPAA for all the mothers, which was expressed as a histogram with the SPAA distributions for the above four groups expressed as a box plot. The test of variability between the data from each group was calculated using the between-subjects effects test, and for the test of differences between the two groups we applied multiple comparisons in an LSD post hoc test. Logistic regression analysis was exploited to examine the predictive effects of the SPAA and other variables (height, body mass index, weight gain, and neonatal weight) on vaginal delivery, and the area under the curve (AUC) for the SPAA was used to evaluate the discriminatory ability of the predictive model; the Hosmer–Lemeshow goodness-of-fit test was then executed to evaluate the calibration of the model. A linear regression method was applied to analyze the relationship between the SPAA with respect to the length of the first stage of labor in women with spontaneous delivery (the normal vaginal delivery and forceps groups) and its relationship with the length of the second stage of labor in the normal vaginal delivery group. P < 0.05 was considered to constitute a statistically significant difference.
A total of 301 pregnant women were assigned to this study, and the overall and descriptive statistics (mean ± SD) of the measured variables in each group are shown in Table 1. The antepartum cesarean section group included 82 cases. Antepartum cesarean delivery is recommended in cases of fetal distress diagnosed by amniotic fluid III or fetal heart abnormalities, failed induction of labor, and macrosomia. The labor cesarean section group had 49 cases. The normal vaginal delivery group included 155 cases. The forceps group had 15 cases. We observed significant differences in pubic arch angle (P = 0.000), body mass index (P = 0.001), and newborn weight (P = 0.000) among the four groups of pregnant women, but not in any other data. Weight was higher in the surgical section group than in the vaginal delivery group, and neonatal weight was higher in the labor cesarean section and forceps groups than in the vaginal delivery and antepartum cesarean section groups.
| Characteristic | Sample | Mode of delivery | P value | ||||
| M | Range | Pre-labor CS (n = 82) | Normal vaginal delivery (n = 155) | Forceps delivery (n = 15) | CS in labor (n = 49) | ||
| SPAA (°) | 99.37 | 81-122.2 | 101.77 ± 6.12 | 99.29 ± 6.48 | 99.18 ± 5.28 | 95.62 ± 5.42 | 0.000 |
| 1st stage of labor (h) | - | - | - | 5.93 ± 3.53 | 6.23 ± 3.37 | - | - |
| 2nd stage of labor (h) | - | - | - | 0.48 ± 0.31 | 0.52 ± 0.40 | - | - |
| Age (yr) | 30.22 | 21-41 | 30.67 ± 3.06 | 29.76 ± 2.97 | 30.33 ± 2.87 | 30.88 ± 3.38 | 0.059 |
| Height (meters) | 1.63 | 1.50-1.78 | 1.63 ± 0.04 | 1.64 ± 0.05 | 1.62 ± 0.04 | 1.62 ± 0.05 | 0.091 |
| Gestational age at delivery (wk) | 39.40 | 36-41 | 39.35 ± 1.10 | 39.31 ± 0.97 | 39.73 ± 1.16 | 39.67 ± 0.97 | 0.173 |
| BMI (kg/m2) | 27.14 | 19-38 | 27.91 ± 3.45 | 26.51 ± 2.76 | 26.61 ± 2.57 | 27.99 ± 2.56 | 0.001 |
| Weight gain (kg) | 14.05 ± 6.21 | 9-52 | 14.37 ± 5.21 | 13.10 ± 4.12 | 12.60 ± 3.07 | 14.43 ± 4.59 | 0.084 |
| Birth weight (g) | 3426.13 | 2500-4500 | 3496.95 ± 394.84 | 3336.86 ± 344.73 | 3522.67 ± 336.99 | 3560.41 ± 410.54 | 0.000 |
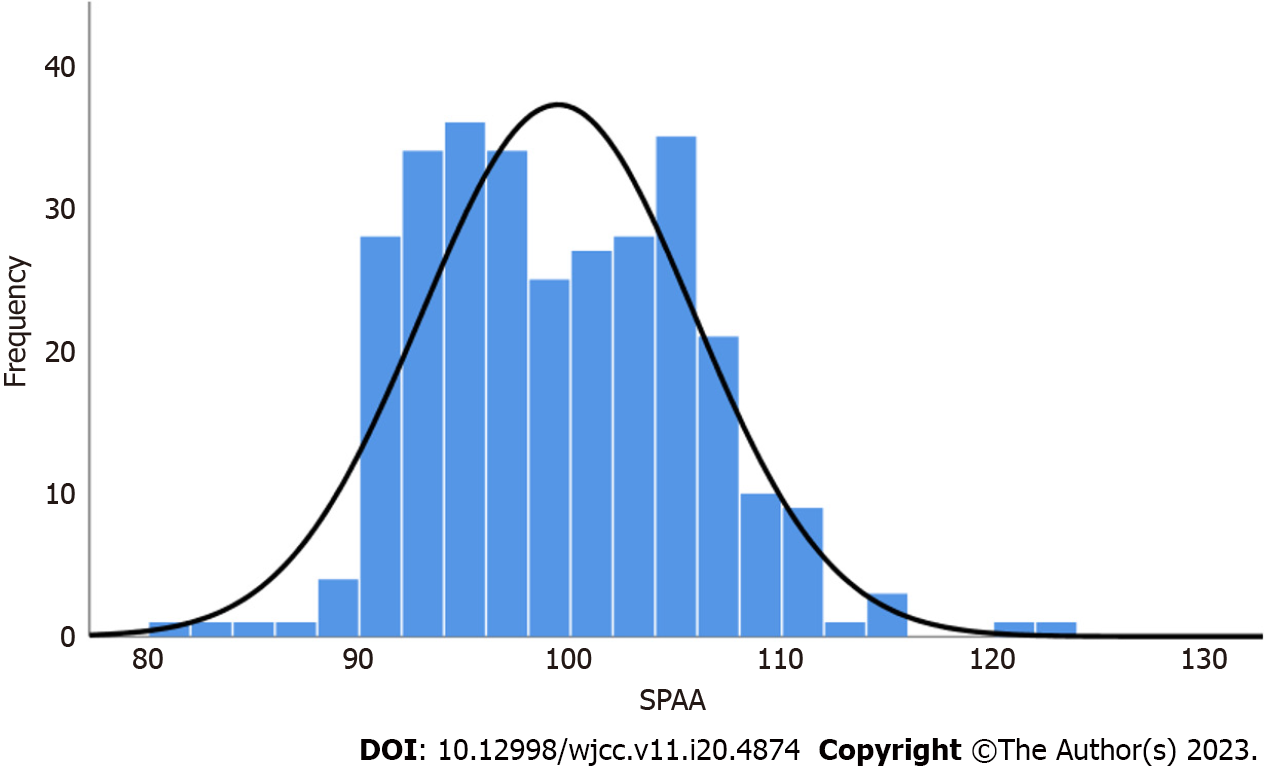
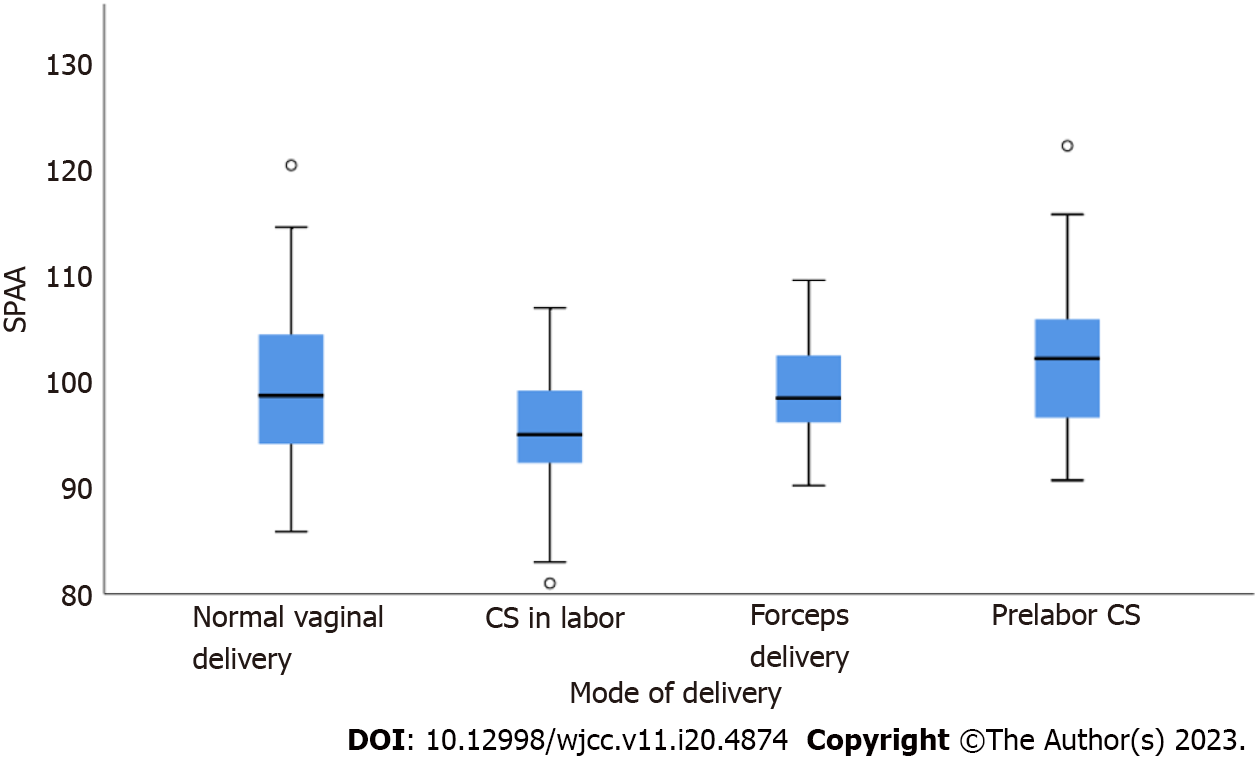
The distribution of the SPAA for all pregnant women and in each group are depicted in Figures 2 and 3. The data show a basically normal distribution, with a minimum angle of 81° and a maximum of 122.2°. The differences in the SPAAs among the four groups were tested for differences and we noted statistically significant differences (P = 0.000). To analyze the differences in the SPAAs among the four groups in detail, a two-by-two comparison was performed, and we ascertained that the angle in the normal vaginal delivery group was larger than that in the labor cesarean group (P = 0.000) and that the angle in the labor cesarean group was smaller than that in the forceps group (P = 0.052). In addition, the SPAA in the normal vaginal delivery group was smaller than that in the antepartum cesarean delivery group (P = 0.004). The remaining potential differences between the normal vaginal aspect group and the forceps group, and between the forceps group and the antepartum cesarean group were not statistically significant (P = 0.944 and 0.135).
To analyze the effect of the SPAA on the ability to deliver vaginally, we excluded the antepartum cesarean delivery group and conducted logistic regression analysis using data from 219 cases in the normal vaginal delivery group, forceps group, and labor cesarean delivery group. Each control variable at the maternal and neonatal levels was also included in the regression equation.
Our results revealed that the SPAA significantly and positively predicted normal vaginal delivery (P = 0.000). Age, height, and neonatal weight also positively predicted vaginal delivery (P = 0.000, 0.026, and 0.042) (Table 2).
| Predictors | Odds ratio (95%CI) | P value |
| Age (yr) | 1.13 (1.00–1.27) | 0.042 |
| Height (meters) | 0.00 (0.00–0.41) | 0.026 |
| Gestational age at delivery (wk) | 1.27 (0.87–1.84) | 0.214 |
| BMI (kg/m2) | 1.11 (0.97–1.26) | 0.130 |
| Weight gain (kg) | 1.05 (0.97–1.14) | 0.256 |
| Birth weight (g) | 1.00 (1.001–1.003) | 0.000 |
| SPAA (°) | 0.90 (0.84–0.95) | 0.000 |
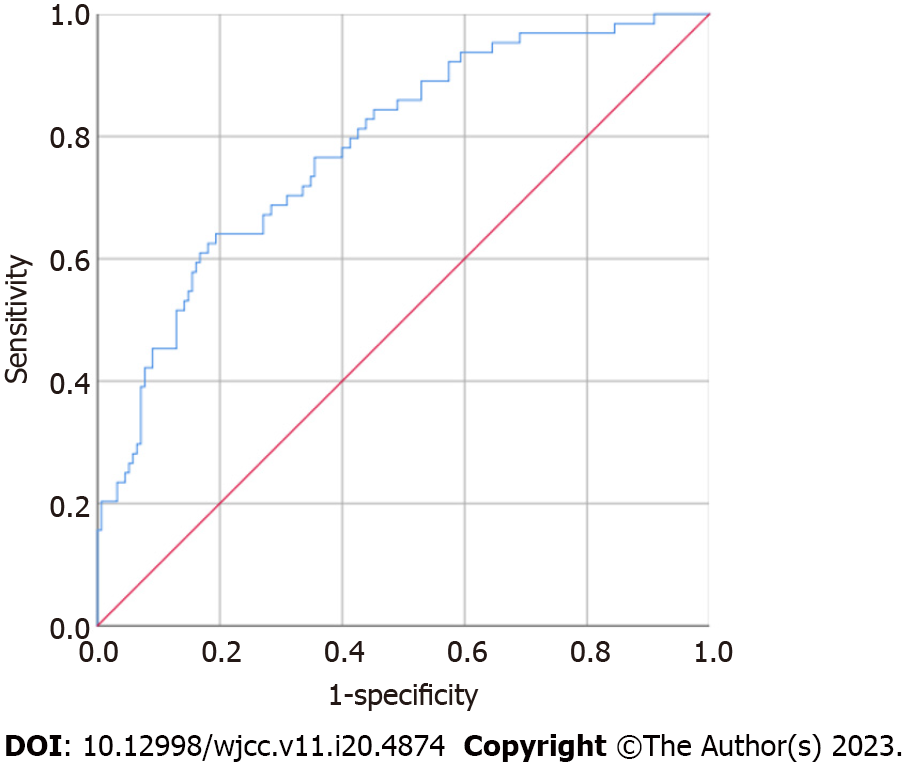
The model’s predictive-power test showed an AUC for the SPAA of 0.782 > 0.75 (P = 0.000; 95%CI: 0.717–0.848) (Figure 4), indicating that the model possessed good discriminatory ability. The Hosmer–Lemeshow goodness-of-fit test showed a Hosmer–Lemeshow χ2 = 6.19, P = 0.63 > 0.05, suggesting that the prediction model reflected favorable calibration ability.
To evaluate the relationship between the SPAA and length of labor, we analyzed its relationship with the first stage of labor and the length of the second stage of labor in women who experienced spontaneous delivery (including our normal vaginal delivery and forceps groups, for a total of 170 pregnant women). Each control variable at the maternal and neonatal levels was also included in the regression equation.
When the first stage of labor was the outcome variable, linear regression revealed that only weight gain positively predicted the duration of the first stage of vaginal delivery (P = 0.025) (Table 3 for details).
| Predictors | B (95%CI) | P value |
| Age (yr) | -0.02 (-0.21 to 0.16) | 0.789 |
| Height (meters) | -0.09 (-17.39 to 4.62) | 0.254 |
| Gestational age at delivery (wk) | 0.02 (-0.50 to 0.66) | 0.785 |
| BMI (kg/m2) | -0.03 (-0.25 to 0.18) | 0.758 |
| Weight gain (kg) | -0.19 (-0.31 to 0.02) | 0.025 |
| Birth weight (g) | 0.13 (0.000 to 0.003) | 0.135 |
| SPAA (°) | 0.06 (-0.05 to 0.12) | 0.459 |
Second, the second stage of labor was not an appropriate variable because it was artificially terminated in the forceps group. Therefore, only the relationship between the length of the second stage of labor (after log conversion) and the SPAA in the normal vaginal delivery group (155 pregnant women) was analyzed (Table 4). Linear regression showed that SPAA positively predicted the length of the second stage of labor (P = 0.045). Among other factors, age (P = 0.039) and height (P = 0.013) positively and negatively predicted the length of second stage of labor, respectively.
| Predictors | B (95%CI) | P value |
| Age (yr) | 0.17 (0.002 to 0.071) | 0.039 |
| Height (meters) | -0.18 (-4.63 to -0.55) | 0.013 |
| Gestational age at delivery (wk) | 0.02 (-0.10 to 0.13) | 0.853 |
| BMI (kg/m2) | -0.11 (-0.074 to 0.005) | 0.087 |
| Weight gain (kg) | 0.02 (-0.02 to 0.03) | 0.765 |
| Birth weight (g) | 0.09 (0.000 to 0.001) | 0.316 |
| SPAA (°) | 0.13 (-0.001 to 0.03) | 0.045 |
In this study we implemented 3D ultrasonographic measurements to analyze the differences in the SPAA among pregnant women experiencing different delivery methods. Our detailed analysis is provided below.
The subjects in the present study were pregnant Chinese women, and their SPAA data reflected Asian characteristics. The mean SPAA in this population was 99.37°, with a minimum of 81° and a maximum of 122.2°; a vast majority of the measurements were between 90 and 110 degrees. This result was in general agreement with the findings of Choi et al[6] in 2013 who measured the SPAA in 27 Asian women in Hong Kong at 9–13 wk of gestation, and found a range of 95.5–127.6°; an angle smaller than that shown for European and American populations. A similar study by Albrich et al[7] in 2015 entailed the use of 3D ultrasound to measure the SPAA in 611 mothers, and their values were much higher than in our study: their mean value was 109.3° (65.6–131.6°). This result may be related to the fact that 78.8% of these authors’ study population was Caucasian and reflected a taller stature.
In addition to population differences, we also determined that the instrument, mode, and timing of measurement exerted an effect on SPAA values. Handa et al[8] used MRI to measure the SPAA and compared the pelvic size of white American women with African American women, and found that their SPAAs were 83.7 ± 7.0° and 82.8 ± 6.7°, respectively. These values were much smaller than ones reported by Albrich et al[9] or relative to the data from this study using ultrasonographic measurements. The values obtained by different measurers in the same study were also inconsistent. For example, in the study by Albrich et al[9] in 2012, it was found that for the same sample the SPAA measured by one examiner was 99.71 ± 10.89° while another measured it at 101.4 ± 10.33°. In addition, the timing of measurements used in different studies varies, potentially leading to measurement errors. For example, in the current study we noted the mean of the three measurements of the SPAA before 38 wk, while previous investigators measured in early pregnancy and also 1-3 d after delivery. However, it was unclear from the current study whether childbirth caused changes in the SPAA. Considering that this index mainly serves to predict vaginal delivery, the measurement time should be appropriate prior to delivery. Ultimately, however, considering the cost of care, the ease of implementation of the measurement method, and patient acceptance, we recommend ultrasonographic measurement.
We herein analyzed the close association between SPAA and delivery mode from two aspects.
The SPAA in the normal vaginal delivery group was larger than that in the cesarean delivery group (P = 0.000), consistent with previous studies. For example, a study by Gilboa et al[10] in 2013 revealed that the SPAA in pregnant women with operative delivery was less than in women experiencing vaginal delivery (97.1 ± 11.5° vs 110.1 ± 14.0°, P < 0.005). These data are also more consistent with the clinical analysis since the SPAA must be larger in pregnant women who can deliver vaginally; otherwise, they could not deliver vaginally and would have to deliver by cesarean section.
Next, we ascertained that the SPAA was a predictor of successful vaginal delivery among pregnant women in spontaneous labor. Logistic regression analysis revealed that the SPAA was significantly associated with vaginal delivery. Moreover, the sensitivity of SPAA in this event was significant (AUC, 0.782; P = 0.000; 95%CI: 0.717–0.848), a finding consistent with a study by Perlman et al[11]. However, this result conflicted with data from the study by Albrich et al[7] in 2015, who failed to find an association between the SPAA and vaginal delivery. This apparent dichotomy may have been due to the differences in the pelvic characteristics between the authors’ sample and the present study: their study sample was predominantly Caucasian with a wider stature and pelvis, and their mean SPAA of 109.3° was greater than the 99.37° in our Asian population in the present study. This also implies that the SPAA is no longer a constraint for vaginal delivery in a wider pelvis.
In addition, this study revealed that maternal age, height, and neonatal weight-in addition to SPAA-predicted vaginal delivery (P = 0.000, 0.026, and 0.042). It is evident that the ability to deliver vaginally and the need for forceps, fetal suction, or even cesarean section to assist delivery are complex matters reflecting several factors that may exert influence. Of these, ultrasound measurement of the SPAA should gain the attention of obstetricians for further routine use because of its non-invasiveness, ease of performance, and favorable predictability.
We also found that the SPAA was inextricably linked to the length of labor. The analysis of the SPAA and the length of the second stage of labor in vaginal delivery herein revealed a significant difference in the SPAA (P = 0.045). This indicated that the duration of the second stage of labor was related to the SPAA, and the smaller the SPAA, the longer the second stage of labor; this finding was congruent with work by Albrich et al[7] in 2015, who found that the SPAA was associated with the second stage of labor in pregnant women with normal vaginal delivery (95%CI: 1.01–1.03; P = 0.003). Additionally, a study by Gilboa et al[10] in 2013 showed that for every 1° decrease in the SPAA, the odds ratio for surgical delivery was 0.933. Thus, it is evident that the SPAA is robustly related to the length of the second stage of labor. Our regression analysis also depicted age and height as correlated with the duration of the second stage of labor.
However, we did not uncover an association between the SPAA and length of the first stage of labor, as only maternal weight gain positively predicted the length of the first stage of labor (P = 0.025). This result may be due to the fact that the SPAA is the pelvic exit meridian, which, in the absence of other pelvic abnormalities, only affects the length of the second stage of labor and not the first stage.
The present study included only 301 pregnant women, and we will therefore in our follow-up study further increase sample size to achieve a more accurate assessment of the SPAA and its relationship to the mode of delivery, in the hope of promoting the application of 3D ultrasound in pelvic measurement.
In conclusion, the SPAA as an important index in pelvic measurement that should be given greater clinical attention as it is closely related to the ability to deliver vaginally, and it can also predict the occurrence of cesarean delivery. 3D ultrasound should be promoted as an important tool to be used in measuring the SPAA as it is of relatively low cost and easy to perform. We posit that this tool can reduce the number of emergency cesarean deliveries conducted during labor.
Numerous variables are linked to the success of vaginal delivery, including the subpubic arch angle (SPAA) during labor, the importance of which has not yet been fully elucidated.
For this study, we adopted three-dimensional (3D) trans-perineal ultrasound to examine the SPAA distributional characteristics.
For this study, we adopted 3D trans-perineal ultrasound to examine the SPAA distributional characteristics and to ascertain SPAA’s ability to predict the type and duration of labor.
The present study comprised a total of 301 pregnant women who had given birth at Beijing Tiantan Hospital of the Capital Medical University between January and December of 2021.
Our analysis of 301 pregnant women revealed that the SPAA measured using 3D trans-perineal ultrasound had a minimum angle of 81° and a maximum angle of 122.2°. The angle in the normal vaginal delivery group was greater than that in the labor cesarean group (P = 0.000). The SPAA was a highly significant positive predictor of normal vaginal delivery (P = 0.000) with an area under the curve of 0.782 (P = 0.000; 95%CI: 0.717–0.848). We found the length of the second stage of labor to be positively influenced by the SPAA using linear regression analysis (P = 0.045).
The SPAA was a highly significant positive predictor of normal vaginal delivery. The length of the second stage of labor and normal vaginal birth were predicted by SPAA.
The SPAA as an important index in pelvic measurement that should be given greater clinical attention as it is closely related to the ability to deliver vaginally, and it can also predict the occurrence of cesarean delivery.
We would like to thank the Hai-Man Song of Department of Ultrasound, Beijing Tiantan Hospital, Capital Medical University.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hatipoglu S, Turkey; Martín Del Olmo JC, Spain S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Martelli F, Youssef A, Capogna MV, Bruno A, Bruno V, Dodaro MG, Ticconi C, Ghi T, Piccione E, Pietropolli A. Longitudinal Changes of Subpubic Arch Angle throughout Pregnancy. Gynecol Obstet Invest. 2020;85:100-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Yeomans ER. Clinical pelvimetry. Clin Obstet Gynecol. 2006;49:140-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Floberg J, Belfrage P, Ohlsén H. Influence of pelvic outlet capacity on labor. A prospective pelvimetry study of 1,429 unselected primiparas. Acta Obstet Gynecol Scand. 1987;66:121-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Maharaj D. Assessing cephalopelvic disproportion: back to the basics. Obstet Gynecol Surv. 2010;65:387-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Dietz HP, Lanzarone V, Simpson JM. Predicting operative delivery. Ultrasound Obstet Gynecol. 2006;27:409-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Choi S, Chan SS, Sahota DS, Leung TY. Measuring the angle of the subpubic arch using three-dimensional transperineal ultrasound scan: intraoperator repeatability and interoperator reproducibility. Am J Perinatol. 2013;30:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Albrich SB, Shek K, Krahn U, Dietz HP. Measurement of subpubic arch angle by three-dimensional transperineal ultrasound and impact on vaginal delivery. Ultrasound Obstet Gynecol. 2015;46:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Handa VL, Lockhart ME, Fielding JR, Bradley CS, Brubaker L, Cundiff GW, Ye W, Richter HE; Pelvic Floor Disorders Network. Racial differences in pelvic anatomy by magnetic resonance imaging. Obstet Gynecol. 2008;111:914-920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Albrich S, Laterza RM, Merinsky A, Skala C, Koelbl H, Naumann G. [Measurement of the infrapubic angle using 3D perineal ultrasound and its relationship to obstetrical parameters]. Ultraschall Med. 2012;33:E95-E100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Gilboa Y, Kivilevitch Z, Spira M, Kedem A, Katorza E, Moran O, Achiron R. Pubic arch angle in prolonged second stage of labor: clinical significance. Ultrasound Obstet Gynecol. 2013;41:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Perlman S, Schreiber H, Kivilevitch Z, Bardin R, Kassif E, Achiron R, Gilboa Y. Sonographic risk assessment for an unplanned operative delivery: a prospective study. Arch Gynecol Obstet. 2022;306:1469-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |