Published online Jan 16, 2023. doi: 10.12998/wjcc.v11.i2.401
Peer-review started: September 25, 2022
First decision: October 18, 2022
Revised: November 11, 2022
Accepted: December 19, 2022
Article in press: December 19, 2022
Published online: January 16, 2023
Processing time: 108 Days and 19.7 Hours
Giant inguinoscrotal hernias are huge inguinal hernias that extend below the midpoint of the inner thigh in the standing posture. Giant inguinoscrotal hernias are rare in developed countries because of their better medical resources and early treatment. However, they can develop in patients who refuse surgery or ignore their condition. Intervention is inevitable because strangulation and organ perforation can occur, leading to peritonitis and sepsis. Common surgical approaches include open abdominal and inguinal approaches or a combination of both.
We present the case of a 73-year-old man who visited our emergency department with a huge mass in his left scrotum and septic complications. Abdominal computed tomography revealed a large left inguinoscrotal hernia that contained small bowel loops and the colon. Emergency surgical intervention was performed immediately because intestinal strangulation was highly suspected. The operative repair was performed using a combination of mini-exploratory laparotomy and the inguinal approach. The incarcerated organs, which included the ileum and sigmoid colon, had relatively good intestinal perfusion without perforation or ischemic changes. They were successfully reduced into the abdomen, and bowel resection was not necessary. A tension-free prosthetic mesh was used for the hernia repair. Two weeks after the initial surgery, and with adequate antimicrobial therapy, the patient recovered and was discharged from our hospital. No evidence of hernia relapse was noted during the outpatient follow-up examination 3 mo after surgery.
Emergency surgery involving combined mini-exploratory laparotomy and the inguinal approach should be performed for serious incarcerated giant inguinoscrotal hernias.
Core Tip: Giant inguinoscrotal hernias are defined as hernias extending below the midpoint of the inner thigh of the patient in the standing position. Symptoms may vary, and serious complications, including intestinal obstruction and strangulation, may cause peritonitis and sepsis. Emergency surgery should be performed because of the risks of strangulation, perforation, and progressive necrosis. In this case, it was surprising to find the simultaneous existence of the ileum and sigmoid colon in the large inguinal hernia sac. The use of the inguinal approach combined with mini-exploratory laparotomy for giant hernial repair is beneficial and should be considered.
- Citation: Liu SH, Yen CH, Tseng HP, Hu JM, Chang CH, Pu TW. Repair of a giant inguinoscrotal hernia with herniation of the ileum and sigmoid colon: A case report. World J Clin Cases 2023; 11(2): 401-407
- URL: https://www.wjgnet.com/2307-8960/full/v11/i2/401.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i2.401
Giant inguinoscrotal hernias are defined as huge inguinal hernias that extend below the midpoint of the inner thigh in the standing posture[1]. Although rare, giant inguinoscrotal hernias still exist in developed countries. The main problem with inguinal hernias is their increasing size, which necessitates early surgical intervention. Giant inguinoscrotal hernias may develop in patients who refuse surgery or ignore their disease for a long time. Treatment of inguinoscrotal hernias is inevitable because strangulation and organ perforation can occur, resulting in further peritonitis and sepsis[2]. The World Society of Emergency Surgery (WSES) guidelines for emergency repair of complicated abdominal wall hernias suggest that patients should undergo emergency hernial repair immediately if intestinal strangulation is suspected[3]. Additionally, it has been proven that emergency surgical interventions are associated with higher rates of postoperative complications and adverse outcomes compared to early elective proce
A 73-year-old man visited the emergency department of our hospital because of a huge mass in his left scrotum and intolerable lower abdominal and groin pain for a duration of approximately 2 wk.
Approximately 20 mo prior, the patient was diagnosed with a huge left inguinoscrotal hernia at our outpatient department; however, he refused early surgical intervention. Several days before the patient presented to the emergency department, he also experienced general weakness and decreased urine output.
Other than the previous diagnosis of left inguinal hernia, the patient had no history of chronic diseases or surgeries.
The patient had been working as a security guard at an apartment for more than 10 years. Part of his job involved lifting and carrying packages received by the residents. No relevant family history was noted.
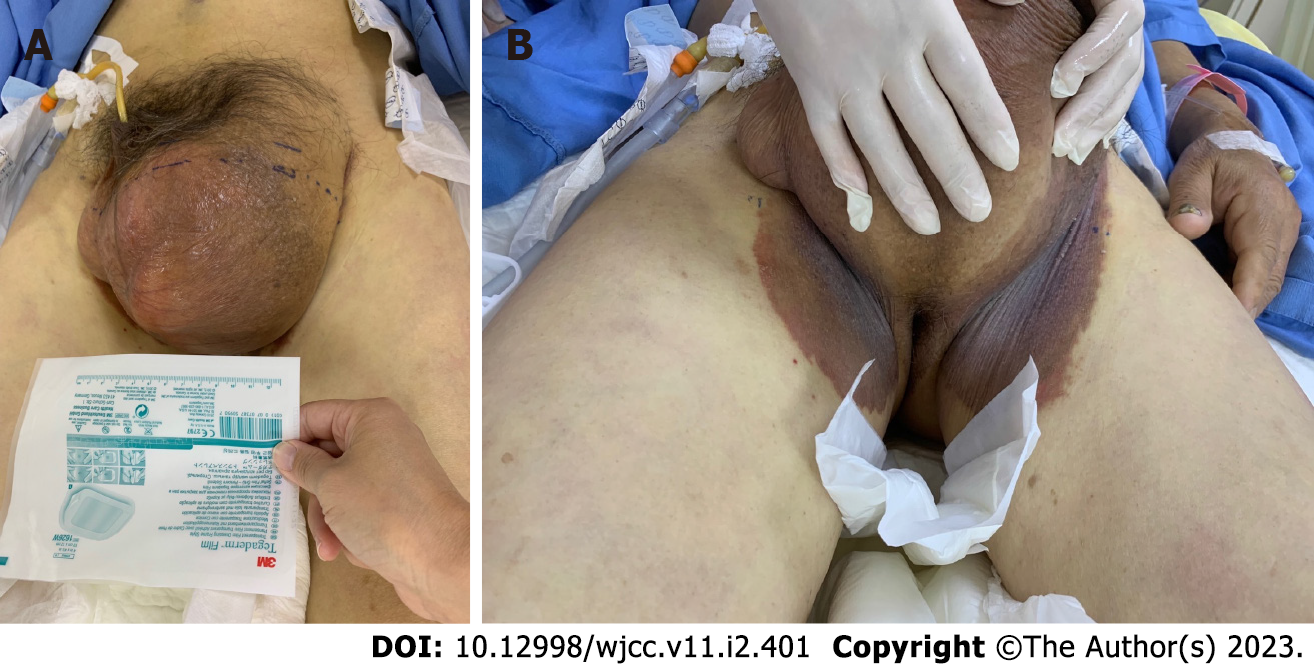
His vital signs were as follows: Body temperature, 36°C; blood pressure, 106/73 mmHg; heart rate, 95 beats/min, and respiratory rate, 22 breaths/min. The results of the physical examination revealed pitting edema of the bilateral lower limbs, tenderness in the left lower abdomen and inguinal region, a large irreducible inguinoscrotal hernia on the left side that measured approximately 14 cm x 16 cm in the supine position, and bilateral inguinal ecchymosis (Figure 1).
Laboratory serum examinations revealed a white blood cell count of 21.57 × 103/μL, 92.3% neutrophils, and thrombocytopenia with a platelet count of 90 × 103/μL. C-reactive protein and procalcitonin levels were 35.32 mg/dL and 24.96 ng/mL, respectively. The serum creatinine level was 2.3 mg/dL.
Abdominal computed tomography (CT) scanning was performed without contrast because of decreased renal function, suggesting a huge left inguinal hernia with herniation of the small intestine and colon as well as a small number of ascites (Figure 2).
Physical and laboratory serum test results and radiographic findings indicated the presence of a large incarcerated inguinal hernia with sepsis.
After diagnosing, we intravenously administered antibiotics comprising Flomoxef 1g every 12 h. Flomoxef was chosen because of its efficacy for intra-abdominal infections. The dosage was adjusted according to the patient’s creatinine clearance rate. Because of the risks of strangulation, perforation, and further profound septic shock, emergency surgery was performed.
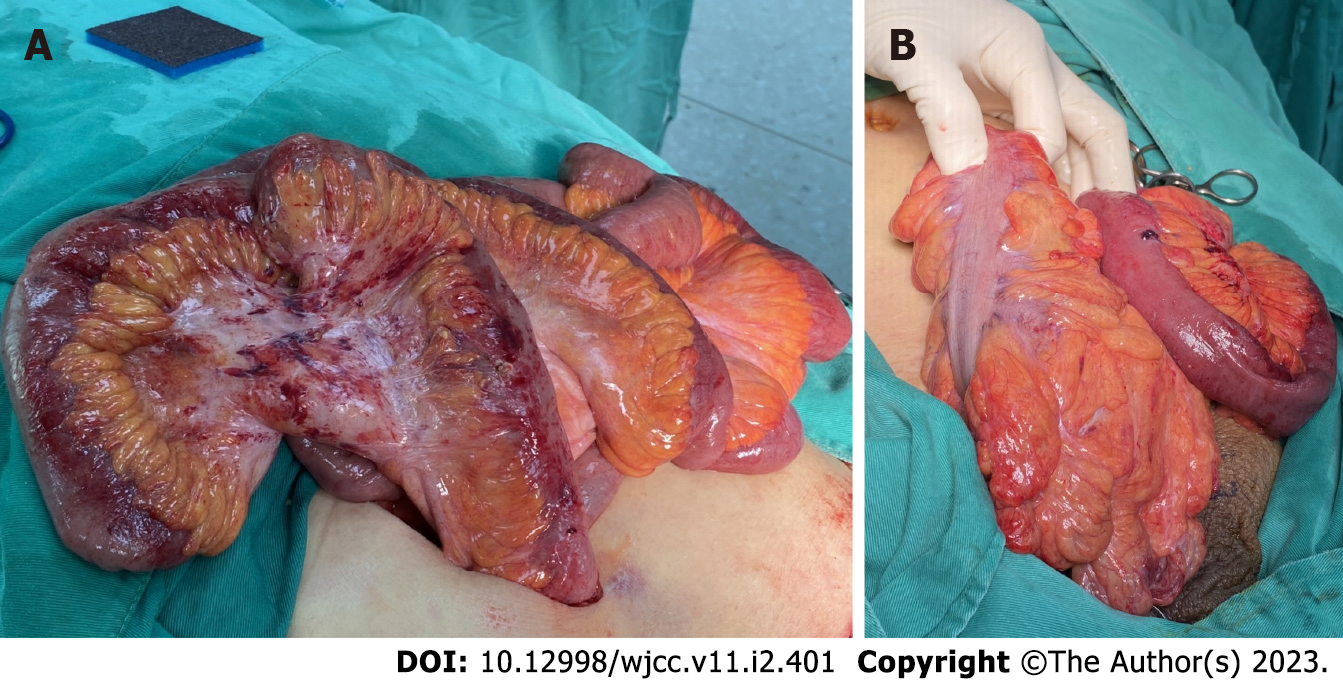
The patient was placed in the supine position under general anesthesia. An inguinal incision on the left side revealed that the hernial sac was filled with ileum and sigmoid colon. Because of the failure to reduce the contents into the abdominal cavity, even with enlargement of the internal ring, a mini-midline incision was made. The incarcerated organs were carefully pulled out, and the adhesion between the hernial contents was separated. The hernial contents were grossly inflamed, with mild swelling and an erythematous appearance (Figure 3A). The incarcerated organs, with relatively good intestinal perfusion and no perforation or ischemic changes following a thorough examination, were successfully reduced into the abdomen (Figure 3B). The hernial repair was performed using tension-free techniques with unabsorbable polypropylene mesh sutured on the posterior wall of the inguinal canal. Finally, a Jackson-Pratt drain was placed in the left inguinal canal. The patient was transferred to the intensive care unit after surgery to closely monitor the end-organ function.
The patient experienced no complications during the early postoperative period. Two weeks after the initial surgery, with adequate infection control, the patient recovered and was discharged. The patient was able to remain in the standing position without evidence of relapse of the hernia at the time of the outpatient follow-up examination 3 mo after surgery.
Giant inguinoscrotal hernias are rare in developed countries. However, they can occur as a complication of an inguinal hernia. Other complications of an inguinal hernia include hernial enlargement, increasing pain, and incarceration or strangulation. They often result from patient neglect and the rejection of the suggested surgery for a hernia. For our patient, the risk factors for inguinal hernia were identified as his age, sex, and occupation[5]. Giant inguinoscrotal hernias are more common in less developed countries that lack medical resources. The size of the hernia often negatively affects daily activities. The penis buried in the enlarged scrotum can result in urine dribbling over the scrotal skin, potentially leading to skin damage, ulceration, and further infections[6]. Giant inguinoscrotal hernias accompanied by acute kidney injury resulting from urinary tract obstruction have been reported[7,8]. In the present case, the CT scan did not reveal obstructive uropathy such as hydronephrosis. Hence, we suspected that renal impairment with the clinical presentation of decreased urine output in our case occurred as a result of sepsis. Hernial contents that cannot be reduced into the abdominal cavity are referred to as incarcerated hernias. Bowel obstruction and strangulation of the bowel contents with a compromised blood supply are serious results of incarceration. The common contents of the hernial sac are the small intestine and omentum. In some cases, the stomach, appendix, cecum, kidney, urinary bladder, ovaries, and sigmoid colon have been found in the hernial sac[9,10]. In the present case, the simultaneous existence of the ileum and sigmoid colon in a large inguinal hernia sac was observed.
In our patient with a giant inguinoscrotal hernia, sepsis occurred with impaired renal function and coagulation according to the Sequential Organ Failure Assessment score[11]. We performed surgery immediately because of the risk of strangulation and progressive necrosis, which could be fatal according to the WSES guidelines for emergency repair of complicated abdominal wall hernias[3].
A sudden increase in intra-abdominal pressure may occur after the majority of the hernial organs have been reduced into the abdominal cavity[12]. Abdominal compartment syndrome can develop, leading to respiratory compromise attributable to an increase in intrathoracic pressure[13]. To avoid compromising respiratory and cardiac functions and enable successful recovery, a complete preo
Several surgical interventions have been developed for this purpose, and they all share the common strategy of relocating the hernial organs into the abdominal cavity, adapting to a relative emptiness. Two approaches can be employed. First, the abdominal cavity can be increased by artificially inducing progressive pneumoperitoneum[14,15]or creating an anterior abdominal wall defect and performing mesh repair and flap techniques[16,17]. Second, reduction of abdominal or hernial contents can be performed to relocate the reduced abdominal organs[18].
In the present case, bowel resection was not necessary because the patient maintained an acceptable abdominal space without excessive tension and airway pressure perioperatively. Furthermore, his vital signs and urine output were closely monitored postoperatively because of the high risk of increased intra-abdominal pressure. Although measuring the intravesical pressure is a common method used to identify intra-abdominal pressure, we did not use this for our patient because of its relatively invasive nature despite the minimally invasive implementation requirements. Orchiectomy was not performed because dissection of the spermatic cord was not problematic. The scrotal skin was not resected because it was not infected. We successfully predicted that the skin would be able to recover after the removal of additional tension caused by the giant inguinoscrotal hernia.
We used an inguinal approach combined with a mini-midline incision. This method of management has several advantages. First, it results in an easier reduction of the ileum and sigmoid colon into the abdominal cavity through the defect. Second, it allowed us to carefully examine the bowel condition to determine the presence of perforation or ischemic changes. Finally, a Jackson-Pratt drain could be placed to ensure adequate drainage. Because hernial defects are large, the risk of recurrence of giant inguinoscrotal hernias is much higher than that of other inguinoscrotal hernias. The use of tension-free techniques whenever possible is recommended for hernial repairs[19]. Most importantly, in addition to the initial surgical intervention, appropriate antimicrobial therapy was fundamental for our patient with sepsis.
In modern surgical practice, giant inguinoscrotal hernias are uncommon. When they do occur, they present challenges for the attending surgeon because they can cause fatal complications. For patients presenting with sepsis, emergency surgery should be performed if there is significant incarceration or strangulation. Adequate preoperative planning as well as intraoperative and postoperative monitoring are essential for these patients. The use of a combination of mini-exploratory laparotomy and the inguinal approach is worthy of further investigation. Enlargement of the abdominal cavity or debulking of the abdominal organs should be avoided if the abdominal cavity is sufficient. Relocation of the incarcerated organs using proper and early antimicrobial therapy was the cornerstone of successful treatment for this case.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Sintusek P, Thailand; Sultan AAEA, Egypt; Tangsuwanaruk T, Thailand S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Hodgkinson DJ, McIlrath DC. Scrotal reconstruction for giant inguinal hernias. Surg Clin North Am. 1984;64:307-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Gaedcke J, Schüler P, Brinker J, Quintel M, Ghadimi M. Emergency repair of giant inguinoscrotal hernia in a septic patient. J Gastrointest Surg. 2013;17:837-839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Birindelli A, Sartelli M, Di Saverio S, Coccolini F, Ansaloni L, van Ramshorst GH, Campanelli G, Khokha V, Moore EE, Peitzman A, Velmahos G, Moore FA, Leppaniemi A, Burlew CC, Biffl WL, Koike K, Kluger Y, Fraga GP, Ordonez CA, Novello M, Agresta F, Sakakushev B, Gerych I, Wani I, Kelly MD, Gomes CA, Faro MP Jr, Tarasconi A, Demetrashvili Z, Lee JG, Vettoretto N, Guercioni G, Persiani R, Tranà C, Cui Y, Kok KYY, Ghnnam WM, Abbas AE, Sato N, Marwah S, Rangarajan M, Ben-Ishay O, Adesunkanmi ARK, Lohse HAS, Kenig J, Mandalà S, Coimbra R, Bhangu A, Suggett N, Biondi A, Portolani N, Baiocchi G, Kirkpatrick AW, Scibé R, Sugrue M, Chiara O, Catena F. 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg. 2017;12:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 114] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 4. | Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996;25:835-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 338] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 5. | HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1355] [Cited by in RCA: 1262] [Article Influence: 180.3] [Reference Citation Analysis (1)] |
| 6. | Serpell JW, Polglase AL, Anstee EJ. Giant inguinal hernia. Aust N Z J Surg. 1988;58:831-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Goonetilleke K, McIlroy B. Giant inguinoscrotal hernia presenting with acute renal failure: a case report and review of literature. Ann R Coll Surg Engl. 2010;92:W21-W23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Szymański MW, Hellmann AR, Patel A, Proczko-Stepaniak M, Kaska Ł. Acute Renal Failure Caused by Giant Inguinoscrotal Bladder Hernia. Urology. 2020;141:24-26. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Tahir M, Ahmed FU, Seenu V. Giant inguinoscrotal hernia: case report and management principles. Int J Surg. 2008;6:495-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Weitzenfeld MB, Brown BT, Morillo G, Block NL. Scrotal kidney and ureter: an unusual hernia. J Urol. 1980;123:437-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17092] [Article Influence: 1899.1] [Reference Citation Analysis (2)] |
| 12. | Parker SG, Halligan S, Blackburn S, Plumb AAO, Archer L, Mallett S, Windsor ACJ. What Exactly is Meant by "Loss of Domain" for Ventral Hernia? World J Surg. 2019;43:396-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Papavramidis TS, Marinis AD, Pliakos I, Kesisoglou I, Papavramidou N. Abdominal compartment syndrome - Intra-abdominal hypertension: Defining, diagnosing, and managing. J Emerg Trauma Shock. 2011;4:279-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Mcadory RS, Cobb WS, Carbonell AM. Progressive preoperative pneumoperitoneum for hernias with loss of domain. Am Surg. 2009;75:504-509. [PubMed] |
| 15. | Caldironi MW, Romano M, Bozza F, Pluchinotta AM, Pelizzo MR, Toniato A, Ranzato R. Progressive pneumoperitoneum in the management of giant incisional hernias: a study of 41 patients. Br J Surg. 1990;77:306-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | El-Dessouki NI. Preperitoneal mesh hernioplasty in giant inguinoscrotal hernias: a new technique with dual benefit in repair and abdominal rooming. Hernia. 2001;5:177-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Valliattu AJ, Kingsnorth AN. Single-stage repair of giant inguinoscrotal hernias using the abdominal wall component separation technique. Hernia. 2008;12:329-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Vasiliadis K, Knaebel HP, Djakovic N, Nyarangi-Dix J, Schmidt J, Büchler M. Challenging surgical management of a giant inguinoscrotal hernia: report of a case. Surg Today. 2010;40:684-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Amid PK. Groin hernia repair: open techniques. World J Surg. 2005;29:1046-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (1)] |