Published online Jan 16, 2023. doi: 10.12998/wjcc.v11.i2.394
Peer-review started: May 13, 2022
First decision: July 29, 2022
Revised: August 7, 2022
Accepted: October 24, 2022
Article in press: October 24, 2022
Published online: January 16, 2023
Processing time: 244 Days and 0.9 Hours
Aggressive giant cell tumor of the distal fibula is so rare that no consensus on a surgical strategy has been reached. Thus, an appropriate treatment strategy is still important to discuss.
A 61-year-old man who had been experiencing progressive swelling of the left lateral malleolus accompanied by pain for half a year was presented at our hospital. He had never been treated prior to coming to our hospital. Preoperative imaging revealed a 10 cm × 6 cm mass located in the body of the distal fibula. Pathological biopsies confirmed it was a giant cell tumor. Preoperative exami
Tibial talus fusion is an effective method for the treatment of distal fibula tumors.
Core Tip: Giant cell tumor of the distal fibula is rare, and tibiotalus fusion has not been reported in the treatment of Campanacci III giant cell tumor of the fibula. In this study, the tibial talus joint was fused with three screws, and the follow-up for 2 years showed satisfactory efficacy and no recurrence.
- Citation: Fan QH, Long S, Wu XK, Fang Q. Management of a rare giant cell tumor of the distal fibula: A case report. World J Clin Cases 2023; 11(2): 394-400
- URL: https://www.wjgnet.com/2307-8960/full/v11/i2/394.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i2.394
Giant cell tumor of bone (GCTB) is an intermediate locally aggressive tumor comprised of osteoclast-like multinuclear cells and hyperplastic mononuclear interstitial cells[1,2]. There is a risk of malignant transformation, although it is only described in rare cases[3,4]. GCTB is a rare primary tumor and accounts for 4%-5% of primary bone tumors[5]. It usually involves the metaphyseal-epiphyseal region of the long bones, with about 50% of tumors occurring in the distal femur, proximal tibia, and distal radius[1,5]. The other less common sites are the distal tibia, proximal humerus, proximal femur, and proximal fibula[6-8]. Clinical manifestations include pain, local swelling, effusion, and limited motion of the affected joint. The GCT of the distal fibula is extremely rare, with an incidence of less than 1%[9]. When GCTB is close to the joint, it poses challenges in the surgical management. Lesion resection, prosthesis replacement, or bone graft reconstruction are often used for salvage treatment, but the joint function can still decrease[1,10,11].
A 61-year-old man presented with progressive swelling of the left lateral malleolus accompanied by pain for half a year and aggravation for 2 wk.
Preoperative examination revealed that he had dilated cardiomyopathy with class 3 cardiac function.
The patient’s past medical history was unremarkable.
The patient denied any family history.
There was a long oval mass around the left lateral malleolus, about 10 cm × 6 cm in size. It had normal skin color, soft texture, deep tenderness, and a clear boundary. It had no mobility, and the pronation and rotation functions were limited.
The results such as routine hematological testing, blood sedimentation rate, and tumor-associated markers were normal.
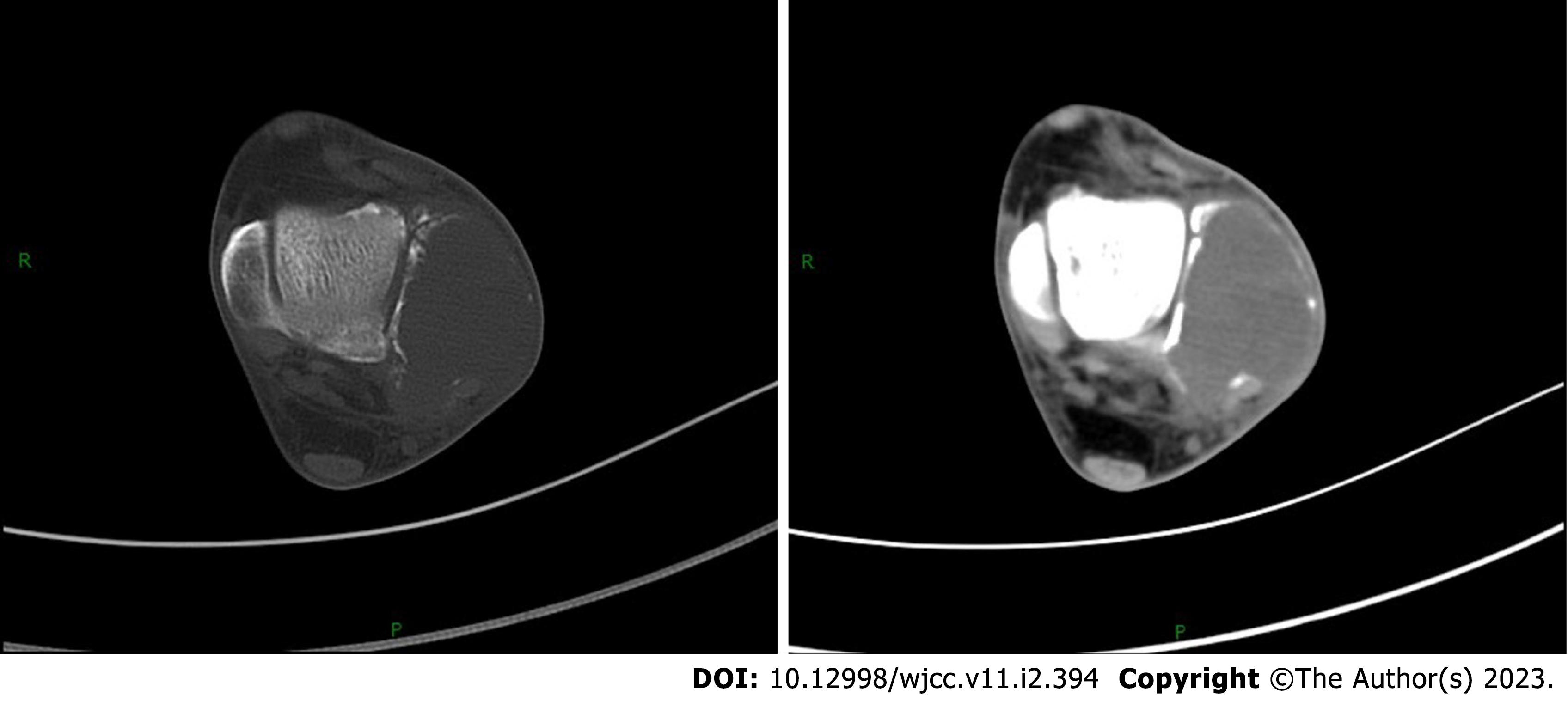
Plain radiographs revealed an expansile lytic lesion in the distal fibula (Figure 1). The ankle computed tomography also showed an expansile lytic lesion with the distal lateral cortex of the fibula invaded (Figure 2). A magnetic resonance imaging scan of his left ankle revealed not only a lytic lesion in the distal fibula but invasion of the soft tissue around the lateral malleolus as well (Figure 3).
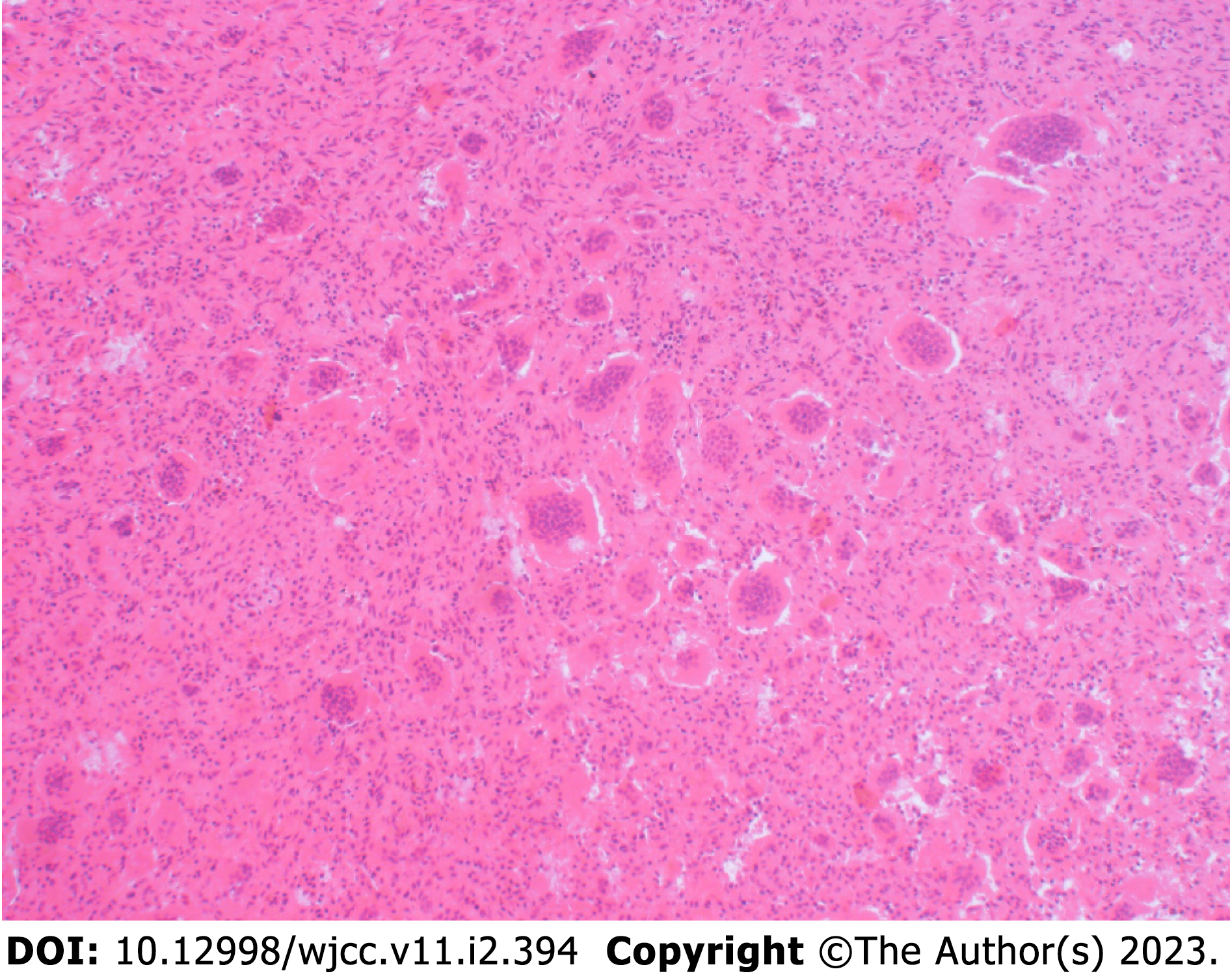
Based on the clinical, radiological, and pathological findings (Figure 4), we confirmed the diagnosis of GCT of the distal fibula (Campanacci Grade III).
The individual therapeutic regimens were discussed and confirmed in a multidisciplinary clinic meeting. We offered three treatment options to the patient, including lesion resection combined with fibula head transplant to stabilize the lateral malleolus, 3D-printed prosthesis to reconstruction, or lesion resection and tibiotalus fusion. The options were discussed with the patient. Although the patient’s heart function was poor, the anesthesiologists and cardiologists concluded that the patient could tolerate the operation, but they recommended to minimize the operation time and the surgical trauma. Because the patient had low requirements for ankle joint function he opted for arthrodesis.
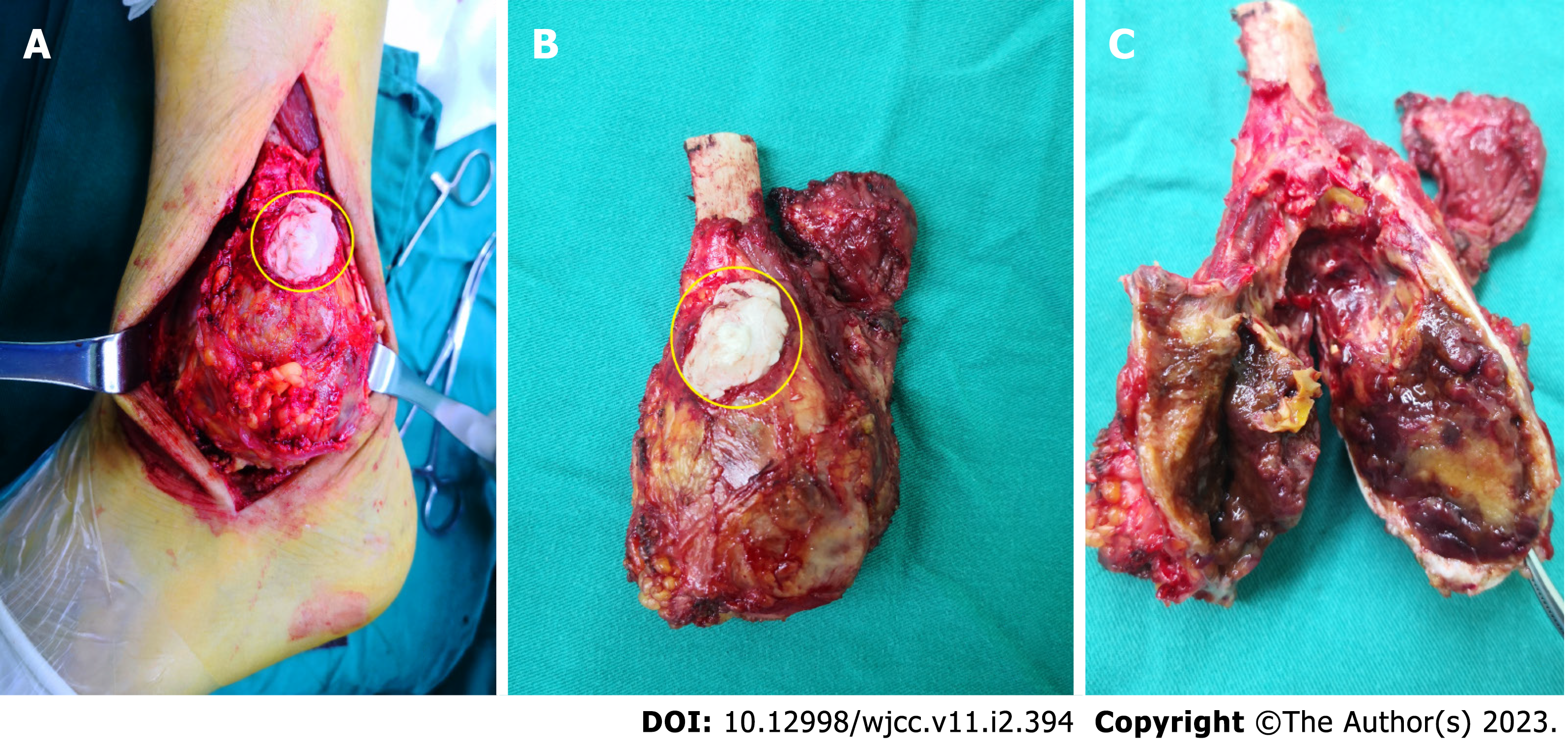
The incision was made along the lateral side of the left lateral malleolus, about 12 cm long. The biopsy incision was fusiform, and subcutaneous separation was performed. It was found that the tumor at the distal peroneal bone had a complete capsule with soft texture and poor mobility. The ligaments at the distal peroneal bone were all invaded and part of the brevis muscle was involved. However, the peroneal longus muscle was not involved. The mass was completely exposed 3 cm above the proximal end of the broken fibula, and the mass, distal ligaments, and soft tissues were completely removed along the fascia space of normal tissue (Figure 5). The joint surface of the medial malleolus was intact, and the tibia and talus were not invaded. The local soft tissue was soaked in distilled water for 10 min. The articular surfaces of the distal tibia and the talus were exposed and removed. After the subchondral bone was combined and flattened, 3 headless compression screws were pressed with compression forceps for fixation. The tibiotalar joint was fixed firmly without micromotion (Figure 6). Next, we sutured the remaining peroneus brevis to the peroneus longus muscle and attached it to the lateral fascia to stabilize the lateral ankle joint. The skin was trimmed, and the incision was sutured. Pressure dressing and plaster cast were used for 6 wk. After 6 wk the plaster was removed, and patient was permitted to partially bear weight. Three months later the patient progressed to full weight bearing.
The patient recovered smoothly after surgery, and the postoperative condition was stable. Three months later he began to walk normally. The patient was asymptomatic during the 2 years of follow-up after the operation. There was no recurrence, and he has had a satisfactory recovery (Figure 7). The patient was advised to continue to follow-up every 3-6 mo.
The lateral malleolus is an important part of the ankle joint, and its distal ligaments are very important for the stability and function of the ankle joint[12-14]. Once the lateral malleolus is invaded by a tumor, it will cause ankle joint dysfunction. GCTs on the bone of the distal fibula are extremely rare[9,15]. It usually occurs in people aged 20-40 years, and the most common sites are in the distal femur, proximal tibia, distal radius, and proximal humerus.
Standard GCT treatment is surgical removal, either by curettage or resection, combined with intraoperative adjuvant therapy[16]; however, some sites may not be amenable to resection, especially near the joint, such as the GCTs of the distal fibula[13,14,17]. Once the articular surface is invaded by a tumor, complete resection is necessary. Due to the importance of its anatomical structure, they are extremely difficult to treat once they occur, and currently there are no guidelines to adopt. Reconstruction treatment such as proximal fibula inversion, allograft, prosthetic replacement, etc. can restore the ankle function to the greatest extent, but external ankle ligament reconstruction has its corresponding difficulties, including soft tissue reconstruction and even rebuilding, and the ligament or tendon-bone healing is still difficult[18-20]. Furthermore, it can lead to long-term complications such as ankle arthritis, joint instability, and pain.
Although reconstructive surgery may improve ankle function, it is time consuming, requires a high cost for reconstruction surgery, and can induce traumatic arthritis, leading to dissatisfaction with the ankle function restoration. Arthrodesis reduces joint function; however the patient can walk without pain and the cost is lower. Therefore, there is no consensus on the best treatment modality. In this case, we first performed pathological biopsy on the patient. In order to avoid tumor spread, we used bone cement to seal the wound cavity. In the fusion procedure, we completely excised the mass and the soft tissue invaded by the tumor, sutured the normal peroneus brevis muscle to the peroneus longus muscle, and then sutured it to the deep fascia surrounding the lateral malleolus to enhance ankle stability. In our experience, arthrodesis is a good option[20].
Tibiotalar fusion and tibiotalocalcaneal fusion are two types of arthrodesis. Tibiotalar fusion is often used in young patients and in patients with good subtalar joints to preserve the range of motion of the subtalar joints[21,22]. Tibiotalar fusion is often used to reconstruct lateral stability, and in this case, the tibiotalar joint was fixed with three screws. The technique has the advantages of requiring less operation time, having a simple operation, and being reliable with effective fixation and good stability of the ankle joint. In addition, it is less invasive and less expensive than prosthetic replacement or reconstruction. After a 2-year follow-up, we concluded that tibiotalar joint fusion by screws was a good option for extensive resection of distal fibula tumors without anatomic reconstruction.
Although the lateral malleolus structure is important, limited excision will only increase the risk of recurrence and pathologic fracture if the distal cortical and ligament structures are damaged by GCTB. Reconstruction can preserve ankle function as much as possible, but there are many complications. Although tibiotalar joint fusion loses the flexion and extension function of the ankle joint, it retains the ankle joint weight-bearing function and can ensure that patients bear weight without pain during walking. Therefore, it can be used as a surgical option for the treatment of distal fibular tumors.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Muthu S, India; Stogov MV, Russia S-Editor: Xing YX L-Editor: Filipodia A P-Editor: Xing YX
| 1. | Montgomery C, Couch C, Emory CL, Nicholas R. Giant Cell Tumor of Bone: Review of Current Literature, Evaluation, and Treatment Options. J Knee Surg. 2019;32:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Werner M. Giant cell tumour of bone: morphological, biological and histogenetical aspects. Int Orthop. 2006;30:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 165] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 3. | Chan CM, Adler Z, Reith JD, Gibbs CP Jr. Risk factors for pulmonary metastases from giant cell tumor of bone. J Bone Joint Surg Am. 2015;97:420-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Rosario M, Kim HS, Yun JY, Han I. Surveillance for lung metastasis from giant cell tumor of bone. J Surg Oncol. 2017;116:907-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Parmeggiani A, Miceli M, Errani C, Facchini G. State of the Art and New Concepts in Giant Cell Tumor of Bone: Imaging Features and Tumor Characteristics. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Đudarić L, Ivanac G, Divjak E, Tomasović Lončarić Č, Petričević Krečak O, Brkljačić B. Giant Cell Tumor of the Distal Ulna: Multimodal Radiological Investigation of a Very Rare Location. Am J Case Rep. 2021;22:e932130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Nagano S, Tsuchimochi T, Yokouchi M, Setoguchi T, Sasaki H, Shimada H, Nakamura S, Ishidou Y, Yamamoto T, Komiya S. Giant cell tumor of the clavicle: report of a case in a rare location with consideration of surgical method. BMC Musculoskelet Disord. 2015;16:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Yadav S, Singhal S, Patel S, Jaiswal S, Mishra R. A Rare Case of Giant-Cell Tumor of Hand in a Young Male. Cureus. 2022;14:e21408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Nadkarni S, Punit AS, Nair RV. Giant Cell Tumour of Distal Fibula Managed by En Block Resection and Reconstruction with Ipsilateral Proximal Fibula. J Orthop Case Rep. 2015;5:52-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Recurrent giant cell tumor of long bones: analysis of surgical management. Clin Orthop Relat Res. 2011;469:1181-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Xu R, Choong PFM. Metastatic giant cell tumour of bone: a narrative review of management options and approaches. ANZ J Surg. 2022;92:691-696. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Aiyer AA, Zachwieja EC, Lawrie CM, Kaplan JRM. Management of Isolated Lateral Malleolus Fractures. J Am Acad Orthop Surg. 2019;27:50-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 13. | Wang J, Du Z, Yang R, Tang X, Guo W. Lateral malleolus en bloc resection for the distal fibula osteosarcoma based on a new classification and proposed reconstruction choice: Analysis of 6 cases prognosis and literature review. Foot Ankle Surg. 2020;26:855-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Vaishya R, Kapoor C, Golwala P, Agarwal AK, Vijay V. A Rare Giant Cell Tumor of the Distal Fibula and its Management. Cureus. 2016;8:e666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Bhowmick K, Boopalan PRJVC. Saving the ankle in distal fibular giant cell tumour - A case report. J Clin Orthop Trauma. 2019;10:1054-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Bukata SV, Blay JY, Rutkowski P, Skubitz K, Henshaw R, Seeger L, Dai T, Jandial D, Chawla S. Denosumab Treatment for Giant Cell Tumor of the Spine Including the Sacrum. Spine (Phila Pa 1976). 2021;46:277-284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Capanna R, van Horn JR, Biagini R, Ruggieri P, Bettelli G, Campanacci M. Reconstruction after resection of the distal fibula for bone tumor. Acta Orthop Scand. 1986;57:290-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Ring A, Kirchhoff P, Goertz O, Behr B, Daigeler A, Lehnhardt M, Harati K. Reconstruction of Soft-Tissue Defects at the Foot and Ankle after Oncological Resection. Front Surg. 2016;3:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Vidal L, Kampleitner C, Brennan MÁ, Hoornaert A, Layrolle P. Reconstruction of Large Skeletal Defects: Current Clinical Therapeutic Strategies and Future Directions Using 3D Printing. Front Bioeng Biotechnol. 2020;8:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 20. | Kundu ZS, Gogna P, Gupta V, Singla R, Sangwan SS, Mohindra M, Singh A. Ankle fusion with centralisation of the fibula after distal tibia bone tumour resection. J Orthop Traumatol. 2014;15:95-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Asomugha EU, Den Hartog BD, Junko JT, Alexander IJ. Tibiotalocalcaneal Fusion for Severe Deformity and Bone Loss. J Am Acad Orthop Surg. 2016;24:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Hanna M, Whicker EA, Traub B, Allam E, Labib SA. Sport activity levels following ankle fusion. Int Orthop. 2021;45:2347-2354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |