Published online Jan 16, 2023. doi: 10.12998/wjcc.v11.i2.357
Peer-review started: September 2, 2022
First decision: October 20, 2022
Revised: November 6, 2022
Accepted: January 5, 2023
Article in press: January 5, 2023
Published online: January 16, 2023
Processing time: 131 Days and 22.7 Hours
Despite the infrequency of trocar site hernias (TSHs), fascial closure continues to be recommended for their prevention when using a ≥ 10-mm trocar.
To identify the necessity of fascial closure for a 12-mm nonbladed trocar incision in minimally invasive colorectal surgeries.
Between July 2010 and December 2018, all patients who underwent minimally invasive colorectal surgery at the Minimally Invasive Surgery Unit of Siriraj Hospital were retrospectively reviewed. All patients underwent cross-sectional imaging for TSH assessment. Clinicopathological characteristics were recorded. Incidence rates of TSH and postoperative results were analyzed.
Of the 254 patients included, 70 (111 ports) were in the fascial closure (closed) group and 184 (279 ports) were in the nonfascial closure (open) group. The median follow up duration was 43 mo. During follow up, three patients in the open group developed TSHs, whereas none in the closed group developed the condition (1.1% vs 0%, P = 0.561). All TSHs occurred in the right lower abdomen. Patients whose drains were placed through the same incision had higher rates of TSHs compared with those without the drain. The open group had a significantly shorter operative time and lower blood loss than the closed group.
Routine performance of fascial closure when using a 12-mm nonbladed trocar may not be needed. However, further prospective studies with cross-sectional imaging follow-up and larger sample size are needed to confirm this finding.
Core Tip: The incidence of trocar site hernias (TSHs) varied from 0.1% to 2%. Previous studies and guidelines have also suggested fascial closure when using a > 10-mm trocar. The findings from this study demonstrated no significant difference in the incidence of TSHs between facial closure and nonclosure groups (0% vs 1.1%, P = 0.561) when the median clinical follow-up duration was 41 mo. Therefore, fascial closure may be selectively omitted when using a 12-mm nonbladed trocar.
- Citation: Krittiyanitsakun S, Nampoolsuksan C, Tawantanakorn T, Suwatthanarak T, Srisuworanan N, Taweerutchana V, Parakonthun T, Phalanusitthepha C, Swangsri J, Akaraviputh T, Methasate A, Chinswangwatanakul V, Trakarnsanga A. Is fascial closure required for a 12-mm trocar? A comparative study on trocar site hernia with long-term follow up. World J Clin Cases 2023; 11(2): 357-365
- URL: https://www.wjgnet.com/2307-8960/full/v11/i2/357.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i2.357
Minimally invasive surgical approaches have gained acceptance worldwide, given their superior benefits in terms of postoperative recovery and wound healing. However, certain complications can occur following laparoscopy, including trocar site hernias (TSHs), the incidence of which varies from 0.1% to 2%[1,2]. Clinical presentation of patients can range from asymptomatic to bowel strangulation in case of delayed diagnosis[3]. Despite the multifactorial etiology of this condition, older age, obesity, and wound infection have been identified to be the predisposing factors[4-6]. Several studies have also suggested fascial defect closure when using a ≥ 10-mm trocar[7-9]. Hence, emphasis should be placed on this preventable condition in high-risk patients.
Similarly, minimally invasive colorectal surgeries have become the standard treatment approach at many centers. Indeed, laparoscopy facilitates meticulous dissection and bowel transection using staplers. Equivalent long-term oncologic outcomes could be achieved by minimizing postoperative morbidities and promoting early recovery of bowel function[10-12]. During the procedure, 12-mm ports are commonly used for 10-mm clips or stapler application. Unlike routine midline incision closure, fascial closure of a 12-mm port incision remains optional. Therefore, we aimed to evaluate the necessity of fascial closure of the 12-mm nonbladed trocar incision made during colorectal surgeries.
This single-center retrospective study was approved by the Siriraj Institutional Review Board (Protocol No. 900/2562). Data were collected from July 2010 to December 2018.
All patients aged ≥ 18 years who underwent nonurgent minimally invasive colorectal surgery at the Minimally Invasive Surgery Unit of Siriraj Hospital, Mahidol University, Thailand, were included. Patients who had incomplete medical records, had connective tissue disease, underwent different fascial closure methods, required conversion to open surgery, < 12 mo of follow up, and did not undergo postoperative cross-sectional imaging were excluded.
We entered the abdominal cavity from the periumbilical region using Hasson’s open technique for laparoscopic surgery or mini-midline incision for hand-assisted laparoscopic surgery to create a pneumoperitoneum. A 12-mm nonbladed trocar was then inserted at a nonperiumbilical location according to the type of surgery. After completing the laparoscopic phase, a mini-midline incision that extended from the periumbilical incision was created for specimen retrieval. A 10-mm abdominal drain was then placed, as specified by the intraoperative findings. The abdominal fascia at the midline incision was closed using a continuous absorbable suture. Closure of the 12-mm trocar site was optional and depended on the surgeon’s preference. The techniques included direct suture with absorbable material and closure under laparoscopic direct vision using the suture passer needle technique. Because of the retrospective nature of our study, details regarding TSHs and repair techniques could not be clearly determined. All patients were followed up using cross-sectional imaging based on the primary disease.
The clinicopathological characteristics of the patients, including age, sex, body mass index, diabetes mellitus, benign prostatic hyperplasia, American Society of Anesthesiologists physical status classification, Modified Charlson Comorbidity Index, serum albumin level, creatinine level, disease diagnosis, type of operation, and number and location of the 12-mm port, were reviewed. The primary outcome was the incidence of TSHs in the nonperiumbilical area, which was diagnosed with postoperative clinical examination or cross-sectional imaging. The date of diagnosis and further management were recorded. Furthermore, details regarding the primary surgery, complications according to the Clavien–Dindo classification[13], and incidence rates of incisional and parastomal hernia were also assessed.
Statistical analyses were performed using SPSS statistical software version 21. The variables were expressed as number (%), mean ± SD, and median with interquartile range (IQR). The data were analyzed using student’s t-test, Mann–Whitney U test, and chi-square test. TSH incidence was analyzed using the Kaplan–Meier curve and log-rank test. P values < 0.05 indicated statistical significance.
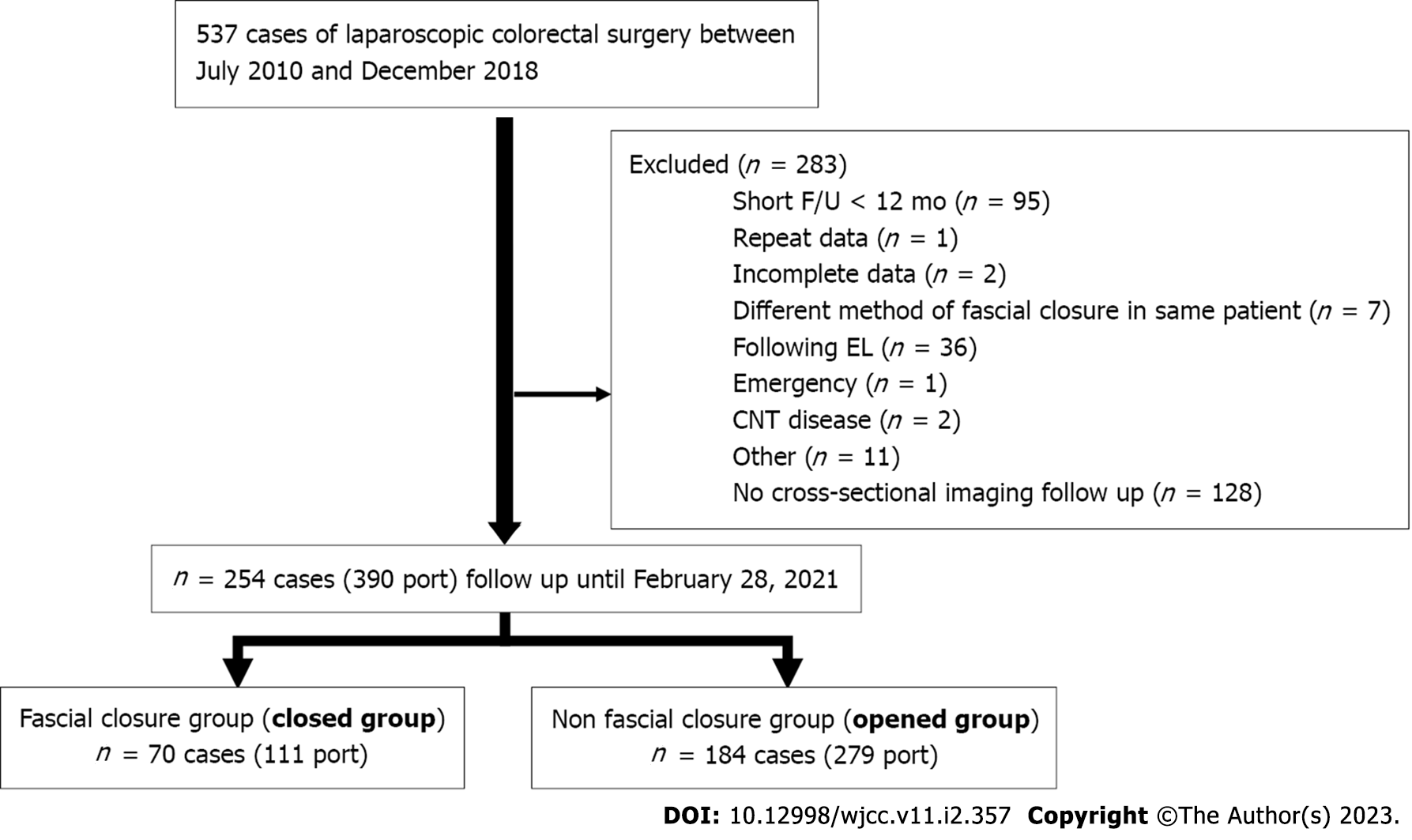
A total of 537 patients with colorectal diseases underwent minimally invasive colorectal surgery. After applying the exclusion criteria, 254 patients (390 ports) were ultimately included in the study. To facilitate comparison, we categorized 70 patients (111 ports) into the fascial closure (closed) group and 184 (279 ports) into the nonfascial closure (open) group (Figure 1). Both groups had comparable baseline characteristics and operative details, except for a higher body mass index in the open group. Table 1 summarizes the clinicopathological characteristics of the patients.
| Closed (n = 70) | Open (n = 184) | P value | |
| Age | 63 ± 12 | 63 ± 11 | 0.461 |
| Male sex | 38 (54.3) | 100 (54.3) | 0.993 |
| Body mass index (kg/m2) | 23 ± 3 | 24 ± 4 | 0.024 |
| Diabetes mellitus | 12 (17.1) | 44 (23.9) | 0.245 |
| Benign prostatic hyperplasia (n = 138) | 3 (7.9) | 9 (9.0) | 1.000 |
| ASA classification | 0.634 | ||
| 1 | 13 (18.6) | 29 (15.8) | |
| 2 | 47 (67.1) | 120 (65.2) | |
| 3 | 10 (14.3) | 35 (19.0) | |
| Modified CCI score | 4 (3.6) | 4 (3.6) | 0.958 |
| Albumin ≥ 3 g/dL | 59 (85.5) | 156 (88.1) | 0.581 |
| Creatinine ≥ 2 mg/dL | 2 (2.9) | 5 (2.7) | 1.000 |
| Disease diagnosis | 0.327 | ||
| Benign | 0 (0) | 5 (2.7) | |
| Malignancy | 70 (100) | 179 (97.3) | |
| Operations | 0.193 | ||
| Right hemicolectomy | 7 (10) | 28 (15.2) | |
| Left hemicolectomy | 29 (41.4) | 57 (31.0) | |
| Subtotal colectomy | 0 (0) | 1 (0.5) | |
| LAR/APR | 32 (45.7) | 97 (52.7) | |
| Total proctocolectomy | 1 (1.4) | 0 (0) | |
| Others | 1 (1.4) | 1 (0.5) | |
| Numbers of 12-mm port per person | 0.511 | ||
| 1 | 29 (41.4) | 90 (48.9) | |
| 2 | 41 (58.6) | 93 (50.5) | |
| 3 | 0 (0) | 1 (0.5) |
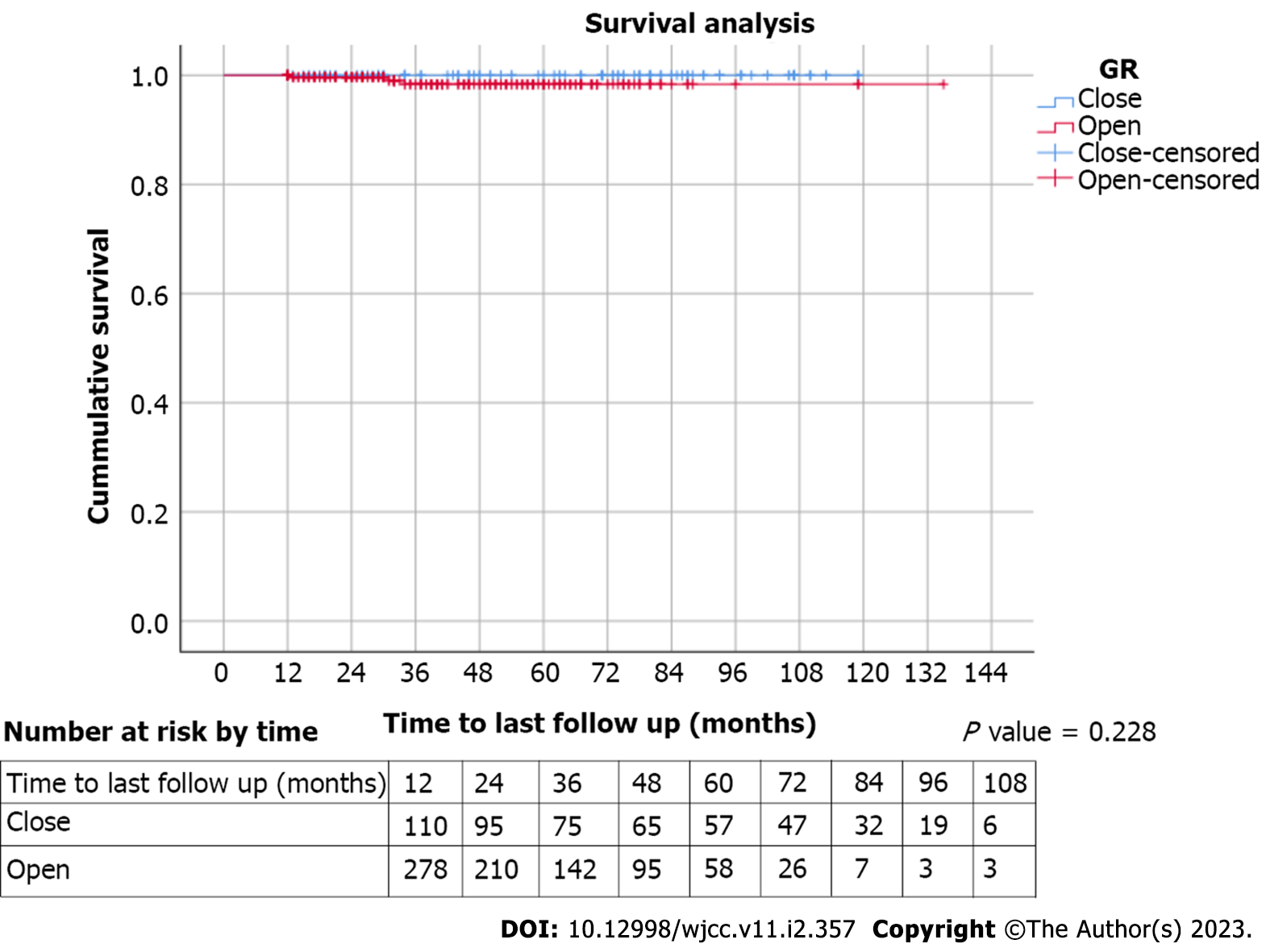
Three patients (3/279 ports, 1.1% per port) in the open group developed TSHs, whereas none in the closed group developed TSHs (0/111 port, 0% per port). There was no significant difference in the incidence of TSHs between the two groups (P = 0.561). The median clinical follow-up duration was 41 mo (IQR 25, 63), whereas the median cross-sectional imaging follow-up duration was 31 mo (IQR 20, 51). Figure 2 demonstrates the Kaplan–Meier analysis of TSH events. Three patients with TSHs were women with adenocarcinoma of the colon who underwent anterior resection. Surveillance computed tomography found that all such patients developed TSHs in the right lower quadrant area containing omental fat. The time to diagnosis ranged from 13 to 34 mo. One patient underwent elective hernia repair at another hospital. Table 2 lists the clinical data. Moreover, one of the three patients developed a concomitant asymptomatic incisional hernia at the midline incision. There were no significant correlations between TSHs and incisional hernia (P = 0.19). None of the patients with TSHs underwent stoma creation during the primary surgery. Subgroup analysis showed that the incidence of TSHs was slightly higher in patients with drain placement than in those without drain placement (3.1% vs 0.5%, P = 0.371).
| Age | BMI | ASA | Alb | Cr | Disease location | Operation | Drain | Time to diagnosis | Treatment | |
| 1 | 77 | 19.9 | 3 | 2.9 | 2.4 | Rectosigmoid | HALS | No | 34 mo | None |
| 2 | 59 | 29.7 | 2 | 4.3 | 0.5 | Sigmoid | Laparoscopic | RLQ | 13 mo | Open repair |
| 3 | 72 | 23.4 | 3 | 4.6 | 1.3 | Sigmoid | HALS | RLQ | 31 mo | None |
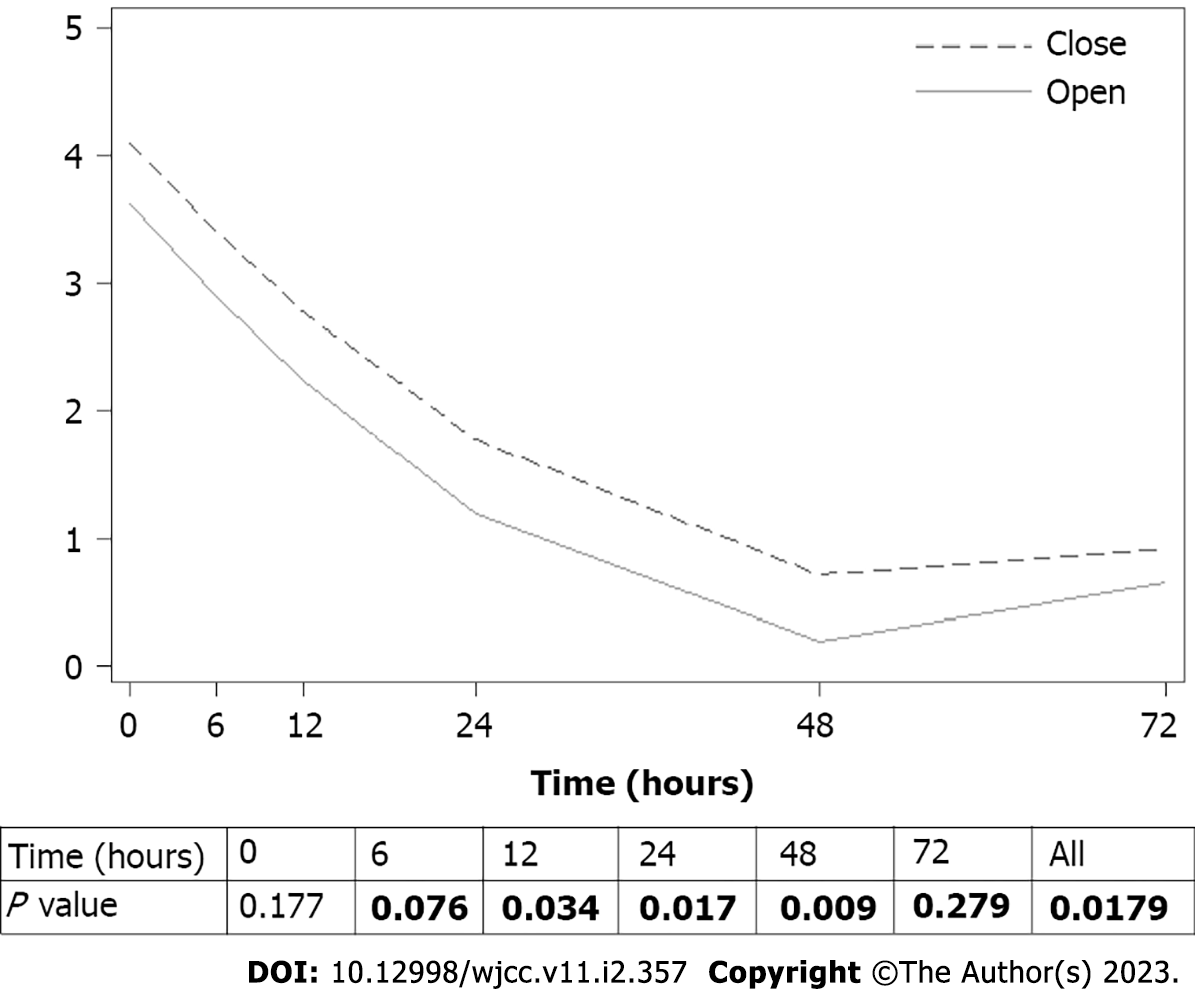
The open group showed shorter operative time and lower blood loss than the closed group. Moreover, the open group experienced significantly lower fitted postoperative pain at 6, 12, 24, and 48 h (P = 0.018) (Figure 3). The length of the hospital stay was comparable between the two groups. No significant difference in complications, such as surgical site infection, anastomosis leakage/bleeding, small bowel obstruction, ileus, arrhythmia, electrolyte imbalance, and urinary tract infection, was observed. In our study, surgical site infection occurred at the midline incision (Table 3).
| Closed (n = 70) | Open (n = 184) | P value | |
| Operative time (minute) | 170 (110, 240) | 123 (100, 185) | 0.004 |
| Estimated blood loss (mL) | 50 (30, 11) | 30 (20, 100) | 0.011 |
| Length of hospital stay (day) | 5 (5, 7) | 5 (4, 6) | 0.122 |
| Complications | 0.228 | ||
| CD-1 | 6 (8.6) | 9 (4.9) | |
| CD-2 | 7 (10) | 10 (5.4) | |
| CD-3 | 2 (2.9) | 3 (1.6) | |
| CD-4, 5 | 0 | 0 |
At present, laparoscopic surgery is a globally acceptable approach across many fields of surgery. Unfortunately, the development of postoperative TSHs remains one of its specific complications. Although prior studies have reported the rare incidence of TSHs after surgery, this complication can be avoided with proper intraoperative management. The predisposing factors for developing hernias may comprise both patient-related instrument-related factors[3,14]. To improve the surgical outcomes and lessen the incidence of TSHs, modifications to the laparoscopic trocar tip have been attempted. Indeed, one study showed that a bladeless trocar allows tissue penetration without cutting the abdominal muscle fibers, which reduces trocar site bleeding and overall complications[15]. However, some laparoscopic instruments may require trocars with larger diameters as working ports. Nonetheless, routine closure of these fascial defects remains controversial. Owing to the potentially harmful consequences, some studies have recommended closing the defect when using a 10-mm trocar[3,16].
Previously, prospective data on other laparoscopic procedures have proven the safety and feasibility of leaving the fascia open after the application of a 10-mm trocar[17]. Our study mainly aimed to determine the necessity of the fascial closure of a 12-mm trocar after minimally invasive colorectal surgeries. Our results demonstrated that routine closure provided no significant benefit. The incidence of TSHs observed in our series was 1.1%, which was comparable to that stated in other reports. All cases underwent cross-sectional imaging based on the index diagnosis. We believe that reliable results were achieved, given that computed tomography is considered one of the best methods for occult hernia detection[18,19]. In 2004, Tonouchi et al[9] classified TSHs into three types. All three cases of TSHs included in this study were of late-onset type. No bowel obstruction or strangulation occurred during the follow-up. Concerning the precipitating factors, only advanced age was found in two patients. None of them were obese or had prior wound infections at the trocar site. Moreover, Sakamoto et al[20] found TSHs after laparoscopic colectomy in elderly patients with low body mass index. Frailty may lead to decreased abdominal wall strength over time. Furthermore, another study found a relationship between TSH incidence and abdominal drain placement. Based on these findings, all patients with TSH also underwent drain placement at the same location of the TSHs after the trocar was removed intraoperatively[20].
Regarding other postoperative results, this study indicated that nonfascial closure, in particular, yielded several advantages. Closure defect usually takes time and may prolong the duration of operation[2]. Postoperative pain is also greater with transfascial suture. However, these parameters may be confounded by various factors. Operative time varies owing to cancer staging or degree of adhesion in benign diseases. The amount of blood loss may be attributed to intraoperative findings or surgical techniques.
Another limitation of our study is its retrospective design. Details regarding the TSHs and repair techniques could not be clearly determined. Given the low TSH rates in our population, factors associated with TSH occurrence could not be identified. Moreover, there was no patient with TSH in the closed group, whereas, 1.1% of TSH was identified in the open group. There was no statistical significance in this study. Further prospective studies with cross-sectional imaging follow-up and larger sample size should be conducted to confirm whether the outcomes of nonfascial closure are not inferior to those of fascial closure.
Fascial closure may be selectively omitted when using a 12-mm nonbladed trocar. To achieve greater benefit from minimally invasive surgery, optimal intraoperative evaluation and decision making are mandatory for TSH prevention.
The incidence of trocar site hernias (TSHs) varies from 0.1% to 2%. Several studies have also suggested fascial defect closure when using a ≥ 10-mm trocar, especially for midline incision and bladed trocar.
The findings from this study imply that there is no significant difference in TSH between the closure and nonclosure groups for 12-mm nonbladed trocar. However, further prospective studies with a larger sample size are required.
To identify the necessity of fascial closure for a 12-mm nonbladed trocar incision in minimally invasive colorectal surgeries.
Closure or nonclosure was decided based on the surgeon’s preference. All patients were followed up via cross-sectional imaging based on the primary disease.
Three patients in the open group developed TSHs, whereas none in the closed group developed TSHs (1.1% vs 0%, P = 0.561). The open group had a significantly shorter operative time and lower blood loss than the closed group.
Fascial closure may be selectively omitted when using a 12-mm nonbladed trocar.
Further prospective studies should be conducted with a larger sample size.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Ferreira GSA, Brazil; Kayano H, Japan; Wani A, India S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Cuesta MA, Bonjer HJ. Treatment of postoperative complication after digestive surgery. Springer; 2014. |
| 2. | Gutierrez M, Stuparich M, Behbehani S, Nahas S. Does closure of fascia, type, and location of trocar influence occurrence of port site hernias? Surg Endosc. 2020;34:5250-5258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Pulle MV, Siddhartha R, Dey A, Mittal T, Malik VK. Port site hernia in laparoscopic surgery: mechanism, prevention and management. Curr Med Res Pract. 2015;5:130-137. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Ciscar A, Badia JM, Novell F, Bolívar S, Mans E. Incidence and risk factors for trocar-site incisional hernia detected by clinical and ultrasound examination: a prospective observational study. BMC Surg. 2020;20:330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Helgstrand F, Rosenberg J, Bisgaard T. Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia. 2011;15:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (1)] |
| 6. | Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA. Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc. 2014;28:3421-3424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East B, Fortelny RH, Gillion JF, Henriksen NA, Israelsson L, Jairam A, Jänes A, Jeekel J, López-Cano M, Miserez M, Morales-Conde S, Sanders DL, Simons MP, Śmietański M, Venclauskas L, Berrevoet F; European Hernia Society. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia. 2015;19:1-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 385] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 8. | Swank HA, Mulder IM, la Chapelle CF, Reitsma JB, Lange JF, Bemelman WA. Systematic review of trocar-site hernia. Br J Surg. 2012;99:315-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 9. | Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trocar site hernia. Arch Surg. 2004;139:1248-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 265] [Article Influence: 13.3] [Reference Citation Analysis (1)] |
| 10. | Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM. Long-term follow-up of the Medical Research Council CLASICC trial of conventional vs laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 495] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 11. | Chern YJ, Hung HY, You JF, Hsu YJ, Chiang JM, Hsieh PS, Tsai WS. Advantage of laparoscopy surgery for elderly colorectal cancer patients without compromising oncologic outcome. BMC Surg. 2020;20:294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Pascual M, Salvans S, Pera M. Laparoscopic colorectal surgery: Current status and implementation of the latest technological innovations. World J Gastroenterol. 2016;22:704-717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24741] [Article Influence: 1178.1] [Reference Citation Analysis (0)] |
| 14. | Sabajo CR, Olthof PB, Roos D, Dekker JWT. Incisional Hernia After Laparoscopic-Assisted Right Hemicolectomy. World J Surg. 2019;43:3172-3178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Blunt vs bladed trocars in laparoscopic surgery: a systematic review and meta-analysis of randomized trials. Surg Endosc. 2013;27:2312-2320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Pamela D, Roberto C, Francesco LM, Umberto M, Carla M, Vincenzo N, Stefano T, Eriberto F, Daniele G, Angelo D, Diego M, Micol Sole DP, Alessandro S, Maurizio B, Vito S, Nicola A, Francesco S. Trocar site hernia after laparoscopic colectomy: a case report and literature review. ISRN Surg. 2011;2011:725601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Singal R, Zaman M, Mittal A, Singal S, Sandhu K. No Need of Fascia Closure to Reduce Trocar Site Hernia Rate in Laparoscopic Surgery: A Prospective Study of 200 Non-Obese Patients. Gastroenterology Res. 2016;9:70-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Kroese LF, Sneiders D, Kleinrensink GJ, Muysoms F, Lange JF. Comparing different modalities for the diagnosis of incisional hernia: a systematic review. Hernia. 2018;22:229-242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 19. | Naguib N, Rafique H, Dhruva Rao PK, Longworth T, Soukias JM, Masoud A. A review of the incidence of iatrogenic hernia in both laparoscopic and open colorectal surgery: Using CT as the gold standard of detection, cohort study. Int J Surg. 2015;19:87-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Sakamoto K, Tashiro Y, Ono S, Sugimoto K, Ishiyama S, Yaginuma Y, Komiyama H, Kojima Y, Tanaka M, Goto M, Sengoku H, TomikiI Y. Trocar site hernia after laparoscopic colectomy. J Japanese College Surg. 2009;34:162-166. [DOI] [Full Text] |