Published online Jan 16, 2023. doi: 10.12998/wjcc.v11.i2.308
Peer-review started: September 20, 2022
First decision: November 15, 2022
Revised: November 24, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 16, 2023
Processing time: 114 Days and 1.1 Hours
Patients with inflammatory bowel disease (IBD) require lifelong and personalized care by a multidisciplinary healthcare team. However, the traditional medical model is not ideal for patients who require continuous close monitoring and whose symptoms may dramatically worsen between regularly scheduled visits. Additionally, close dietary follow-up and monitoring of IBD in a traditional setting are challenging because of the disease complexity, high pressure on outpatient clinics with a small number of IBD specialist dietitians, and rising incidence. Given the significant burden of IBD, there is a need to develop effective dietary management strategies. The coronavirus disease 2019 pandemic caused an unprecedented shift from in-person care to delivering health care via technological remote devices. Traditional nutrition therapy and consultation can be provided by telenutrition through remote electronic communication applications that could greatly benefit patient care. Telenutrition might be useful, safe, and cost-effective compared with standard care. It is likely that virtual care for chronic diseases including IBD will continue in some form into the future. This review article summarizes the evidence about telenutrition applications in the management of IBD patients, and we gave an overview of the acceptance and impact of these interventions on health outcomes.
Core Tip: Routine nutritional assessment, education, and close communication about diet are essential for professionally recommended diets, and they are a potential therapeutic strategy for inflammatory bowel disease onset and severity. Traditional nutrition therapy and consultation can be provided by telenutrition through remote electronic communication applications, which could greatly benefit patient care. Telenutrition is a self-management tool offering cost-effective, quick, and accessible personalized dietary advice for inflammatory bowel disease patients that require lifelong follow-up and maintenance treatment. However, there are certain barriers to legacies, education, sufficient equipment, and privacy. Further studies and interventions should focus on removing barriers while improving benefits.
- Citation: Güney Coşkun M, Kolay E, Basaranoglu M. Telenutrition for the management of inflammatory bowel disease: Benefits, limits, and future perspectives. World J Clin Cases 2023; 11(2): 308-315
- URL: https://www.wjgnet.com/2307-8960/full/v11/i2/308.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i2.308
Inflammatory bowel disease (IBD) is a relapsing disease manifested by focal asymmetric, transmural, and granulomatous inflammation, which includes ulcerative colitis and Crohn’s disease[1]. Ethnic origin, genetics, gut microbiome, environmental factors, immune response, and lifestyle are the main factors in the epidemiology of this disease[2]. The incidence IBD has increased from 0.5% in 2010 to 0.75% in 2020, and it is expected to rise to > 1% of the population by 2030[3]. This will result in a high demand for health care worldwide[4,5]. IBD is characterized by active disease (flares), remission periods, and symptoms that may dramatically worsen between regularly scheduled visits. Inadequate clinical management might result in irreversible intestinal fibrosis and even cancer[6-8].
Diet is considered a potential therapeutic strategy for IBD onset and severity. IBD specified nutrition care could have an anti-inflammatory effect, regulate the immune system, support the mucous layer, contribute to microbial healing, and other mechanisms. The International Organization for the Study of IBD revealed dietary guidance based on the best current evidence[9]. Dietary recommendations include regular intake of fruits and vegetables (in remission) and reduce saturated, trans, and dairy fat intake for patients with Crohn’s disease. The dietary practice focuses on increasing the consumption of natural sources of omega-3 fatty acids while decreasing the consumption of saturated, trans, dairy fat, and red and processed meat for patients with ulcerative colitis[9]. Although several dietary patterns (such as the Mediterranean diet, specific carbohydrate diet, and Crohn’s disease exclusion diet) are commonly recommended for patients with IBD, a personalized approach and close monitoring are the key to successful nutritional support[10-12]. Additionally, diet recommendations and characteristics of the diet may differ depending on whether the patient’s disease is acute or in remission, the medication type, perianal abscess fistula if stricture development is present, and pre- and post-operative status[9,13].
On the other hand, malnutrition and body mass index of people with obesity are predictive factors for IBD[2]. In order to determine unintentional weight loss, rapid weight gain, and nutritional deficiencies, nutrition consultation should be provided as early-stage dietetic support[14]. Furthermore, close dietary follow-up and monitoring of IBD in a traditional setting are challenging due to the disease complexity, the limited number of IBD specialist dietitians in outpatient clinics, and rising disease incidence. The British Society of Gastroenterology consensus guidelines suggests that 0.5 whole-time equivalent dietitians should be allocated to gastroenterology per population of 250000[15]. Along with that, IBD patients require continuous, close, and personalized monitoring to minimize short-term and long-term undesirable outcomes. However, the traditional medical model for IBD care may not be ideal for patients who require lifelong and personalized care by a multidisciplinary healthcare team (gastroenterologists, surgeons, nurse practitioners, psychologists, and dietitians).
The traditional medical model for IBD offers a routine follow-up visit depending on disease history, phenotype, activity, and current treatment, including regular disease monitoring tests (clinical, biochemical, stool, endoscopic, cross-sectional imaging, and histological investigations)[2]. The clinical follow-up timeline given by the ECCO-ESGAR Guideline recommends that in patients with IBD who have reached clinical and biochemical remission, monitoring ensures early recognition of the disease flare[2]. The interval of monitoring should be between 3-6 mo depending upon the duration of remission and current therapy. Moreover, endoscopic surveillance should be performed to detect changes from 1-5 years depending on risk factors[2]. Therefore, this study aimed to review the literature on the benefits and limits of telenutrition in IBD nutrition care and provide future perspectives to improve telenutrition applications.
In broad terms, telemedicine can be defined as the transfer of health resources and health care in distance conditions. The telemedicine term embodies many concepts that cover telemonitoring, tele-education, teleconsultation, and telecare as well as m-health[16]. According to a definition provided by The American Telemedicine Association, it also aims to improve a patient’s clinical health status[17]. The transformation of IBD care is rapidly rising after coronavirus disease 2019 (COVID-19) through novel approaches to telemedicine with targeting convenient access and well-tolerated IBD care. The ECCO Position Statement on IBD management during the COVID-19 outbreak recommended implementing telemedicine, monitoring at distance, reporting outcomes online, promoting local labs with e-mail reports, implementing point-of-care biomarkers, calprotectin measurement at home, and measurement of drug levels (therapeutic drug monitoring) with rapid tests[2].
On the other hand, most of the IBD patients experienced psychological distress and were inadequately informed about the management of their chronic condition during the COVID-19 pandemic[18,19]. A vital issue is considering the psychological well-being of the patients, detecting vulnerable groups via various questionnaires, and preventing stigmatization during the consultation[20-22]. Therefore, switching to telemedicine as an alternative first-choice follow-up tool supporting therapeutic adherence is highly recommended after the pandemic.
Given the significant burden of IBD, there is a need to develop effective dietary management strategies. Traditional nutrition therapy and consultation can be provided by telenutrition through remote electronic communication applications that could greatly benefit patient care. Telenutrition is one of the major components of telemedicine, and the Academy of Nutrition and Dietetics characterized it as virtual dietary consultations including telecommunications technologies to apply the Nutrition Care Process[23]. In recent years, there has been an increasing interest in telenutrition applications for the long-term monitoring and nutrition management of chronic diseases[24]. A growing body of literature follows this statement: Telenutrition is becoming a suggested strategy to overcome barriers and increase access to nutrition care[25]. Consequently, the transition to telenutrition practices in IBD can be promising to overcome the barriers and challenges that arise in the nutrition care of the disease.
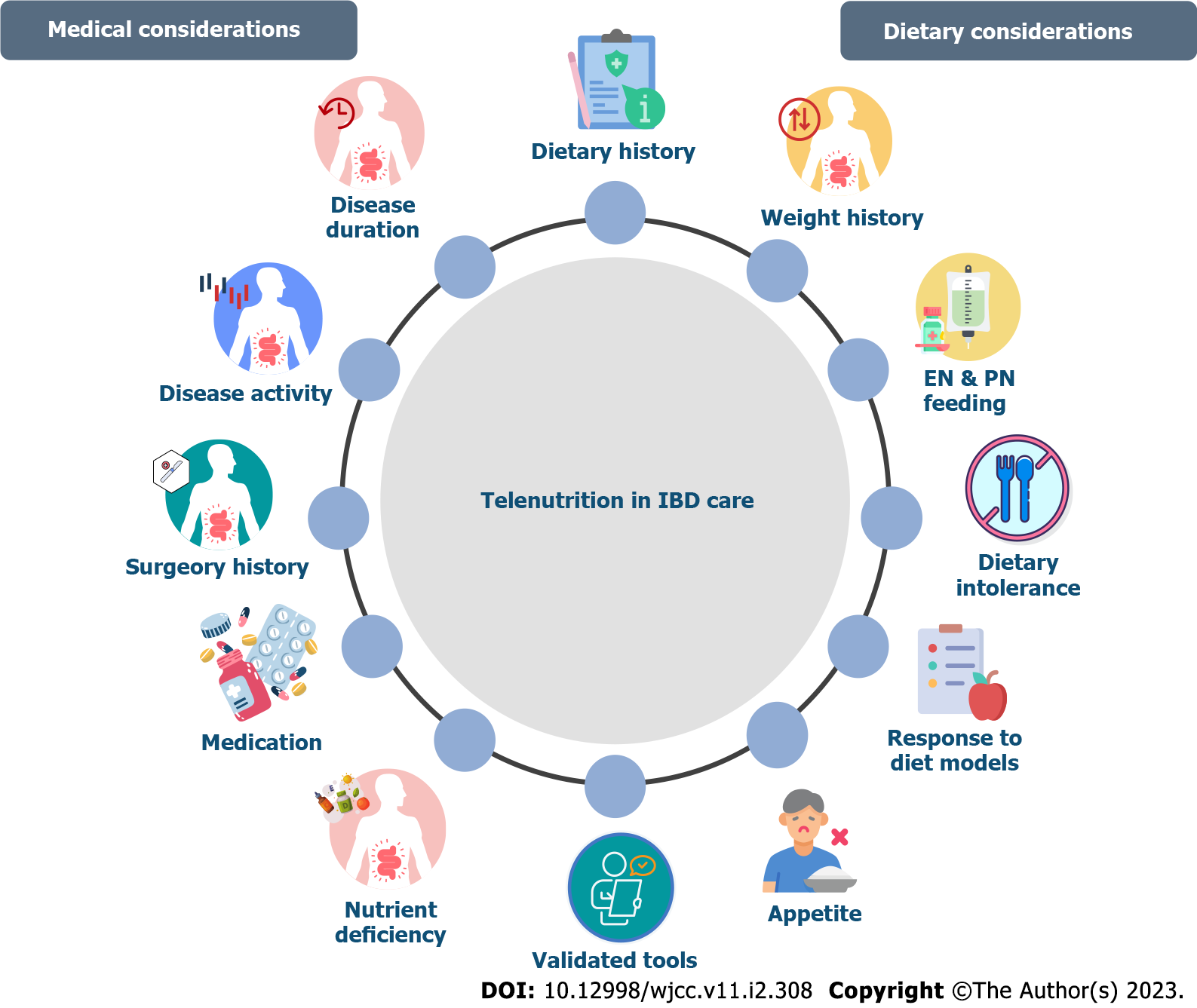
Telemedicine is most frequently transmitted through the internet via high-quality web portals, online courses, smartphone applications, or telephone[26]. Telenutrition modules can implement applications to complete IBD patient care. Dietitians who specialized in IBD could also be involved in applying and operating most telemedicine interventions and projects. Routine nutritional assessment, education, and close communication about diet are essential for professionally recommended diet and dietary restrictions to control symptoms, and long-term monitoring of behaviors that may trigger symptoms[27]. Additionally, various factors and nutritional factors can affect patient health and quality of life[28]. Therefore, telenutrition as a communication method could be considered to meet individual patients’ requests. A comprehensive medical history of IBD patients should be recorded at the first consultation. Assessment tools are also useful for ensuring a consistent approach and can be used by dietitians during initial and follow-up telenutrition visits. Validated tools for objective measures include the IBD questionnaire[29], which is considered the gold standard for use in clinical trials, food-related quality of life[30], Subjective Global Assessment, the Malnutrition Universal Screening Tool, Malnutrition Inflammation Risk Tool, Saskatchewan IBD Nutrition Risk Tool, and Nutrition Risk Screening 2002[31] and could be appropriate and useful in certain situations. Monitoring and identifying psychological dimensions that could affect the clinical course of the disease with various approaches would be useful in determining the psychological effects of nutrition[32]. Additionally, micronutrient deficiencies should be assessed in the beginning and reassessed as needed. Deficits can occur even in apparently well-nourished patients or in patients without laboratory results[33]. Patients on elimination diets, who present with symptoms of deficiency or who meet < 75% of estimated energy requirements for > 1 mo should be monitored closely. Last but not least nutritional education must be included in telenutrition consultations. Figure 1 summarized the telenutrition in IBD care with medical and dietary considerations, which can be implemented in the first consultation and long-term monitoring of IBD patients.
The benefits of telemedicine can be listed under several headings: access and monitoring; cost-effectiveness; information sharing; and communication between health professionals and patients[34]. An umbrella review that investigated the clinical effectiveness of telemedicine revealed that it can positively affect diet and lifestyle-related factors such as improvement in glycemic control in diabetic patients, helping patients increase physical activity, and improving diet quality and nutrition[35]. Telemedicine technology enhances the accessibility of medical data and healthcare professional monitoring of patients[34]. Accessibility to telehealth applications including telenutrition has grown rapidly during the COVID-19 pandemic time due to contact limitations[36]. The results from a survey study conducted in Italy demonstrated that after the COVID-19 pandemic, the accessibility of telenutrition increased from 16% to 63%[37]. Australia’s study on reimbursed telehealth dietetics services showed that telehealth items for dietitians have increased by 17.7% and represent 5% of total dietetics services provided by telemedicine[38].
Moreover, financial burdens and difficulties can be considered key barriers for patients with IBD to obtain healthcare services[39]. Existing research recognizes the financial contribution of telehealth considering the importance of cost-effectiveness and cost-saving in the healthcare system. Collective data supported the economic benefits of m-health usage compared to traditional applications[40]. These results seem to be consistent with other research that found videoconferencing can be cost-saving and highly effective for patients with IBD[41]. It is important to consider that the majority of studies investigate telehealth rather than telenutrition. Although the results obtained from telehealth studies can be extrapolated to telenutrition, it should be noted that diet-related factors may affect the outcomes. The improvement in telehealth technologies is unlikely to cause significant increases in cost or access and will assist the population to support a healthier diet to fight against chronic disease outcomes.
Telemedicine is particularly beneficial for IBD patients for treatment management, education, self-reported disease activity, and outcomes[42]. A recent review reported mixed results when comparing face-to-face visits with telemedicine visits[42]. Most IBD-related apps allow patients to record symptoms, bowel habits, and dietary history to log meals, nutrition, medications, and mood[43-45]. Telemedicine systems become prominent in being safe, feasible, cost-effective, meeting patients’ needs, and overcoming distance barriers between patients and healthcare facilities[44]. Several telemedicine systems for IBD patients that provide nutritional support are listed in Table 1.
| Ref. | Study/application | Country | Design | n | Benefits for nutritional aspects |
| Habashi et al[46], 2019 | Promoting access and care through centers of excellence | Canada | Prospective comparative study | 90 patients with IBD | Including IBD nutrition expert in the health care team. Providing frequent consultations, reducing wait times and cost savings |
| Ehrlich et al[47], 2012 | GI buddy | Crohn’s and Colitis Foundation | Application | N/A | Allowing patients to record their symptoms, bowel movements, diet, physical activity, and medication adherence, notes, questions, or doubts for the next clinician interaction. Helping patients and healthcare team see how IBD may be affecting patients, improving IBD management and quality of life |
| Oshi Health[48], 2022 | Oshi Health | United States | Application | N/A | Providing nutrition and dietary support, health coaching, IBD-friendly recipes, provides a space to message with professionals, symptom tracking |
| de Jong et al[49], 2017 | myIBDcoach | Netherlands | Randomized controlled trial | 909 patients with IBD (n = 465 telemedicine, n = 444 standard care) | Providing eLearning modules about medications, adherence, smoking cessation, nutrition, symptom management, fatigue, work productivity, anxiety, and depression. Showing plan and messaging care team, weekly or monthly assessment (monitor IBD at home questionnaire) according to disease severity |
| Gupta et al[50], 2022 | IBD NutriCare | India | Prospective observational study | 49 patients with IBD | Recording daily diet and other disease-related parameters to provide timely telenutrition counselling, comprehensive analysis report including nutrient intake, calorie distribution of patient’s daily intake, and weight records, giving answers, frequently asked questions about diet in IBD, sending notifications or message from the dietitians |
In spite of all mentioned benefits of telemedicine, there are certain limitations that are necessary to consider. The most important limitations are legal and ethical issues including privacy protection, difficulties with equipment, educating patients and health professionals in the usage of telenutrition, patient-centered barriers, and financial sources spent on system adjustments[51,52]. Telemedicine systems may not be appropriate for patients who do not have well-established treatment plans. Furthermore, patients may not be familiar with the technological applications or must invest extensive time to become familiar. Also, it must be underlined that studies were mainly conducted in developed countries, and there might be differences in terms of equipment quality and internet availability in some countries[40]. Telemedicine settings in low and low-middle income countries may be limited by financial elements and interference with the cost-effectiveness[40]. Besides the financial barrier, careful consideration must be given to patient privacy and data protection. There is a need for further improvement from both the clinical dietetic practice and patient perspective. Even though the results of limited study samples cannot be generalized, evidence shows that telenutrition has a significant impact on patient education, treatment adherence, medication management, quality of life, and care[42].
Besides limitations related to telemedicine, nutrition-specific barriers must be recognized in overcoming possible obstacles. Considering that anthropometric measurements are essential compo
Digital health interventions and self-monitoring offer quick, cost-effective, personalized, accessible medical care and nutritional advice[53]. Especially when considering the rising number of IBD patients and an insufficient number of specialists, telemedicine could reduce the burden on the healthcare system by providing digital sources. Patients with less aggressive disease severity or in remission can likewise be followed up via telenutrition applications supported by a dietitian. However, studies showed some barriers, and it is not yet proven if telemedicine monitoring can change the natural disease course of IBD. Future studies with larger sample sizes are needed to evaluate the telenutrition side of digital health interventions in the following areas: (1) Nutritional assessment accuracy, dietary model acceptability, telenutrition effectiveness, and self-management of dietary triggers; (2) Dietary recommendations through artificial intelligence need proper validation and investigation of their clinical utility in real-life settings before recommending clinical use; (3) More ease-of-use virtual interface adaptations are needed for delivering telenutrition for dietitians and populations including the elderly or with limited digital literacy; and (4) Standard telenutrition care procedure need to be established and include data protection systems to ensure patient privacy and security[54].
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Behera B, India; Gravina AG, Italy S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Basaranoglu M, Sayilir A, Demirbag AE, Mathew S, Ala A, Senturk H. Seasonal clustering in inflammatory bowel disease: a single centre experience. Expert Rev Gastroenterol Hepatol. 2015;9:877-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Kucharzik T, Ellul P, Greuter T, Rahier JF, Verstockt B, Abreu C, Albuquerque A, Allocca M, Esteve M, Farraye FA, Gordon H, Karmiris K, Kopylov U, Kirchgesner J, MacMahon E, Magro F, Maaser C, de Ridder L, Taxonera C, Toruner M, Tremblay L, Scharl M, Viget N, Zabana Y, Vavricka S. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J Crohns Colitis. 2021;15:879-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 248] [Article Influence: 62.0] [Reference Citation Analysis (32)] |
| 3. | Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 731] [Article Influence: 182.8] [Reference Citation Analysis (0)] |
| 4. | Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769-2778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2677] [Cited by in RCA: 4052] [Article Influence: 506.5] [Reference Citation Analysis (110)] |
| 5. | Coward S, Clement F, Benchimol EI, Bernstein CN, Avina-Zubieta JA, Bitton A, Carroll MW, Hazlewood G, Jacobson K, Jelinski S, Deardon R, Jones JL, Kuenzig ME, Leddin D, McBrien KA, Murthy SK, Nguyen GC, Otley AR, Panaccione R, Rezaie A, Rosenfeld G, Peña-Sánchez JN, Singh H, Targownik LE, Kaplan GG. Past and Future Burden of Inflammatory Bowel Diseases Based on Modeling of Population-Based Data. Gastroenterology. 2019;156:1345-1353.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 317] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 6. | Frigerio S, Lartey DA, D'Haens GR, Grootjans J. The Role of the Immune System in IBD-Associated Colorectal Cancer: From Pro to Anti-Tumorigenic Mechanisms. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Argov S, Sahu RK, Bernshtain E, Salman A, Shohat G, Zelig U, Mordechai S. Inflammatory bowel diseases as an intermediate stage between normal and cancer: a FTIR-microspectroscopy approach. Biopolymers. 2004;75:384-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Hemminki K, Li X, Sundquist J, Sundquist K. Cancer risks in Crohn disease patients. Ann Oncol. 2009;20:574-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Levine A, Rhodes JM, Lindsay JO, Abreu MT, Kamm MA, Gibson PR, Gasche C, Silverberg MS, Mahadevan U, Boneh RS, Wine E, Damas OM, Syme G, Trakman GL, Yao CK, Stockhamer S, Hammami MB, Garces LC, Rogler G, Koutroubakis IE, Ananthakrishnan AN, McKeever L, Lewis JD. Dietary Guidance From the International Organization for the Study of Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2020;18:1381-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 184] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 10. | Sasson AN, Ananthakrishnan AN, Raman M. Diet in Treatment of Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2021;19:425-435.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 72] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 11. | Limketkai BN, Gordon M, Mutlu EA, De Silva PS, Lewis JD. Diet Therapy for Inflammatory Bowel Diseases: A Call to the Dining Table. Inflamm Bowel Dis. 2020;26:510-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Sood A, Ahuja V, Kedia S, Midha V, Mahajan R, Mehta V, Sudhakar R, Singh A, Kumar A, Puri AS, Tantry BV, Thapa BR, Goswami B, Behera BN, Ye BD, Bansal D, Desai D, Pai G, Yattoo GN, Makharia G, Wijewantha HS, Venkataraman J, Shenoy KT, Dwivedi M, Sahu MK, Bajaj M, Abdullah M, Singh N, Abraham P, Khosla R, Tandon R, Misra SP, Nijhawan S, Sinha SK, Bopana S, Krishnaswamy S, Joshi S, Singh SP, Bhatia S, Gupta S, Ghoshal UC. Diet and inflammatory bowel disease: The Asian Working Group guidelines. Indian J Gastroenterol. 2019;38:220-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Guney M, Basaranoglu M. A patient with Crohn's disease during remission by biological agent treatment developed active pulmonary tuberculosis and determining the eating habits. Eur J Gastroenterol Hepatol. 2020;32:541-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Fitzpatrick JA, Melton SL, Yao CK, Gibson PR, Halmos EP. Dietary management of adults with IBD - the emerging role of dietary therapy. Nat Rev Gastroenterol Hepatol. 2022;19:652-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 15. | Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, Barrett KJ, Davies RJ, Bennett C, Gittens S, Dunlop MG, Faiz O, Fraser A, Garrick V, Johnston PD, Parkes M, Sanderson J, Terry H; IBD guidelines eDelphi consensus group, Gaya DR, Iqbal TH, Taylor SA, Smith M, Brookes M, Hansen R, Hawthorne AB. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1-s106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1402] [Cited by in RCA: 1539] [Article Influence: 256.5] [Reference Citation Analysis (0)] |
| 16. | Perisetti A, Goyal H. Successful Distancing: Telemedicine in Gastroenterology and Hepatology During the COVID-19 Pandemic. Dig Dis Sci. 2021;66:945-953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 17. | Telehealth Basics-ATA. [cited 15 July 2022]. Available from: https://www.americantelemed.org/resource/why-telemedicine/. |
| 18. | Spina A, Mazzarella C, Dallio M, Romeo M, Pellegrino R, Durante T, Romano M, Loguercio C, Di Mauro M, Federico A, Gravina AG. The Lesson from the First Italian Lockdown: Impacts on Anxiety and Depressive Symptoms and Sleep Quality in Patients with Remission of Inflammatory Bowel Disease. Rev Recent Clin Trials. 2022;17:109-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (2)] |
| 19. | Pellegrino R, Pellino G, Selvaggi F, Federico A, Romano M, Gravina AG. Therapeutic adherence recorded in the outpatient follow-up of inflammatory bowel diseases in a referral center: Damages of COVID-19. Dig Liver Dis. 2022;54:1449-1451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (5)] |
| 20. | Guo L, Rohde J, Farraye FA. Stigma and Disclosure in Patients With Inflammatory Bowel Disease. Inflamm Bowel Dis. 2020;26:1010-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Roberts CM, Baudino MN, Gamwell KL, Edwards CS, Traino KA, Tung J, Grunow JE, Jacobs NJ, Mullins LL, Chaney JM. Illness Stigma, Worry, Intrusiveness, and Depressive Symptoms in Youth With Inflammatory Bowel Disease. J Pediatr Gastroenterol Nutr. 2021;72:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 966] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 23. | Peregrin T. Telehealth Is Transforming Health Care: What You Need to Know to Practice Telenutrition. J Acad Nutr Diet. 2019;119:1916-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Lewinski AA, Walsh C, Rushton S, Soliman D, Carlson SM, Luedke MW, Halpern DJ, Crowley MJ, Shaw RJ, Sharpe JA, Alexopoulos AS, Tabriz AA, Dietch JR, Uthappa DM, Hwang S, Ball Ricks KA, Cantrell S, Kosinski AS, Ear B, Gordon AM, Gierisch JM, Williams JW Jr, Goldstein KM. Telehealth for the Longitudinal Management of Chronic Conditions: Systematic Review. J Med Internet Res. 2022;24:e37100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 25. | Elamin S, Cohen J. Telenutrition for Inflammatory Bowel Disease: A Tipping Point for Dietary Wellness. Crohns Colitis 360. 2021;3:otab017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Pang L, Liu H, Liu Z, Tan J, Zhou LY, Qiu Y, Lin X, He J, Li X, Lin S, Ghosh S, Mao R, Chen M. Role of Telemedicine in Inflammatory Bowel Disease: Systematic Review and Meta-analysis of Randomized Controlled Trials. J Med Internet Res. 2022;24:e28978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 27. | Devlen J, Beusterien K, Yen L, Ahmed A, Cheifetz AS, Moss AC. The burden of inflammatory bowel disease: a patient-reported qualitative analysis and development of a conceptual model. Inflamm Bowel Dis. 2014;20:545-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 28. | Toruner M, Basaranoglu M, Atug O, Senturk O, Akyuz F, Cekic C, Over Hamzaoglu H, Tekin F, Sezgin O, Akpinar H, Celik AF, Tezel A, Gokturk HS, Kav T. Improvement of Work Productivity and Quality of Life with Anti-Tumor Necrosis Factor Treatment Used in Crohn's Disease in Routine Clinical Practice in Turkey. Turk J Gastroenterol. 2022;33:406-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804-810. [PubMed] [DOI] [Full Text] |
| 30. | Hughes LD, King L, Morgan M, Ayis S, Direkze N, Lomer MC, Lindsay JO, Whelan K. Food-related Quality of Life in Inflammatory Bowel Disease: Development and Validation of a Questionnaire. J Crohns Colitis. 2016;10:194-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 31. | Li S, Ney M, Eslamparast T, Vandermeer B, Ismond KP, Kroeker K, Halloran B, Raman M, Tandon P. Systematic review of nutrition screening and assessment in inflammatory bowel disease. World J Gastroenterol. 2019;25:3823-3837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (2)] |
| 32. | Barreiro-de Acosta M, Marín-Jiménez I, Panadero A, Guardiola J, Cañas M, Gobbo Montoya M, Modino Y, Alcaín G, Bosca-Watts MM, Calvet X, Casellas F, Chaparro M, Fernández Salazar L, Ferreiro-Iglesias R, Ginard D, Iborra M, Manceñido N, Mañosa M, Merino O, Rivero M, Roncero O, Sempere L, Vega P, Zabana Y, Mínguez M, Nos P, Gisbert JP. Recommendations of the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) and the Association of Crohn's Disease and Ulcerative Colitis Patients (ACCU) in the management of psychological problems in Inflammatory Bowel Disease patients. Gastroenterol Hepatol. 2018;41:118-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Nazarenkov N, Seeger K, Beeken L, Ananthakrishnan AN, Khalili H, Lewis JD, Konijeti GG. Implementing Dietary Modifications and Assessing Nutritional Adequacy of Diets for Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y). 2019;15:133-144. [PubMed] |
| 34. | Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 426] [Article Influence: 106.5] [Reference Citation Analysis (3)] |
| 35. | Eze ND, Mateus C, Cravo Oliveira Hashiguchi T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One. 2020;15:e0237585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 180] [Cited by in RCA: 173] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 36. | Rozga M, Handu D, Kelley K, Jimenez EY, Martin H, Schofield M, Steiber A. Telehealth During the COVID-19 Pandemic: A Cross-Sectional Survey of Registered Dietitian Nutritionists. J Acad Nutr Diet. 2021;121:2524-2535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 37. | Gnagnarella P, Ferro Y, Monge T, Troiano E, Montalcini T, Pujia A, Mazza E. Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Kelly JT, Ahmadvand A, Snoswell C, Ball L. How have temporary Medicare telehealth item numbers impacted the use of dietetics services in primary care settings? Nutr Diet. 2022;79:481-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Yu Q, Zhu C, Feng S, Xu L, Hu S, Chen H, Yao S, Wang X, Chen Y. Economic Burden and Health Care Access for Patients With Inflammatory Bowel Diseases in China: Web-Based Survey Study. J Med Internet Res. 2021;23:e20629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 40. | Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? PLoS One. 2017;12:e0170581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 277] [Cited by in RCA: 323] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 41. | de Jong MJ, Boonen A, van der Meulen-de Jong AE, Romberg-Camps MJ, van Bodegraven AA, Mahmmod N, Markus T, Dijkstra G, Winkens B, van Tubergen A, Masclee A, Jonkers DM, Pierik MJ. Cost-effectiveness of Telemedicine-directed Specialized vs Standard Care for Patients With Inflammatory Bowel Diseases in a Randomized Trial. Clin Gastroenterol Hepatol. 2020;18:1744-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 42. | Yin AL, Hachuel D, Pollak JP, Scherl EJ, Estrin D. Digital Health Apps in the Clinical Care of Inflammatory Bowel Disease: Scoping Review. J Med Internet Res. 2019;21:e14630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 43. | Con D, De Cruz P. Mobile Phone Apps for Inflammatory Bowel Disease Self-Management: A Systematic Assessment of Content and Tools. JMIR Mhealth Uhealth. 2016;4:e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 44. | Solitano V, Alfarone L, D'Amico F, Peyrin-Biroulet L, Danese S. IBD goes home: from telemedicine to self-administered advanced therapies. Expert Opin Biol Ther. 2022;22:17-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 45. | Read AJ, Muza-Moons MM. Patient-focused IBD Applications Review. Gastroenterology. 2017;152:1241-1243. |
| 46. | Habashi P, Bouchard S, Nguyen GC. Transforming Access to Specialist Care for Inflammatory Bowel Disease: The PACE Telemedicine Program. J Can Assoc Gastroenterol. 2019;2:186-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 47. | Ehrlich O, Atreja A, Markus-Kennell S, Frederick K. P-50 CCFA GI Buddy Provides Patient Reported Outcomes and IBD Symptoms Evaluation. Inflamm Bowel Dis. 2012;18:S35-S36. [DOI] [Full Text] |
| 48. | Oshi Health. [cited 15 July 2022]. Available from: https://oshihealth.com. |
| 49. | de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, Cilissen M, van Bodegraven AA, Mahmmod N, Markus T, Hameeteman WM, Dijkstra G, Masclee AA, Boonen A, Winkens B, van Tubergen A, Jonkers DM, Pierik MJ. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 250] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 50. | Gupta A, Singh N, Madan D, Farooqui M, Singh M, Virmani S, Verma M, Bajaj A, Markandey M, Kante B, Vuyyuru SK, Kumar P, Sahu P, Makharia G, Kedia S, Ahuja V. P418 Development and validation of a digital health platform (IBD NutriCare) for telenutrition in patients with Inflammatory bowel disease. J Crohns Colitis. 2022;16:i407. [DOI] [Full Text] |
| 51. | Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff (Millwood). 2014;33:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 171] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 52. | Solimini R, Busardò FP, Gibelli F, Sirignano A, Ricci G. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 53. | Gentili A, Failla G, Melnyk A, Puleo V, Tanna GLD, Ricciardi W, Cascini F. The cost-effectiveness of digital health interventions: A systematic review of the literature. Front Public Health. 2022;10:787135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 141] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 54. | Rowan C, Hirten R. The future of telemedicine and wearable technology in IBD. Curr Opin Gastroenterol. 2022;38:373-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |