Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4692
Peer-review started: March 13, 2023
First decision: May 19, 2023
Revised: May 31, 2023
Accepted: June 14, 2023
Article in press: June 14, 2023
Published online: July 6, 2023
Processing time: 108 Days and 23.3 Hours
Morbihan disease is a rare skin condition with diagnostic and therapeutic challenges. Facial nonpitting erythematous edema is usually considered to be a characteristic manifestation and diagnostic clue for the Morbihan disease. Treatment of Morbihan disease remains a dilemma due to its long course, poor response, and high recurrence rate.
We report the case of a 69-year-old man with Morbihan disease. The patient presented ptosis as the first and main symptom. There was no obvious edema or other skin lesions. The patient was misdiagnosed with senile blepharoptosis based on eyelid performance and no treatment was administered to him. After continuous progressive asthenia of eye-opening and ptosis for more than one year, a skin biopsy was recommended. Histopathological analysis showed edema in the dermis, lymphatic hyperplasia and dilatation, and perivascular lym
Ptosis without obvious swelling could be the only or main clinical manifestation of Morbihan disease in rare conditions. An increase of mast cells was an important therapeutic clue to the rapid and remarkable efficiency of the combination therapy of minocycline and antihistamine.
Core Tip: Morbihan disease is a rare skin disease that is mainly characterized by nonpitting erythematous edema on the upper two-thirds of the face. We report an atypical case of progressive blepharoptosis without obvious edema, as a reminder of the existence of this uncommon condition to dermatologists, neurologists, and ophthalmologists to reduce chances of misdiagnosis. Usually long-term minocycline is used to treat Morbihan disease but has uncertain efficacy. We successfully treated our patient with a combination of minocycline and ketotifen. We also summarized previous reports on the use of minocycline in Morbihan disease and noted that mast cells might be key histological predictors of the treatment response to minocycline.
- Citation: Na J, Wu Y. Morbihan disease misdiagnosed as senile blepharoptosis and successfully treated with short-term minocycline and ketotifen: A case report. World J Clin Cases 2023; 11(19): 4692-4697
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4692.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4692
So far, less than 100 cases of Morbihan disease have been reported. The clinical manifestation of this rare disease has not been fully described. Based on the limited available reports, Morbihan disease classically occurs in middle-aged to elderly males, with chronic persistent nonpitting erythematous edema on the upper two-thirds of the face being the main diagnostic clue in most cases[1]. Ptosis has rarely been considered as a hint of Morbihan disease unless accompanied by extreme periocular swelling[2]. However, diagnosis is more difficult for the atypical cases without obvious edema. The treatment of Morbihan disease also remains controversial. Therapeutic strategies that include drugs, laser, and surgical techniques have been used for Morbihan disease but these often end in long courses and unsatisfactory efficacy[3]. More evidence is urgently needed for the diagnosis and treatment of this disease. Here, we report a special case of Morbihan disease with misleading ptosis and without obvious erythematous edema in a 69-year-old man who was successfully treated with short-term minocycline combined with ketotifen.
A 69-year-old man presented to our Department of Dermatology with progressive asthenia of eye-opening and ptosis for more than one year.
Ptosis for over one year was the only complaint that the patient presented. There were no obvious lesions on periocular skin or other areas of the face. The patient denied the existence of discomfort such as itching, swelling, or pain. He attended the Neurological Department and Ophthalmology Department frequently with no significant positive changes in his condition. Initial considerations of neurogenic and myogenic ptosis, for example, oculomotor paralysis, myasthenia gravis, and hyperthyroid ophthalmomyopathy, were excluded after a series of examinations including neuroelectromyography, neostigmine test, myasthenia gravis-related antibodies, thyroid function, and craniocerebral imaging. The patient was diagnosed with senile blepharoptosis, and he refused treatment. However, his ptosis aggravated so a skin biopsy was finally recommended.
The patient reported well-controlled diabetes and hypertension. He denied other systemic diseases or any history of dermatoses such as rosacea, acne, erysipelas, contact dermatitis, angioedema, and skin lupus erythematosus. The patient also denied preceding periocular rash, trauma, surgery, or self-conscious swelling.
The patient denied bad personal habits and genetic diseases in his family. However, he reported that his father had similar progressive ptosis but did not attend a hospital for diagnosis and treatment before his death.
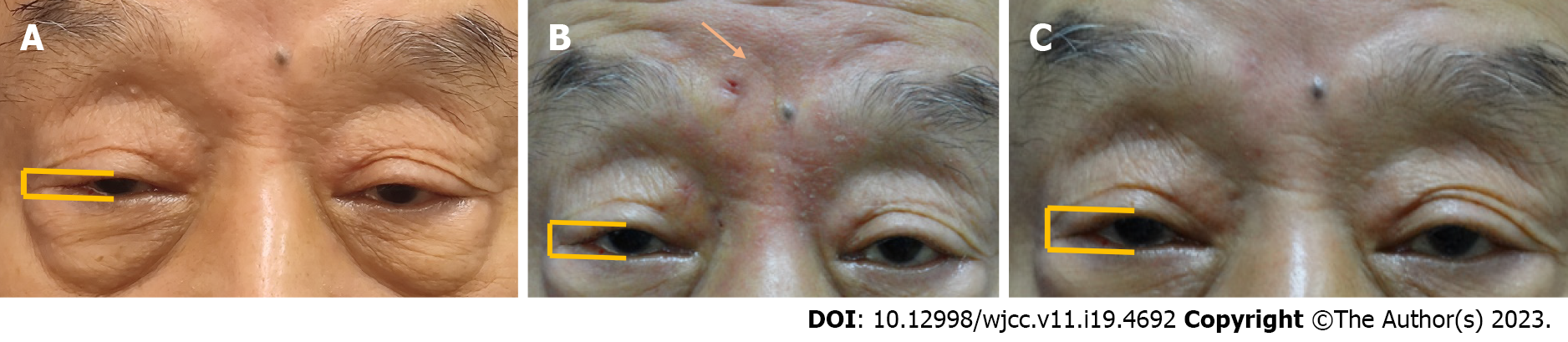
Upon physical examination, moderate bilateral blepharoptosis was observed without obvious edema, erythema, papules, or masses on his face (Figure 1A). Further careful examination of the periocular and upper facial skin led to the observation of shallow glabellar wrinkles and obvious infiltration by touch. It was important to note that erythematous lesions were inspired for the first time after the skin biopsy of the upper eyelid and forehead (Figure 1B).
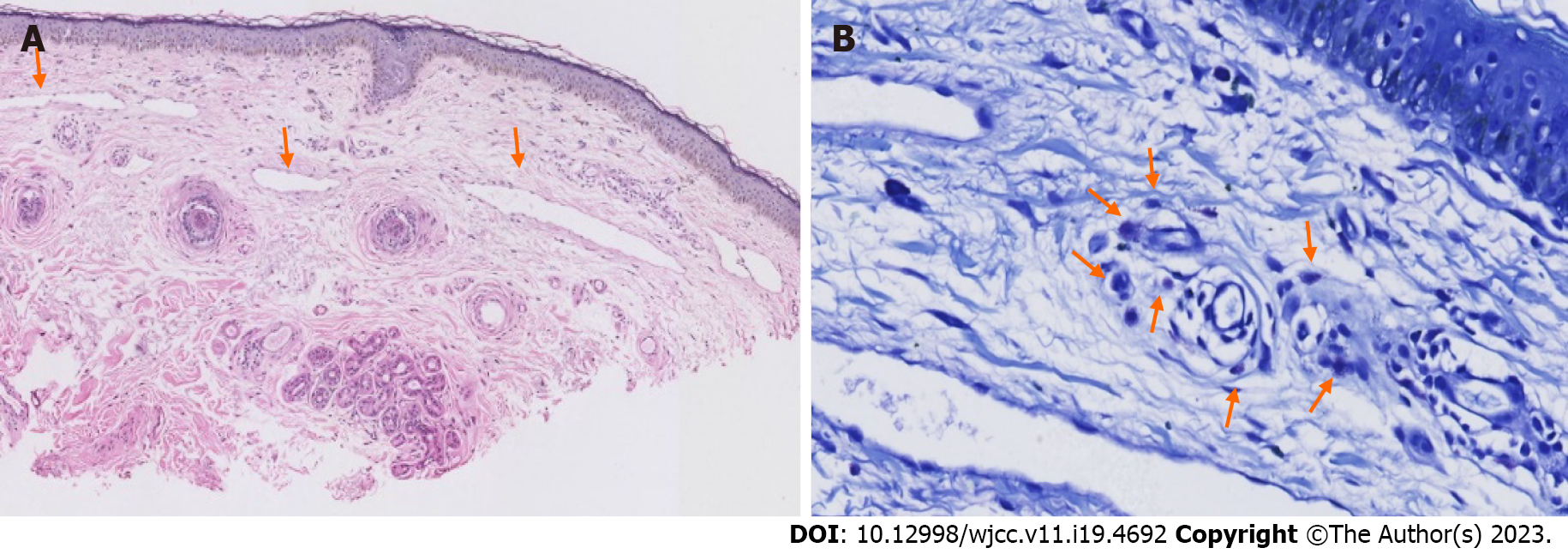
No abnormalities were observed after routine examination of the blood, liver and kidney function, and electrolyte levels. Antinuclear antibody, anti-DNA antibody, anti-ENA antibody, muscle enzymes, and immunoglobulin E (IgE) tests were all negative. There were no obvious abnormalities from neuroelectromyography, neostigmine test, myasthenia gravis-related antibodies, and thyroid function. Upper eyelid and forehead histopathological results showed manifestations such as edema in dermis, lymphatic hyperplasia and dilatation, as well as perivascular lymphocytic infiltration (Figure 2A). Toluidine blue-stained mast cells increased with a mean number of over five in each high-power field (Figure 2B).
There were no significant abnormalities in craniocerebral imaging.
By combining the typical pathological features with the less conspicuous skin manifestations, which included infiltration by touch, together with subsequent erythema and slight edema induced by biopsy, the patient was diagnosed with Morbihan disease. Given the less typical clinical appearance, differential diseases that could cause periorbital edema were considered, and these included blepharochalasis syndrome, angioedema, contact dermatitis, dermatomyositis, lupus erythematosus and Melkersson-Rosenthal Syndrome. However, the patient’s inconsistent history (e.g. onset age, persistent course, no allergen exposure, no wheals, normal muscle strength, no tongue fissures or facial nerve defects) and associated examinations (e.g. normal eosinophils, IgE, muscle enzymes, autoantibodies, unsupported pathological findings) eliminated the possibility of these differential diseases.
The patient was treated with a combination therapy of oral minocycline at 100 mg/d and oral ketotifen at 1 mg/d. His ptosis was rapidly relieved and forehead wrinkles also deepened seven days later (Figure 1B), accompanied by progressive gradual improvement in the condition, overall (Figure 1C).
Bilateral ptosis improved and the eyelids reassumed the pre-disease state. The administration of the drugs was stopped 40 days after the commencement of the treatment. No recurrence of the signs and symptoms was observed during a six-month follow-up period.
Morbihan disease, also known as rosacea lymphedema or solid persistent facial edema, is a rare entity and few cases have previously been reported. The precise diagnosis of Morbihan disease remains a challenge in clinical practice. Eyelids are most frequently involved, followed by the forehead, nose and cheeks[4]. Swelling can be found in almost all previous periocular Morbihan disease cases as the typical feature. There have been no reports of Morbihan disease with ptosis as the first or only manifestation. When ptosis exists without obvious edema, it is more likely to be overlooked and mislead ophthalmologists, neurologists and dermatologists to confused directions. Skin inflammation can also cause ptosis, which is attributed to transient dysfunction of aponeurosis or levator palpebrae. This dysfunction may be due to inflammatory cell infiltration or edema-induced mechanical weight increase[5]. The inflammatory ptosis should be considered as a diagnostic prompt in our atypical case. The histopathological features of Morbihan disease include dermal edema, lymphatic hyperplasia and dilatation, perivascular infiltration of lymphocytes, perifollicular fibrosis and occasionally perilymphatic or intralymphatic epithelioid cell granulomas[6]. The infiltration of increased mast cells was a histological feature in our patient. Activation of mast cells in Morbihan disease[7-9] can promote vasodilation, edema, and lymphocytic infiltration in the dermis. In addition, mast cells are a key mediator of cutaneous pathogenic fibrosis. These changes are associated with injury and obstruction of lymphatics, ultimately triggering dermal lymphedema and inflammatory ptosis when occurring in eyelids[10].
The treatment of Morbihan disease remains a dilemma with no recognized guidelines[11,12]. Corticosteroids, antihistamines, antibiotics, isotretinoin, and combination regimens have been used but these are long-term and are associated with unsatisfactory outcomes. Carbon dioxide laser blepharoplasty and surgical eyelid debulking[1,13] are other treatment options that are employed when drugs are ineffective. However, recurrence is common when these interventions are used, especially in patients with obvious inflammatory cell infiltration. Minocycline has been used in twelve patients with Morbihan disease in previous English language reports (Table 1), mainly as an oral monotherapy, but only six of twelve patients achieved significant improvement to variable extents. The histopathological features might guide and predict the therapeutic effects of various interventions. The positive effects of minocycline were associated with the presence of mast cells (4/6). The patients without mast cell infiltration failed in treatment with minocycline even at high doses or with long-term administration, except one patient who was infected with increased Demodex mites and was administered minocycline combined with topical metronidazole[14]. This suggested that mast cells might be a histological therapeutic clue for Morbihan disease. The anti-mast cell activities of minocycline indicate their significant role in the treatment of Morbihan disease[15]. Tetracycline can inhibit cytokine production of mast cells in vitro[8], and minocycline has been shown to inhibit IgE responses and mast cell mediated cutaneous edema[16]. However, treatment with minocycline often requires a long period of four to six months, which inevitably exposes the liver to toxicity issues. In our patient, a seven-day rapid response was observed, and a 40-d short course was achieved when minocycline was combined with ketotifen. Ketotifen is a strong mast cell stabilizer that is used in many allergic diseases. It can inhibit mast cell degranulation during the early stages of inflammation. It suppresses pathological edema and fibrosis by reducing the release of inflammatory factors IgE, tumor necrosis factor-α, interleukin (IL)-4, and IL-13[17,18]. The success of the combination therapy of minocycline and ketotifen in our patient may be a good option that reduces the duration of antibiotic administration, especially in the early stages of the disease.
| Sex/age (yr) | Clinical features | Mast cell | Dose | Course | Effect |
| M/51[10] | Erythema and edema on left upper eyelid with complete left ptosis | - | N/A | N/A | Ineffective |
| M/70[6] | Erythematous edema on forehead, nose and periorbital areas | - | 200 mg/d, 300 mg/d | Over 2 mo | Ineffective |
| M/54[12] | Erythema and edema on cheek and periorbital area | - | N/A | 6 to 7 mo | Ineffective |
| M/30[13] | Edema on bilateral eyelids | - | 100 mg/d, 50 mg/d | 7 mo | Discontinued due to insignificant improvement and abnormal liver enzyme levels |
| M/74[7] | Swelling on right cheek and left upper eyelid | + | 50 mg/d, 100 mg/d | 4 mo | Partially effective |
| F/64[15] | Swelling on entire face | + | 100 mg/d | 6 mo | Significantly effective |
| M/38[18] | Periorbital indurated edema | + | N/A | 3 mo | Ineffective |
| M/56[8] | Swelling on both eyelids and cheeks | + | 100 mg/d | 7 mo | Effective but discontinued due to abnormal liver enzyme levels |
| F/41[4] | Erythematous edema on upper eyelids, forehead, nose and cheeks | + | N/A | N/A | Effective |
| F/40[11] | Bilateral periorbital edema and intermittent blurry vision | - | N/A | A short period | Discontinued due to urticaria |
| N/A/88[1] | Swelling on left eyelid | N/A | N/A | N/A | Partially improved |
| M/28[14] | Edema and erythema on periorbital region, nose and cheeks; telangiectasias and pustules | - | 100 mg/d | Over 2 mo | Partially improved |
Morbihan disease with blepharoptosis as the only or main manifestation rather than facial edema has not been previously reported. This rare condition provided supplementary clinical manifestation and diagnostic clues of Morbihan disease for physicians in dermatology, neurology, and ophthalmology. There is no exact effective treatment strategy for Morbihan disease. However, histopathology is an important reference for the selection of treatment strategies. Based on literature review and the successful treatment of our patient, minocycline combined with antihistamines should be the prior treatment choice in Morbihan disease with increased mast cells.
We are very grateful to the patient for agreeing to publish of case details.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alkhatib AJ, Jordan; Emran TB, Bangladesh S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Yvon C, Mudhar HS, Fayers T, Siah WF, Malhotra R, Currie Z, Tan J, Rajak S. Morbihan Syndrome, a UK Case Series. Ophthalmic Plast Reconstr Surg. 2020;36:438-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Kim JE, Sim CY, Park AY, Hong SA, Park YL, Jang SY, Lee SY. Case Series of Morbihan Disease (Extreme Eyelid Oedema Associated with Rosacea): Diagnostic and Therapeutic Approaches. Ann Dermatol. 2019;31:196-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Kim JH. Treatment of Morbihan disease. Arch Craniofac Surg. 2021;22:131-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Ramirez-Bellver JL, Pérez-González YC, Chen KR, Díaz-Recuero JL, Requena L, Carlson JA, Llamas-Velasco M. Clinicopathological and Immunohistochemical Study of 14 Cases of Morbihan Disease: An Insight Into Its Pathogenesis. Am J Dermatopathol. 2019;41:701-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Koursh DM, Modjtahedi SP, Selva D, Leibovitch I. The blepharochalasis syndrome. Surv Ophthalmol. 2009;54:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Fujimoto N, Mitsuru M, Tanaka T. Successful treatment of Morbihan disease with long-term minocycline and its association with mast cell infiltration. Acta Derm Venereol. 2015;95:368-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Okubo A, Takahashi K, Akasaka T, Amano H. Four cases of Morbihan disease successfully treated with doxycycline. J Dermatol. 2017;44:713-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Ludgate M, Baker G. Unlocking the immunological mechanisms of orbital inflammation in thyroid eye disease. Clin Exp Immunol. 2002;127:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004;82:765-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Boparai RS, Levin AM, Lelli GJ Jr. Morbihan Disease Treatment: Two Case Reports and a Systematic Literature Review. Ophthalmic Plast Reconstr Surg. 2019;35:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Hu SW, Robinson M, Meehan SA, Cohen DE. Morbihan disease. Dermatol Online J. 2012;18:27. [PubMed] |
| 13. | Kou K, Chin K, Matsukura S, Sasaki T, Nozawa A, Aihara M, Kambara T. Morbihan disease and extrafacial lupus miliaris disseminatus faceie: a case report. Ann Saudi Med. 2014;34:351-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Rizzo A, Fiorani D, Lazzeri L, Taddeucci P, Rubegni P, Flori ML, Russo F. Usefulness of in vivo reflectance confocal microscopy in Morbihan syndrome. Skin Res Technol. 2021;27:974-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Kabuto M, Fujimoto N, Honda S, Tanaka T. Successful treatment with long-term use of minocycline for Morbihan disease showing mast cell infiltration: A second case report. J Dermatol. 2015;42:827-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Joks R, Durkin HG. Non-antibiotic properties of tetracyclines as anti-allergy and asthma drugs. Pharmacol Res. 2011;64:602-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Yuan W, Hou S, Jia H, Qiu Z, Liu T, Chen X, Li H, Sun Y, Liang L, Sui X, Zhao X, Zhao Z. Ketotifen fumarate attenuates feline gingivitis related with gingival microenvironment modulation. Int Immunopharmacol. 2018;65:159-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Rebellato PR, Rezende CM, Battaglin ER, Lima BZ, Fillus Neto J. Syndrome in question. An Bras Dermatol. 2015;90:909-911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |